Translate this page into:
Laser and light based treatments of acne
Correspondence Address:
Reena Rai
Department of Dermatology, PSG Institute of Medical Science and Research, Coimbatore - 641 004
India
| How to cite this article: Rai R, Natarajan K. Laser and light based treatments of acne. Indian J Dermatol Venereol Leprol 2013;79:300-309 |
Abstract
Medical treatments for acne vulgaris include a variety of topical and oral medications. Poor compliance, lack of durable remission, and potential side effects are common drawbacks to these treatments. Therefore, there is a growing demand for a fast, safe, and side-effect-free novel therapy. Acne often improves after exposure to sunlight, and this has led to the development of laser and other light therapies resulting in the overall ease of treatment, with minimal adverse effects. A variety of light and laser devices has been used for the treatment of acne, including the potassium titanyl phosphate laser, the 585- and 595-nm pulsed dye lasers, the 1450-nm diode laser, radiofrequency devices, intense pulsed light sources, and photodynamic therapy using 5-aminolevulinic acid and indocyanine green. These devices are thought to target the underlying pathogenic factors such as propionibacterium acnes colonization, increased sebaceous gland activity, and the cutaneous inflammatory response. In this article, we review the current status of light- and laser-based treatment of acne.Introduction
Acne vulgaris is a multifactorial skin disorder of pilosebaceous unit significantly associated with psycho-social comorbidites. Acne is treated with a variety of topical and oral medications such as antibacterials, antimicrobials and retinoids. Conventional treatments for acne can be prolonged and associated with side-effects. This has prompted a search for more acceptable therapies. Acne often improves after exposure to sunlight, and this observation has led to the development of laser and other light therapies over two decades, laser and light sources are given in combination with oral and topical treatments or as an alternate regimen. Till date, the trials of lasers and light therapy have been small and the results conflicting. However′ in this article we discuss the recent updates regarding the use of lasers and light therapy in treating acne vulgaris.
Pathogenesis of Acne
Acne is a chronic inflammatory disease of pilosebaceous units and the major factors involved in the pathogenesis are increased sebum production, hypercornification of the pilosebaceous duct, abnormality of the microbial flora, especially ductal colonization with Propionibacterium acnes (P. acnes) and inflammation. Recent molecular and clinical studies have advanced knowledge in areas such as sebocyte biology, [1] the role of androgens, [2] hyperkeratinization, [3] dietary factors, [4] and the effect of cytokines and toll-like receptors, [5] leading to the identification of potential new targets for acne therapy.
Treatment with Laser and Light-Based Therapies
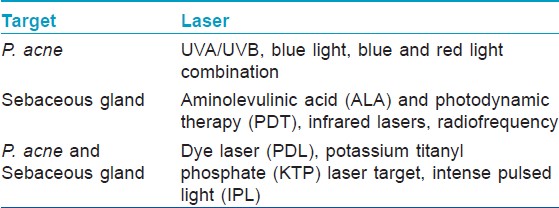
Lasers/light-based devices may offer an alternative to conventional acne modalities in selected patients, such as non-responder or noncompliant patients or in antibiotic resistance patients. Over almost a century, many types of light sources were introduced to treat or improve acne symptoms. These light sources include fluorescent, halogen, xenon, tungsten lamps, and recently lasers. The devices used to treat acne may be separated into groups based on approach; namely devices that directly or indirectly target P. acnes are UVA/UVB, blue light, blue and red light combination, devices that alter the sebaceous gland structure include aminolevulinic acid (ALA) and photodynamic therapy (PDT), infrared lasers, radiofrequency, and devices that exert an effect on both are pulse dye laser (PDL), potassium titanyl phosphate (KTP) laser target, intense pulsed light (IPL) [6] [Table - 1].
Targeting P. Acnes
P. acnes which is implicated in the pathogenesis of acne is a gram positive microaerophilic skin bacterium. As a part of its normal metabolic and reproductive processes, it produces and accumulates endogenous porphyrins, namely protoporphyrin, uroporphyrin, and coproporphyrin III. [7] These porphyrins absorb light energy at the near-ultraviolet (UV) and blue light spectrum. Exposure to absorbed light wavelengths induces these photosensitizers to generate highly reactive free radical species, which subsequently cause bacterial destruction. [8],[9] The singlet oxygen formed in the reaction is a potent oxidizer that destroys lipids in the cell wall of P. acnes. [10] Although absorption and photodynamic excitation are most efficient between the wavelengths of 400 and 430 nm, with enough light, the reaction may be initiated with a variety of different wavelengths. Many light sources may affect P. acnes including narrowband light sources, IPL devices (broadband light), KTP lasers (532 nm), PDLs (585-595 nm), and various orange/red light lasers or light sources (610-635 nm); as these light sources have wavelengths that correspond to an absorption peak of P. acnes porphyrins.
UVA/UVB
70% of patients report improvement in their acne after sunlight exposure, [11] but it was not clear until recently which wavelengths contribute to this favorable effect, UV, visible light, or the combination of both. UVA and UVB treatment was found to have a marginal beneficial effect, but it is potentially carcinogenic. [12]
Blue Light and Red Light
Blue light has the most effective visible wavelength for photoactivation of endogenous porphyrin component of P. acnes because the 407- to 420-nm band has the strongest porphyrin photoexcitation coefficient.
