Translate this page into:
Langerhans cell histiocytosis with widespread ulcers and masses on the palate
2 State Key Laboratory of Oral Diseases, West China Hospital of Stomatology, Sichuan University, Chengdu, Sichuan; College of Stomatology, Chongqing Medical University; Chongqing Key Laboratory of Oral Diseases and Biomedical Sciences, Chongqing, China
Correspondence Address:
Xin Jin
College of Stomatology, Chongqing Medical University, 426, SongShiBeiLu, Chongqing
China
Xin Zeng
State Key Laboratory of Oral Diseases, West China Hospital of Stomatology, Sichuan University, 14, RenMinNanLu, Section - 3, Chengdu, Sichuan - 610 041
China
| How to cite this article: Liu J, Liu D, Zhou Y, Chen Q, Zeng X, Jin X. Langerhans cell histiocytosis with widespread ulcers and masses on the palate . Indian J Dermatol Venereol Leprol 2014;80:462-463 |
Sir,
Langerhans cell histiocytosis (LCH) is a rare disease characterized by abnormal proliferation of Langerhans cells in various organs. The etiopathogenesis of LCH is unknown. [1] It can present with both local and systemic manifestations involving bone, skin and mucosal tissue, and can also involve internal organs. LCH was previously classified into three clinical forms: Letterer-Siwe disease (subacute or acute disseminated form), Hand-Schüller-Christian disease (disseminated chronic form) and eosinophilic granuloma (localized chronic form). [2] Oral lesions may be the first sign of LCH, and sometimes the oral cavity may be the only area affected. [2],[3] In this report, we describe a case of LCH with widespread ulcers and masses on the palate as the earliest clinical features.
A 21-month-old girl presented to our clinic with an ulcerated palate for 1 month. She did not have any fever or hypothermia, reduced intake of food or disturbed sleep. The lesions first appeared as pustules. An incision and drainage was performed at a local hospital. Her parents sought a second opinion as the ulcers showed no sign of healing. The ulcer was found to have enlarged in size and almost the entire palate was involved. She was otherwise healthy and her parents denied any history of oral trauma, insect bites, allergies, or systemic diseases.
Oral examination revealed widespread ulcers and masses on the palate and maxillary palatal gingiva without detectable teeth mobility and lymphadenopathy [Figure - 1]. There was no cutaneous involvement. No systemic lesions were detected by physical examination, chest and skull radiographs. Maxillofacial cone-beam computed tomography (CBCT) showed bony destruction of the left orbital plate and maxilla in a pattern suggestive of Langerhans cell histiocytosis. Hematoxylin and eosin staining of the palatal biopsy performed in our hospital revealed a diffuse infiltrate of round and oval cells with kidney-shaped nuclei. Immunohistochemical studies of the specimen showed positive staining with CD1a, S100 and langerin, supporting the diagnosis of Langerhans cell histiocytosis [Figure - 2]a-e.
 |
| Figure 1: Widespread swelling and masses were detected on the palate and maxillary palatal gingiva |
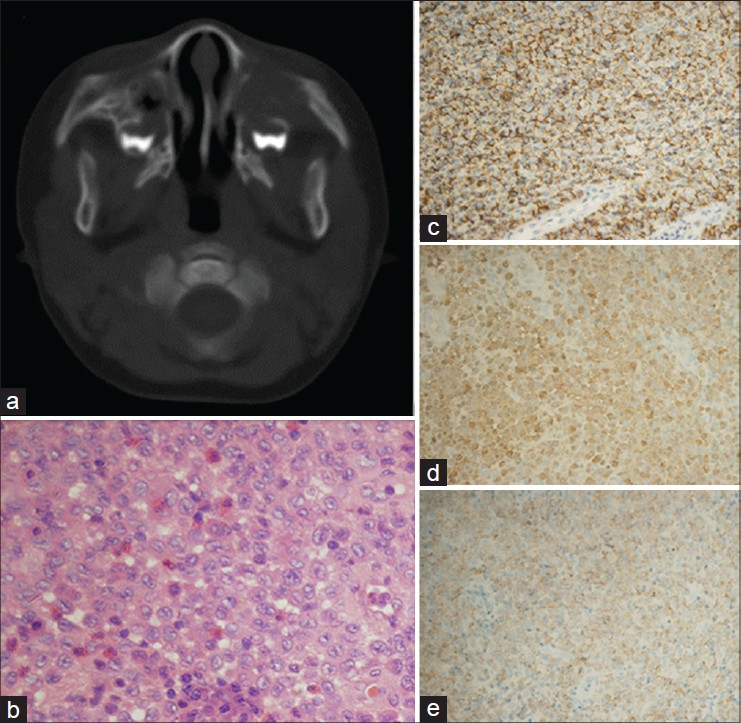 |
| Figure 2: (a) Bone destruction of left orbital plate and maxilla. (b) A diffuse infiltration of round or oval cells, with kidneyshaped nuclei (hematoxylin and eosin, ×200 magnification). (c-e) CDla-positive, S-100-positive and langerin-positive cells (×100 magnification) |
She was transferred to the hematology department immediately. The ulcers healed and masses in the palate gradually resolved after chemotherapy with vincristine, 0.9 mg, once a week, intravenously and prednisone 12.5 mg, twice a day, orally for 4 months [Figure - 3].
 |
| Figure 3: Ulcers and masses gradually normalized after chemotherapy |
Widespread ulcers and masses on the palate as the earliest clinical sign of Langerhans cell histiocytosis is a presentation rarely reported previously. Oral lesions may be the first or only sign of the disease but they usually manifest as swelling or ulceration overlying destructive lesions of the jawbone. [4] The inflammatory or ulcerative lesions may be mistaken for another disease and delay diagnosis of Langerhans cell histiocytosis which may then progress to an aggressive life-threatening multiorgan disease. [5] Furthermore, it is considered that the younger the patient, worse the prognosis. Therefore, the possibility of the diagnosis of Langerhans cell histiocytosis should be considered, especially in young children with gingival swellings and mobility of teeth. Additionally, histological diagnosis is often complicated by a nonspecific inflammatory reaction. The diagnosis depends on clinical, histopathological and radiographic examination and should be confirmed by immunohistochemical study with CD1a, S100 protein and langerin, three markers used widely for identifying Langerhans cells.
| 1. |
Jalil Ab, Hin-Lau S. Oral Langerhans cell histiocytosis in Malaysian children: A 40-year experience. Int J Paediatr Dent 2009;19:349-53.
[Google Scholar]
|
| 2. |
Madrigal-Martinez-Pereda C, Guerrero-Rodriguez V, Guisado-Moya B, Meniz-Garcia C. Langerhans cell histiocytosis: Literature review and descriptive analysis of oral manifestations. Med Oral Patol Oral Cir Bucal 2009;14:E222-8.
[Google Scholar]
|
| 3. |
Shirley JC, Thornton JB. Oral manifestations of langerhans' cell histiocytosis: Review and report of case. ASDC J Dent Child 2000;67:293-6.
[Google Scholar]
|
| 4. |
Cleveland DB, Goldberg KM, Greenspan JS, Seitz TE, Miller AS. Langerhans' cell histiocytosis: Report of three cases with unusual oral soft tissue involvement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;82:541-8.
[Google Scholar]
|
| 5. |
Fistarol S, Itin P, Häusermann P, Oberholzer M, Raineri I, Lambrecht T, et al. Unifocal Langerhans cell histiocytosis of the oral mucosa. J Dtsch Dermatol Ges 2009;7:620-2.
[Google Scholar]
|
Fulltext Views
3,664
PDF downloads
2,019





