Translate this page into:
Laugier-hunziker pigmentation
Correspondence Address:
Sanjeev Handa
Dept. of Dermatology, Venereology & Leprology PGIMER, Chandigarh-160 012
India
| How to cite this article: Ajith C, Handa S. Laugier-hunziker pigmentation. Indian J Dermatol Venereol Leprol 2005;71:354-356 |
Abstract
Laugier-Hunziker pigmentation (LHP) is an acquired disorder of hypermelanosis characterized by mucocutaneous hyperpigmentation. LHP may resemble various disorders characterized by mucocutaneous pigmentation. A 58-year-old lady presented with progressively increasing number of variable sized, hyperpigmented macules over the lips, fingers, toes and nails. There was no family history of similar illness. Systemic examination and all relevant investigations were within normal limits. Histopathology of a skin lesion had features consistent with LHP. The diagnosis of LHP must be made only after relevant investigations to rule out any associated systemic involvement. This case further highlights that LHP is not restricted to European countries.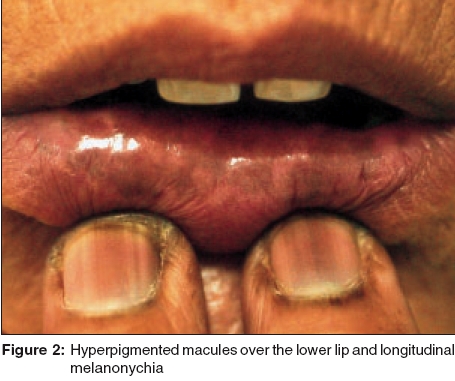 |
 |
 |
 |
Introduction
Laugier-Hunziker pigmentation (LHP) is an acquired disorder of hypermelanosis and involves the lips, oral mucosa, nails and acral areas in varying combinations. LHP may resemble various disorders characterized by mucocutaneous pigmentation. Differentiation from these disorders is essential as a few of them imply associated systemic disorders. Though LHP was initially thought to be restricted to European countries, it has been reported from many parts of world, including India. [1],[2],[3],
Case Report
A 58-year-old housewife presented with complaints of progressively increasing macular, hyperpigmented lesions over the lips, fingers, toes and nails. The lesions started 15 years back as longitudinal hyperpigmented streaks over toenails. Over the years, similar longitudinal streaks occurred on the fingernails. Since the last 4 years, she noticed multiple hyperpigmented macules on the lips, tongue and distal fingers and toes. There was no history of any systemic complaints. There was no family history of any pigmentary disorders, or any history of digestive tract tumors or disorders, though no other family members could be examined.
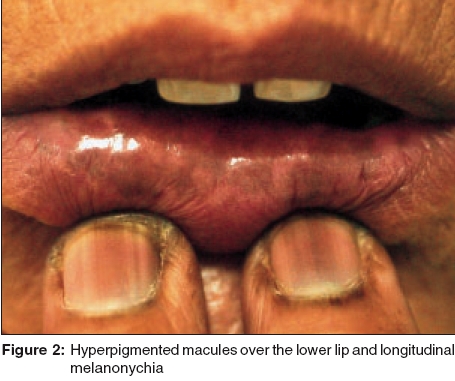
On examination, there were multiple, irregular, 2-5 mm sized pigmented macules over the fingers [Figure - 1] and toes as well as multiple lenticular lesions over the lower lips [Figure - 2]. A few larger melanotic patches were present over the tongue. Almost all the nails showed single or multiple longitudinal melanonychia [Figure - 2]. There were no vulval/genital mucosal melanotic lesions. No lesions were seen over the gums, palate or conjunctiva.
Investigations revealed normal hemogram and normal renal and liver function tests as well as normal hormonal assessment for pituitary adrenal dysfunction. Gastroscopy and colonoscopy revealed normal mucosal epithelium and no evidence of any polyps or growths. Barium meal follow through was normal except for the presence of suspicious duodenal malrotation, which was of no clinical significance. Histopathological examination of a skin biopsy from a lesion from the finger revealed mild acanthosis and increase in melanin pigmentation in the basal layer, but no increase in the number of melanocytes. There was no elongation of rete ridges.
The patient was explained about the benign nature of the condition.