However, blue light has poor depth of skin penetration. [10] Red light, however, in addition to its deeper penetration up to the sebaceous glands, [13] may have anti-inflammatory properties by influencing cytokine release from macrophages. [14] Research has shown in vitro that the viability of P. acnes relates inversely to light intensity. According to an action spectrum for the inactivation of P. acnes, the sensitivity of P. acnes is highest for shorter wavelengths and decreases with increasing wavelength. [15]
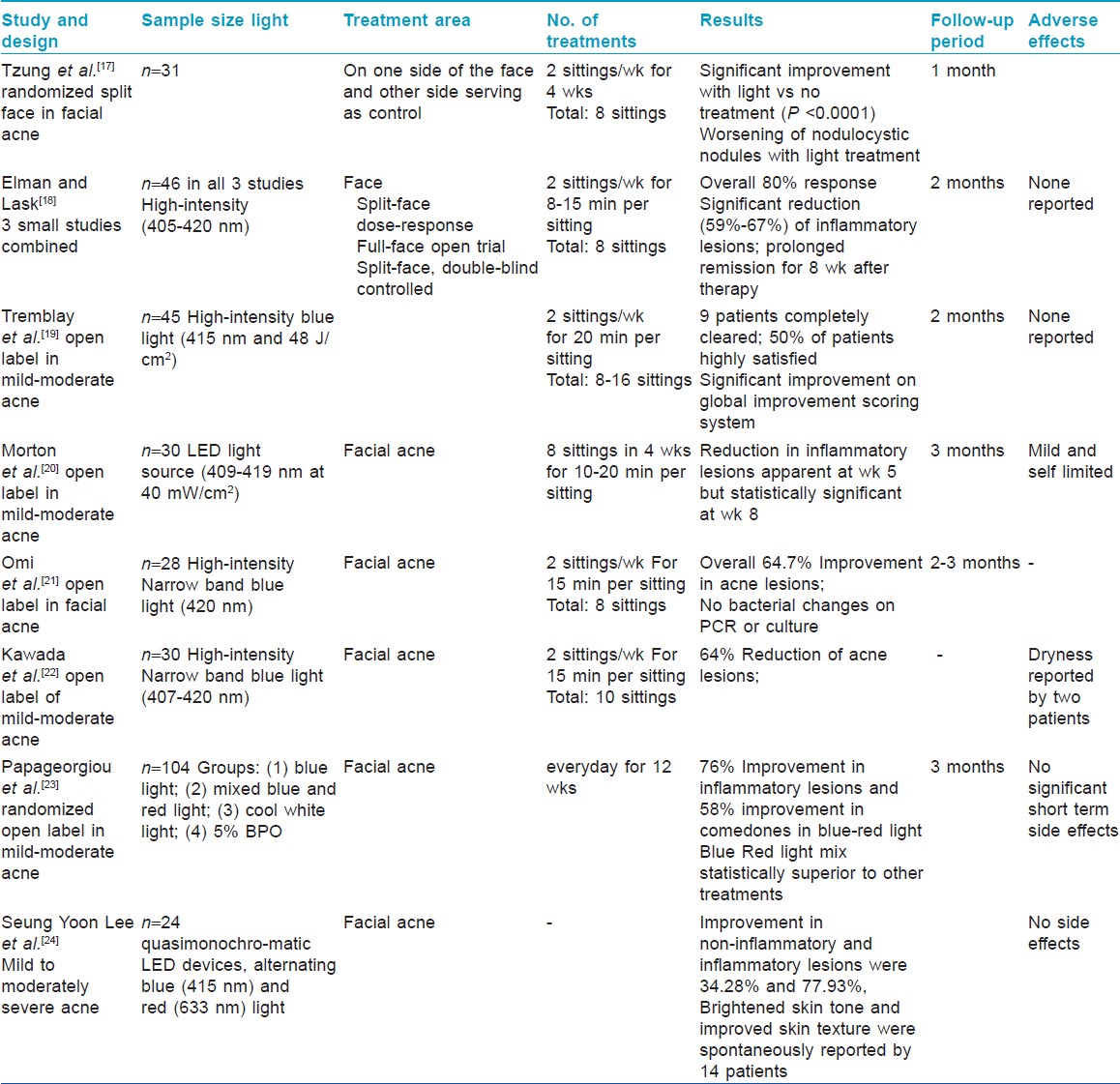
There are several studies showing the efficacy of blue light, and combination of both blue and red light for the treatment of mild to moderate acne [Table - 2]. Most of the studies were open label with sample size ranging between 30 to 50 patients. The results uniformly showed short term improvement in inflammatory lesions with blue light. Further none of the studies has showed follow up results beyond 12 weeks after treatment. Acne clearing is variable among patients and relapse rates are high after therapy is discontinued. [16],[17],[18],[19],[20],[21],[22],[23],[24] We have quoted two studies of combination of blue-red light therapy and one of them show that combination is superior to blue light alone [Table - 2].
