Translate this page into:
Lichen planus of the uterine cervix: A rare manifestation of mucocutaneous lichen planus
Correspondence Address:
Maryam Ranjbar
Skin Research Center, Shahid Beheshti University of Medical Sciences, Shohada-e Tajrish Hospital, Shahrdari St, 1989934148, Tehran
Iran
| How to cite this article: Barikbin B, Shakoei S, Ranjbar M. Lichen planus of the uterine cervix: A rare manifestation of mucocutaneous lichen planus. Indian J Dermatol Venereol Leprol 2014;80:264-265 |
Sir,
Lichen planus is a chronic inflammatory mucocutaneous disease. [1] The prevalence in the general population is reported to be 0.1-3%. [2] It is most common in the fourth decade of life and has a female-to-male prevalence ratio of 3:2. [1] To the best of our knowledge, there is only one case of cervical lichen planus reported so far. [3]
A 28-year-old woman with a history of cutaneous lichen planus for eight years presented to the gynecologist for a routine examination. She was asymptomatic and had no co-morbidities. She had been treated with oral prednisolone during the periods of exacerbation. There was no history of use of other drugs or intrauterine contraceptive devices prior to onset of lesions. She had undergone three sessions of cryotherapy at 4-week intervals with the diagnosis of cervicitis before being referred to our center; however there was no clinical response. At presentation, her skin lesions had relapsed. On gynecological examination, there was a whitish ulceration measuring 1.5 × 1 cm in the posterior lip of cervix at the 5 o′clock position. Her vulvovaginal examination was normal [Figure - 1]. The cervical smear showed non-specific inflammation. Mucocutaneous examination revealed generalized violaceous polygonal flat-topped papules on her trunk and extremities suggestive of classical lichen planus [Figure - 2].
Histopathological examination of the erosion revealed saw-toothed rete ridges in some areas of the epidermis and a band like lymphocytic infiltrate in the dermis with basal cell degeneration confirming the diagnosis of erosive lichen planus. There was no evidence of dysplasia in the epithelium. [Figure - 3]. Laboratory tests for human papilloma virus (HPV) and hepatitis C virus (HCV) infection were negative. Based on previous reports in the literature on safety and efficacy of methotrexate in lichen planus, including the vulvovaginal type, [4] we decided to treat her with oral methotrexate. After a 5 mg test dose, she was treated with oral methotrexate, 10 mg once weekly. After 3 months, there was a significant improvement in cutaneous lesions with a partial response in the cervical lesion [Figure - 1] and [Figure - 2].
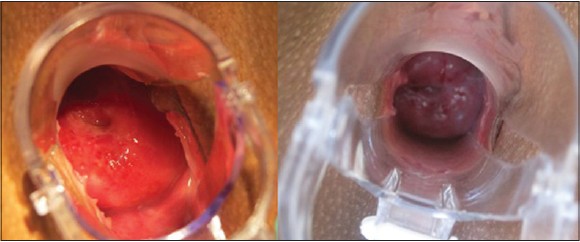 |
| Figure 1: A whitish ulceration measuring 1.5 × 1 cm in size at 5 o'clock position in the cervix. Improvement in the cervical lesion 5 months after treatment |
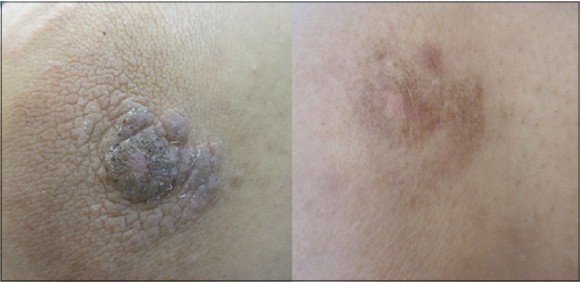 |
| Figure 2: Violaceous polygonal papules of cutaneous lichen planus before treatment. Improvement in papules after treatment |
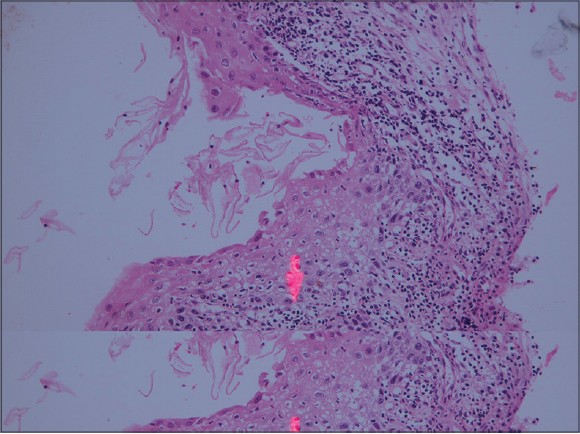 |
| Figure 3: Histopathology showing band- like dermal infi ltration of lymphocytes, neutrophils and plasma cells. Basal cell vacuolar degeneration was also seen (H and E, ×40) |
Vulvovaginal involvement is seen in approximately 57% of women with oral lichen planus while concomitant skin involvement is reported among 15% of the patients. [5] Another study also noted that vulvar lichen planus is more frequently associated with other mucosal lesions than skin lesions. [6] However, our patient presented with an erosive cervical lesion with no evidence of oral or external genital lesions. Oral disease is associated with several potential risk factors such as genetic predisposition, [1] infections, [3],[5] human papilloma virus [3],[6] and hepatitis C virus [5],[6] Since human papilloma virus infection is common in the cervix, [3] it is necessary to evaluate its role in cases of cervical lichen planus. Low-risk types of human papilloma virus were detected in a proportion of patients with vulvar lichen planus. [6]
Malignant transformation of cutaneous lesions of lichen planus has been reported to be less than 1%, [3] while the risk rate reported for oral lesions ranges from 0.4-5% in different studies. [3],[5],[6] There are few reports of squamous cell carcinoma in vulvar lichen planus. [3],[6] There is no information on the risk of malignant transformation in cervical lichen planus.
Examination of the cervix in women with generalized lichen planus will help us know how frequently this site is affected.
| 1. |
Lavanya N, Jayanthi P, Rao UK, Ranganathan K. Oral lichen planus: An update on pathogenesis and treatment. J Oral Maxillofac Pathol 2011;15:127-32.
[Google Scholar]
|
| 2. |
Fox LP, Lightdale CJ, Grossman ME. Lichen planus of the esophagus: what dermatologists need to know? J Am Acad Dermatol 2011;65:175-83.
[Google Scholar]
|
| 3. |
Gupta R, Bansal B, Singh S, Yadav I, Gupta K, Kudesia M. Lichen planus of uterine cervix-the first report of a novel site of occurrence: A case report. Cases J 2009;11;2:9306.
[Google Scholar]
|
| 4. |
Turan H, Baskan EB, Tunali S, Yazici S, Saricaoglu H. Methotrexate for the treatment of generalized lichen planus. J Am Acad Dermatol 2009;60:164-6.
[Google Scholar]
|
| 5. |
Kirtschig G, Wakelin SH, Wojnarowska F. Mucosal vulval lichen planus: Outcome, clinical and laboratory features. J Eur Acad Dermatol Venereol 2005;19:301-7.
[Google Scholar]
|
| 6. |
Kirtschig G, Brink AA, Scheper RJ, Jaspars EH. No oncogenic mucosal human papillomaviruses in erosive vulval lichen planus. Br J Dermatol 2005;152:1367-8.
[Google Scholar]
|
Fulltext Views
5,015
PDF downloads
1,921