Discussion
Acquired hyperpigmentation of lips and mouth along with longitudinal melanonychia was first described by Laugier and Hunziker in 1970.[4] LHP is characterized by discrete and confluent, slate to brown-black pigmented, lenticular and linear macules not associated with any systemic manifestations. The mucocutaneous sites involved are the lips (especially the lower lip) mucosae (including the gingiva, tongue, hard palate, soft palate, buccal mucosa, conjunctiva, and glans penis), corners of the mouth, and fingers. Pigmented macules may also be seen on the neck, thorax and abdomen. The nails may show longitudinal melanonychia. Pigmented macules have also been rarely described in perineal or perianal areas, sclera and esophagus.[1],[2],[3],[4],[5],Onset of the disease is usually after puberty. Most reports of the histopathologic changes in pigmented macules of Laugier and Hunziker describe increased basal layer pigmentation in skin and mucosal lesions, but normal numbers and morphologic appearance of melanocytes. [1],[2],[3],[4],[5],[6], But two recent reports demonstrated increased intraepidermal melanocytosis in the lesions of LHP, [5],[6],[7], with one report also describing significant cellular atypia of intraepithelial melanocytes from a macular lesion on a sun-exposed area.[5]
The differential diagnosis of LHP includes Peutz- Jeghers syndrome (PJS), LAMB syndrome and LEOPARD syndrome. Intraepidermal melanocytic hyperplasia has been identified in the pigmented macules of all these syndromes.[8] PJS is characterized by mucocutaneous lentigines prominent on the lips and genitalia and associated intestinal polyposis. Onset of the disease in PJS is usually early in life, whereas LHP manifests later. LAMB syndrome is characterized by lentigines of the skin and mucosa, a trial and m ucocutaneous myxomas, and multiple b lue nevi, while LEOPARD syndrome is characterized by lentigines, electrocardiographic abnormalities, o cular hypertelorism, p ulmonic stenosis, a bnormalities of genitalia, r etardation of growth, and d eafness.[9],[10] Another important differential diagnosis for LHP is Addison′s disease, which is characterized by darkening in areas of trauma and recent scars, at points of pressure and friction, nipples, areolae, axillae, perineum, and genitalia. Longitudinal melanonychia may occur, and diffuse pigmentation may appear on mucosal surfaces, especially the buccal mucosa, gums, and tongue.[10] The well-circumscribed pigmented macules of LHP can be readily distinguished from the more diffuse and accentuated pigmentation of Addison′s disease. Our patient had no manifestations suggestive of LAMB or LEOPARD syndrome. PJS and Addison′s disease were excluded by relevant investigations.
Though many authors have used the term Laugier- Hunziker syndrome, [1],[2],[3],[4],[5],[6],[7], recently the term has been disputed on the basis of the absence of any associated systemic abnormalities. The term Laugier and Hunziker pigmentation or mucocutaneous lentiginosis of Laugier and Hunziker is suggested instead.[5]
This report emphasizes that LHP is not restricted to European countries and proves the ubiquity of LHP.
| 1. |
Lenane P, Sullivan DO, Keane CO, Loughlint SO. The Laugier-Hunziker syndrome. J Eur Acad Dermatol Venereol 2001;15:574-7.
[Google Scholar]
|
| 2. |
Kanwar AJ, Kaur S, Kaur C, Thami GP. Laugier-Hunziker syndrome. J Dermatol 2001;28:54-7.
[Google Scholar]
|
| 3. |
Ayoub N, Barete S, Bouaziz JD, Le Pelletier F, Frances C. Additional conjunctival and penile pigmentation in Laugier-Hunziker syndrome: a report of two cases. Int J Dermatol 2004;43:571-4.
[Google Scholar]
|
| 4. |
Laugier P, Hunziker H. Pigmentation mιlanique lenticulaire, essentielle, de la muqueuse jugale et des lθvres. Arch Belg Dermatol Syphiligr 1970;26:391-9. Quoted from: Moore RT, Chae KA, Rhodes AR. Laugier and Hunziker pigmentation: A lentiginous proliferation of melanocytes. J Am Acad Dermatol 2004;50:70-4.
[Google Scholar]
|
| 5. |
Moore RT, Chae KA, Rhodes AR. Laugier and Hunziker pigmentation: A lentiginous proliferation of melanocytes. J Am Acad Dermatol 2004;50:70-4.
[Google Scholar]
|
| 6. |
Veraldi S, Cavicchini S, Benelli C, Gasparini G. Laugier-Hunziker syndrome: a clinical, histopathologic and ultra structural study of four cases and review of literature. J Am Acad Dermatol 1991;25:632-6.
[Google Scholar]
|
| 7. |
Koch SE, Le Boit PE, Odom RB. Laugier-Hunziker syndrome. J Am Acad Dermatol 1987;16:431-4.
[Google Scholar]
|
| 8. |
Rhodes AR. Benign neoplasias and hyperplasias of melanocytes. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, et al , editors. Fitzpatrick's Dermatology in general medicine. 5th edn. New York: McGraw-Hill; 1999. p. 1018-59.
[Google Scholar]
|
| 9. |
Mosher DB, Fitzpatrick TB, Ortonne JP, Hori Y. Hypomelanoses and hypermelanoses. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, et al , editors. Fitzpatrick's Dermatology in general medicine. 5th edn. New York: McGraw-Hill; 1999. p. 988-1001.
[Google Scholar]
|
| 10. |
Rhodes AR, Silverman RA, Harrist TJ, Perez-Atayde AR. Mucocutaneous lentigines, cardiomucocutaneous myxomas, and multiple blue nevi: the "LAMB" syndrome. J Am Acad Dermatol 1984;10:72-82.
[Google Scholar]
|
Fulltext Views
4,042
PDF downloads
3,522