Lasers:
KTP
The 532 nm green light pulsed laser therapy has been tried as it penetrates deeper than blue light and activates porphyrins to target P. acnes. It is well tolerated and causes non-specific collateral thermal injury to sebaceous glands. KTP has been shown to have short-term effects on improving acne severity with minimal side effects, Baugh et al., [25] in a trial evaluated twenty-six subjects, with moderate facial acne. They concluded that use of the KTP 532 nm laser for the treatment and management of acne vulgaris is both safe and effective, with positive results enduring up to four weeks post-treatment.
Another prospective split-face study involving 11 patients using KTP laser by Bowes et al., showed a 36% decrease in mild-to-moderate acne lesion count versus a 2% increase in the control group after 1 month. A 28% decrease in sebum production but minimal effect on P. acnes (measured by fluorescent photography) was also noted. [26]
Another study by Yilmaz et al., [27] to evaluate the efficacy and safety of 532-nm KTP laser and compare the effects of once and twice weekly applications in the treatment of mild to moderate acne vulgaris was conducted on 38 patients They concluded that 532-nm KTP laser treatment may be an alternative method in selected acne vulgaris patients with no significant difference noted between once and twice weekly applications.
PDL
585-nm PDL that targets oxyhemoglobin has also been investigated for treatment of acne. It causes selective photothermolysis of the dilated vascular component of inflammation associated with acne. Through the delivery of coherent yellow light, porphyrins are activated to produce phototoxic effects.
Seaton et al., [28 ] demonstrated a 49% reduction in inflammatory lesion counts versus 10% in controls 12 weeks after treatment using a 585 nm PD. Compared to controls, almost half of the treated patients (regardless of severity at baseline) had a 50% reduction in lesion counts by 12 weeks. In a randomized blinded placebo-controlled trial of 26 patients with mild-to moderate acne, Orringer et al., [29] showed only a trend towards improvement with the laser treated side that was not statistically significant.
Another study by Seaton et al., [30] with pulsed dye laser showed no effect on the degree of P. acnes colonization or sebum production as measured by the standardized application of absorptive tape. This study found a significant upregulation of transforming growth factor β, which are a potent stimulator of neocollagenesis and a potent inhibitor of inflammation. Thus, the efficacy of this laser on inflammatory acne is likely through its local anti-inflammatory effects.
The 595-nm pulsed dye laser has also been used in conjunction with the 1450-nm diode laser to treat both acne vulgaris and post-inflammatory erythema resulting from acne. In one non controlled study by Glaich et al., [31] of 15 patients the lesions counts dropped by a mean of 52%, 63%, and 84% after 1, 2, and 3 treatments, respectively ( P < 0.01). In addition to improvements in acne and acne scarring, significant improvement in post-inflammatory erythema was also noted and was attributed to the selective photothermolysis of vessels by the pulsed dye laser. Although the combination of the two lasers may provide better targeting of different pathophysiologic contributors to acne, the authors did not know whether the improvement is greater than that achieved with either the pulsed dye laser or the 1450-nm diode laser alone.
A randomized controlled single-blinded trial was conducted to assess the efficacy of an adjuvant PDL treatment when combined with a proven topical treatment [fixed-combination clindamycin 1%-benzoyl peroxide 5% hydrating gel) in 80 patients. The findings did not support the concept of a substantial benefit of PDL treatment in acne vulgaris. [32]
At low, nonpurpuric fluences, this laser can also reduce inflammatory acne. The effect of this laser on acne improvement was believed to be mediated by decreasing P. acnes or sebaceous gland activity. Although studies suggest promise, conclusions are not possible because of the varying regimens and methodologies used.
Targeting Sebaceous Glands:
Sebum plays an important role in acne, therapies targeting the gland with the goal of reduction in size and sebum output has resulted in acne improvement.
Infrared Lasers
Infrared lasers were developed for non-ablative facial skin rejuvenation; they have become one of the most effective, novel acne treatments available due to their depth of penetration into the dermis. Although the distribution of sebaceous glands is highly variable in the dermis, infrared lasers target water, which is the dominant chromosphere in the sebaceous gland. The laser light selectively produces an injury zone in the dermal layer where sebaceous glands are located and causes enough injury to arrest the over production of sebum, thereby eliminating acne. [10] The lasers at 1,450 nm and 1,540 nm have been used for this purpose.
1450-Nm Diode Laser
This device can cause thermal coagulation of the sebaceous lobule and associated hair follicle through peak thermal heating of the upper to mid dermis up to a depth of 500 μm. [13] The presumed mechanism of acne improvement is through heating of the sebaceous gland and associated structures resulting in reduced sebaceous gland activity resulting in a reduction in inflammatory acne lesions. Treatment with the infrared 1450-nm diode laser with a dynamic cooling device has been shown to safely and effectively reduce inflammatory acne lesions of the face with fluences as high as 14 J/cm 2 . The first report of the efficacy of this laser in the treatment of acne was an uncontrolled pilot study where 19 patients with inflammatory acne, many of whom were refractory to traditional medical treatment, underwent three treatments at four to six week intervals using a fluence of 14 J/cm 2 . The decrease in lesion counts from baseline was 37% after the first treatment, 58% after the second treatment, and 83% after the third treatment. Pain was well tolerated, and adverse effects were limited to transient erythema and edema at treatment sites. [33]
A subsequent study on 20 patients was done to evaluate long-term improvement in inflammatory acne after cessation of laser treatments. A reduction of 76.1% from baseline was sustained 12 months after the third and final laser treatment which helped demonstrate that the 1450-nm diode laser provides a long-term remission in acne, sebum production, as measured by Sebutape scores corroborating the hypothesis that the mechanism of this laser involves reduced sebaceous gland activity. [34]
1540-Nm Erbium Glass Laser
A single study has also shown efficacy of the 1540-nm erbium glass laser for treatment of acne. After four treatments at four-week intervals, a 78% reduction in acne lesions and decreased skin oiliness was noted in 25 patients. [35]
Similar results (82% decreased lesion count at three months) were reported by Kassir et al., [ 36] in 20 patients (skin phototypes I-IV) with facial acne who received four bi-weekly treatments. Patients in both trials reported decreased oiliness of the skin and no immediate or delayed adverse effects were reported in either study.
Another study by Angel et al., [37] was performed to investigate the effects of this laser on active lesions of the face and of the back at the two-year follow-up. The mean percent reduction was 71% at the six-month follow-up, 79% at the one-year follow-up and 73% at the two-year follow-up. Furthermore, this longer follow-up study demonstrates long-term acne clearing.
A study by Bogle et al., [38] was performed on 15 patients with moderate to severe acne with 1,540- on the face four times at 2-week intervals. Treatment of inflammatory facial acne with this laser showed improvement of 68%, but sebum measurements did not change.
Intense Pulsed Light
Unlike a laser, an intense pulsed light source provide a noncoherent (500 to 1200 nm) source of intense light that can be modified by filters to provide irradiation with specific wavelengths of light. The use of intense pulsed light for the treatment of acne has been theoretically based on the production of singlet oxygen after photoactivation of porphyrins synthesized and stored by P. acnes. [39] Broad spectrum delivery by IPL devices is believed to lead to photothermolysis, where the absorption of light by endogenous chromophores in the skin creates enough heat and energy to target the blood vessels that supply sebaceous glands in order to reduce sebum production. Several studies have utilized intense pulse light sources after topical application of porphyrins. In one study of intense pulsed light, patients with mild to moderate acne were treated using wavelengths between 430 and 1100 nm. Reductions of 79% and 74% were noted in non-inflammatory and inflammatory lesions, respectively, one month after the final treatment. [40]
Current studies using IPL as an anti-acne therapy have led to mixed results. Kanwna et al., [41] evaluated the efficacy and safety of IPL on acne vulgaris in Asian skin in 25 patients. He showed short-term improvement in both inflammatory and non-inflammatory acne lesions using IPL alone. After the first exposure, numbers of non-inflammatory and inflammatory acne lesions decreased to 36.6 and 43.0%, respectively, of their pretreatment values. After five treatments, they decreased to 12.9 and 11.7%, respectively, of their pretreatment values. Others have shown that IPL alone and IPL with photodynamic therapy significantly reduced the number of non-inflammatory, but not inflammatory lesions. [42] In comparison with other light sources, IPL was less effective at reducing acne lesions than pulsed dye lasers but more effective than blue-red combination light-emitting diodes. [43] With the adverse effects of pain, swelling, erythema, blistering, and crusting [39] and its doubtful efficacy it is unclear of the usefulness of IPL in future of acne therapy.
Radiofrequency
Reductions in perifollicular inflammation and sebaceous gland is the presumed mechanism of action A combined radiofrequency and pulsed light has been used to treat acne. Twice-weekly treatments for four weeks resulted in reduction of mean acne lesion counts by 47% in 32 patients. [44] Adverse effects were limited to temporary erythema, tingling and burning. Another study of 22 patients using a monopolar radiofrequency device showed greater than 75% reduction in inflammatory acne lesions in more than 90% of patients after one treatment session. [45]
Photodynamic Therapy
PDT involves the application of ALA, which, when taken up by the pilosebaceous units, is metabolized through the heme synthesis pathway to produce protoporphyrin IX which when photoactivated, the resultant singlet oxygen and free radicals produced are cytotoxic. This results in not only death of P. acnes but also damage to the pilosebaceous unit itself. [13],[46],[47],[48]
PDT requires 3 factors, a photosensitiser, light and oxygen. The commonly used photosensitizers are 5-aminolevulinic acid or, methylaminolevilunate (MAL) and the newer ones are Indocyanine green (ICG) and Indole-3-acetic acid. Sources of light used are light emitting diodes, fluorescent lamps, IPL (filtered xenon flashlamps) filtered incandescent or arc lamps, lasers and sunlight. There are certain variables that influence P. acnes photo inactivation which include concentration of porphyrins, (depending on type of acne lesion), effective fluence, wavelength of emitted photons, temperature at which the reaction is carried out and tissue oxygen availability. [49]
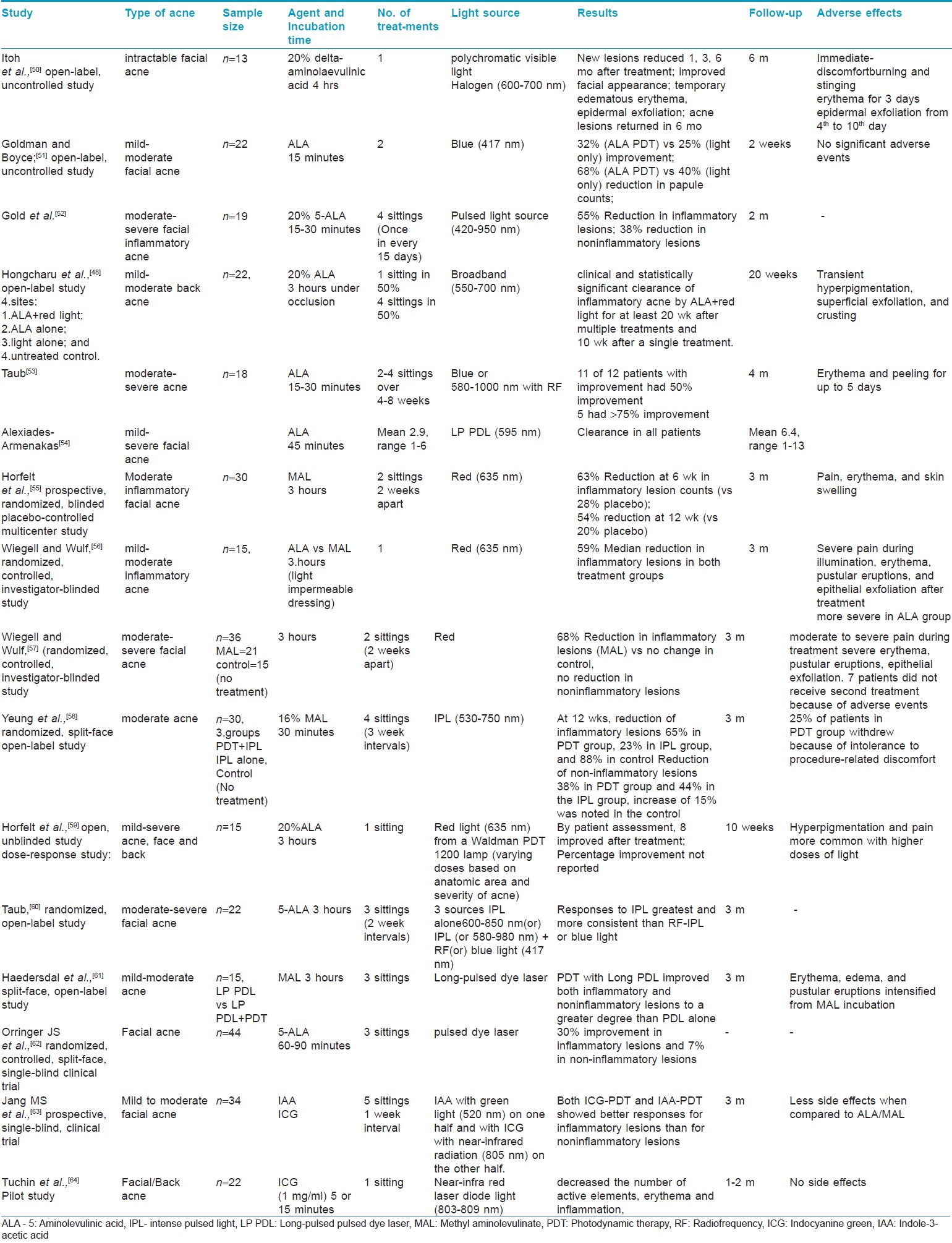
Various studies have been conducted using PDL with ALA, MAL and ICG. [48],[50],[51],[52],[53],[54],[55],[56],[57],[58],[59],[60],[61],[62],[63],[64] [Table - 3] Most of the studies and their data are short term and data limited. More controlled trials are required to rationalize the results.However the data below shows that inflammatory lesions respond better to the various light sources of PDT in cases of mild to moderate acne.
Conclusions
Laser and light-based acne treatments can be an alternative to medical treatment for non responders and is associated with minimal adverse effects. These devices also offer an option for those patients who have moderate to severe acne but are concerned about oral medications because of potential adverse effects. Long-term improvements have been documented with laser treatments. However, low powered visible light sources alone achieve mild acne improvement but the patient might be able to use the light in combination with a topical medication, thus avoiding the need for an oral antibiotic. The acne clearance produced by devices targeting P. acnes is generally short-lived and requires continued follow-up treatments. Devices that target sebaceous glands are all effective to varying degrees based upon the principle of selective damage to the sebaceous gland. And though this temporary alteration may be sufficient to decrease sebum production and result in long-term acne clearance, studies have yet to demonstrate sebaceous gland ablation. More clinical studies are needed to determine its efficacy and safety in different acne symptoms in a larger set of patients and in longer follow-up periods. Future advances in laser technology may improve both the efficacy and safety of lasers for the treatment of acne vulgaris and will make laser and light based treatments an attractive and cost-effective option for patients with acne.
| 1. |
Bohm M. Neuroendocrine regulators: Novel trends in sebaceous gland research with future perspectives for the treatment of acne and related disorders. Dermatoendocrinol 2009;1:136-40.
[Google Scholar]
|
| 2. |
Chen W, Tsai SJ, Sheu HM, Tsai JC, Zouboulis CC. Testosterone synthesized in cultured human SZ95 sebocytes derives mainly from dehydroepiandrosterone. Exp Dermatol 2010;19:470-2.
[Google Scholar]
|
| 3. |
Melnik BC. Role of FGFR2-signaling in the pathogenesis of acne. Dermatoendocrinol 2009;1:141-56.
[Google Scholar]
|
| 4. |
Danby FW. Nutrition and acne. Clin Dermatol 2010;28:598-604.
[Google Scholar]
|
| 5. |
Tenaud I, Khammari A, Dreno B. In vitro modulation of TLR-2, CD1d and IL-10 by adapalene on normal human skin and acne inflammatory lesions. Exp Dermatol 2007;16:500-6.
[Google Scholar]
|
| 6. |
Mariwalla K, Rohrer TE. Use of lasers and light-based therapies for treatment of acne vulgaris. Lasers Surg Med 2005;37:333-42.
[Google Scholar]
|
| 7. |
Ashkenazi H, Malik Z, Harth Y, Nitzan Y. Eradication of Propionibacterium acnes by its endogenic porphyrins after illumination with high intensity blue light. FEMS Immunol Med Microbiol 2003;35:17-24.
[Google Scholar]
|
| 8. |
Kjeldstad B. Photoinactivation of Propionibacterium acnes by near-ultraviolet light. Z Naturforsch [C] 1984;39:300-2.
[Google Scholar]
|
| 9. |
Melo TB. Uptake of protoporphyrin and violet light photodestruction of Propionibacterium acnes. Z Naturforsch [C] 1987;42:123-8.
[Google Scholar]
|
| 10. |
Elman M, Lebzelter J. Light therapy in the treatment of acne vulgaris. Dermatol Surg 2004;30:139-46.
[Google Scholar]
|
| 11. |
Charakida A, Seaton ED, Charakida M, Mouser P, Avgerinos A, Chu AC. Phototherapy in the treatment of acne vulgaris: What is its role? Am J Clin Dermatol 2004;5:211-6.
[Google Scholar]
|
| 12. |
Van Weelden H, de Gruihl FR, van der Putte SC, Toonstra J, Leun JC. The carcinogenic risks of modern tanning equipment: Is UV-A safer than UV-B? Arch Dermatol Res 1988;280:300-7.
[Google Scholar]
|
| 13. |
Ross EV. Optical treatments for acne. Dermatol Ther 2005;18:253-66
[Google Scholar]
|
| 14. |
Young S, Bolton P, Dyson M, Harvey W, Diamantopoulos, C. Macrophage responsiveness to light therapy. Lasers Surg Med 1989;9:497-505.
[Google Scholar]
|
| 15. |
Kjeldstad B. Different photoinactivation mechanisms in Propioni-bacterium acnes for near-ultraviolet and visible light. Photochem Photobiol 1987;46:363-6.
[Google Scholar]
|
| 16. |
Elman M, Lebzelter J. Light therapy in the treatment of acne vulgaris. Dermatol Surg 2004;30:139-46.
[Google Scholar]
|
| 17. |
Tzung TY, Wu KH, Huang ML. Blue light phototherapy in the treatment of acne. Photodermatol Photoimmunol Photomed 2004;20:266-9.
[Google Scholar]
|
| 18. |
Elman M, Slatkine M, Harth Y. The effective treatment of acne vulgaris by a high-intensity, narrow band 405-420 nm light source. J Cosmet Laser Ther 2003;5:111-7.
[Google Scholar]
|
| 19. |
Tremblay JF, Sire DJ, Lowe NJ, Moy RL. Light-emitting diode 415 nm in the treatment of inflammatory acne: An open-label, multicentric, pilot investigation. Cosmet Laser Ther 2006;8.31-3.
[Google Scholar]
|
| 20. |
Morton CA, Scholefield RD, Whitehurst C, Birch J. An open study to determine the efficacy of blue light in the treatment of mild to moderate acne. J Dermatol Treat 2005;16:219-23.
[Google Scholar]
|
| 21. |
Omi T, Bjerring P, Sato S, Kawana S, Hankins RW, Honda M. 420 nm Intense continuous light therapy for acne. J Cosmet Laser Ther 2004;6:156-62.
[Google Scholar]
|
| 22. |
Kawada A, Aragane Y, Kameyama H, Sangen Y, Tezuka T. Acne phototherapy with a high-intensity, enhanced, narrow-band, blue light source: An open study and in vitro investigation. J Dermatol Sci 2002;30:129-35.
[Google Scholar]
|
| 23. |
Papageorgiou P, Katsambas A, Chu A. Phototherapy with blue (415 nm) and red (660 nm) light in the treatment of acne vulgaris. Br J Dermatol 2000;142:973-8.
[Google Scholar]
|
| 24. |
Lee SY, You CE, Park MY. Blue and Red Light Combination LED Phototherapy for Acne Vulgaris in Patients with Skin Phototype IV. Lasers Surg Med 2007;39:180-8.
[Google Scholar]
|
| 25. |
Baugh WP, Kucaba WD. Nonablative phototherapy for acne vulgaris using the KTP 532 nm laser. Dermatol Surg 2005;31:1290-6.
[Google Scholar]
|
| 26. |
Bowes LE, Manstein D, Anderson RR. Effects of 532 nm KTP laser exposure on acne and sebaceous glands. Lasers Surg Med 2003;18:S6-7.
[Google Scholar]
|
| 27. |
Yilmaz O, Senturk N, Yuksel EP, Aydin F, Ozden, Canturk T, et al. Evaluation of 532-nm KTP laser treatment efficacy on acne vulgaris with once and twice weekly applications. J Cosmet Laser Ther 2011;13:303-7.
[Google Scholar]
|
| 28. |
Seaton ED, Charakida A, Mouser PE, Grace I, Clement RM, Chu AC. Pulsed-dye laser treatment for inflammatory acne vulgaris: Randomised controlled trial. Lancet 2003;362:1347-52.
[Google Scholar]
|
| 29. |
Orringer JS, Kang S, Hamilton T, Schumacher W, Cho S, Hammerberg C, et al. Treatment of acne vulgaris with a pulsed dye laser: A randomized controlled trial. JAMA 2004;291:2834-9.
[Google Scholar]
|
| 30. |
Seaton ED, Mouser PE, Charakida A, Alam S, Seldon PE, Chu AC. Investigation of the mechanism of action of nonablative pulsed-dye laser therapy in photorejuvenation and inflammatory acne vulgaris. Br J Dermato 2006;155:748-55.
[Google Scholar]
|
| 31. |
Glaich AS, Friedman PM, Jih MH, Goldberg LH. Treatment of inflammatory facial acne vulgaris with combination 595-nm pulsed-dye laser with dynamic-cooling-device and 1,450-nm diode laser. Lasers Surg Med 2006;38:177-80.
[Google Scholar]
|
| 32. |
Karsai S, Schmitt L, Raulin C. The pulsed-dye laser as an adjuvant treatment modality in acne vulgaris: A randomized controlled single-blinded trial. Br J Dermatol 2010;163:395-401.
[Google Scholar]
|
| 33. |
Friedman PM, Jih MH, Kimyai-Asadi A, Goldberg LH. Treatment of inflammatory facial acne vulgaris with the 1450-nm diode laser: A pilot study. Dermatol Surg 2004;30:147-51.
[Google Scholar]
|
| 34. |
Jih MH, Friedman PM, Goldberg LH, Robles M, Glaich AS, Kimyai-Asadi A. The 1450-nm diode laser for facial inflammatory acne vulgaris: Dose-response and 12-month follow-up study. J Am Acad Dermatol 2006;55:80-7.
[Google Scholar]
|
| 35. |
Boineau D, Angel S, Auffret N, Dahan S, Mordon S. Treatment of active acne with an erbium glass (1.54 micron) laser. Lasers Surg Med 2004;16:S55.
[Google Scholar]
|
| 36. |
Kassir M, Newton D, Maris M, Euwer R, Servell P. Er: Glass (1.54 mm) laser for the treatment of facial acne vulgaris. Lasers Surg Med 2004;34:S65.
[Google Scholar]
|
| 37. |
Angel S, Boineau D, Dahan S, Mordon S. Treatment of active acne with an Er: Glass (1.54 microm) laser: A 2-year follow-up study. J Cosmet Laser Ther 2006;8:171-6.
[Google Scholar]
|
| 38. |
Bogle MA, Dover JS, Arndt KA, Mordon S. Evaluation of the 1,540-nm Erbium: Glass Laser in the Treatment of Inflammatory Facial Acne. Dermatol Surg 2007;33:810-7.
[Google Scholar]
|
| 39. |
Babilas P, Schreml S, Szeimies RM, Landthaler M. Intense pulsed light (IPL): A review. Lasers Surg Med 2010;42:93-104.
[Google Scholar]
|
| 40. |
Elman M, Lask G. The role of pulsed light and heat energy (LHE) in acne clearance. J Cosmet Laser Ther 2004;6:91-5.
[Google Scholar]
|
| 41. |
Kawana S, Tachihara R, Kato T, Omi T. Effect of smooth pulsed light at 400 to 700 and 870 to 1,200 nm for acne vulgaris in Asian skin Dermatol Surg 2010;36:52-7.
[Google Scholar]
|
| 42. |
Yeung CK, Shek SY, Bjerring P, Yu CS, Kono T, Chan HH. A comparative study of intense pulsed light alone and its combination with photodynamic therapy for the treatment of facial acne in Asian skin. Lasers Surg Med 2007;39:1-6.
[Google Scholar]
|
| 43. |
Sami NA, Attia AT, Badawi AM. Phototherapy in the treatment of acne vulgaris. J Drugs Dermatol 2008;7:627-32.
[Google Scholar]
|
| 44. |
Prieto VG, Zhang PS, Sadick NS. Evaluation of pulsed light and radiofrequency combined for the treatment of acne vulgaris with histologic analysis of facial skin biopsies. J Cosmet Laser Ther 2005;7:63-8.
[Google Scholar]
|
| 45. |
Ruiz-Esparza J, Gomez JB. Nonablative radiofrequency for active acne vulgaris: The use of deep dermal heat in the treatment of moderate to severe active acne vulgaris (thermotherapy): A report of 22 patients. Dermatol Surg 2003;29:333-9.
[Google Scholar]
|
| 46. |
Peng Q, Moan J, Warloe T, Nesland JM, Rimington C. Distribution and photosensitizing efficiency of porphyrins induced by application of exogenous 5-aminolevulinic acid in mice bearing mammary carcinoma. Int J Cancer 1992;52: 433-43.
[Google Scholar]
|
| 47. |
Bhardwaj S, Rohrer TE, Arndt K. Lasers and light therapy for acne vulgaris. Semin Cutan Med Surg 2005;24:107-12.
[Google Scholar]
|
| 48. |
Hongcharu W, Taylor CR, Chang Y, Aghassi D, Suthamjariya K, Anderson RR. Topical ALA-photodynamic therapy for the treatment of acne vulgaris. J Invest Dermatol 2000;115:183-92.
[Google Scholar]
|
| 49. |
Riddle CC, Terrell SN, Menser MB, Aires DJ, Schweiger ES. A review of photodynamic therapy (PDT) for the treatment of acne vulgaris. J Drugs Dermatol 2009;8:1010-9.
[Google Scholar]
|
| 50. |
Itoh Y, Ninomiya Y, Tajima S, Ishibashi A. Photodynamic therapy of acne vulgaris with topical delta-aminolevulinic acid and incoherent light in Japanese patients. Br J Dermatol 2001;144:575-9.
[Google Scholar]
|
| 51. |
Goldman MP, Boyce SM. A single-center study of aminolevulinic acid and 417 NM photodynamic therapy in the treatment of moderate to severe acne vulgaris. J Drugs Dermatol 2003;2:393-6.
[Google Scholar]
|
| 52. |
Gold MH, Bradshaw VL, Boring MM, Bridges TM, Biron JA. Treatment of sebaceous gland hyperplasia by photodynamic therapy with 5-aminolevulinic acid and a blue light source or intense pulsed light source. J Drugs Dermatol 2004;3: S6-9.
[Google Scholar]
|
| 53. |
Taub AF. Photodynamic therapy for the treatment of acne: A pilot study. J Drugs Dermatol 2004;3:S10-4.
[Google Scholar]
|
| 54. |
Alexiades-Armenakas M. Laser-mediated photodynamic therapy. Clin Dermatol 2006;24:16-25.
[Google Scholar]
|
| 55. |
Horfelt C, Funk J, Frohm-Nilsson M, Wiegleb Edstrom D, Wennberg AM. Topical methyl aminolevulinate photodynamic therapy for treatment of facial acne vulgaris: Results of a randomized, controlled study. Br J Dermatol 2006;155:608-13.
[Google Scholar]
|
| 56. |
56. Wiegell SR, Wulf HC. Photodynamic therapy of acne vulgaris using 5- aminolevulinic acid versus methyl aminolevulinate. J Am Acad Dermatol 2006;54:647-51.
[Google Scholar]
|
| 57. |
Wiegell SR, Wulf HC. Photodynamic therapy of acne vulgaris using methyl aminolevulinate: A blinded, randomized, controlled trial. Br J Dermatol 2006;154:969-76.
[Google Scholar]
|
| 58. |
Yeung CK, Shek SY, Bjerring P, Yu CS, Kono T, Chan HH. A comparative study of intense pulsed light alone and its combination with photodynamic therapy for the treatment of facial acne in Asian skin. Lasers Surg Med 2007;39: 1-6.
[Google Scholar]
|
| 59. |
Horfelt C, Stenquist B, Larko O, Faergemann J, Wennberg AM. Photodynamic therapy for acne vulgaris: A pilot study of the dose-response and mechanism of action. Acta Derm Venereol 2007;87:325-9.
[Google Scholar]
|
| 60. |
Taub AF. A comparison of intense pulsed light, combination radiofrequency and intense pulsed light, and blue light in photodynamic therapy for acne vulgaris. J Drugs Dermatol 2007;6:1010-6.
[Google Scholar]
|
| 61. |
Haedersdal M, Togsverd-Bo K, Wiegell SR, Wulf HC. Long-pulsed dye laser versus long-pulsed dye laser-assisted photodynamic therapy for acne vulgaris: A randomized controlled trial. J Am Acad Dermatol 2008;58:387-94.
[Google Scholar]
|
| 62. |
Orringer JS, Sachs DL, Bailey E, Kang S, Hamilton T, Voorhees JJ. Photodynamic therapy for acne vulgaris: A randomized, controlled, split-face clinical trial of topical aminolevulinic acid and pulsed dye laser therapy. J Cosmet Dermatol 2010;9:28-34.
[Google Scholar]
|
| 63. |
Jang MS, Doh KS, Kang JS, Jeon YS, Suh KS, Kim ST. A comparative split-face study of photodynamic therapy with indocyanine green and indole-3-acetic acid for the treatment of acne vulgaris. Br J Dermatol 2011;165:1095-100.
[Google Scholar]
|
| 64. |
Tuchin VV, Genina EA, Bashkatov AN, Simonenko GV, Odoevskaya OD, Altshuler GB. A pilot study of ICG laser therapy of acne vulgaris: Photodynamic and photothermolysis treatment. Lasers Surg Med 2003;33:296-310.
[Google Scholar]
|
Fulltext Views
18,203
PDF downloads
4,550





