Translate this page into:
Lichen simplex chronicus of anogenital region: A clinico-etiological study
Correspondence Address:
Devinder Mohan Thappa
Department of Dermatology and STD, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry-605 006
India
| How to cite this article: Rajalakshmi R, Thappa DM, Jaisankar TJ, Nath AK. Lichen simplex chronicus of anogenital region: A clinico-etiological study. Indian J Dermatol Venereol Leprol 2011;77:28-36 |
Abstract
Background: Lichen simplex chronicus (LSC) of the anogenital region, is a benign, extremely uncomfortable disease. Aims: As very little is known about the cause of anogenital LSC (AGLSC), we undertook this study to determine various clinico-etiological factors involved in it and to assess the frequency of AGLSC. Methods: This was a descriptive study, including 105 patients with AGLSC, who attended the Dermatology clinic in our institute from September 2007 to June 2009. Detailed history, physical examination, and relevant investigations were done. The collected data were tabulated and analyzed. Results: The frequency of AGLSC among patients presenting with anogenital pruritus was 2.54%. Primary AGLSC was more common than secondary AGLSC (69.5% vs. 30.5%). AGLSC manifested more commonly in males than in females (56.2% vs. 43.8%). The mean duration of the disease was 30.6 months. The common triggering factors for itching were sweating (41.9%), rubbing of thighs while walking for long distances (9.5%), and mental stress (5.7%). Pruritus of AGLSC was related to the intake of various food items in 37.1% of patients. In males, scrotum was the predominant site involved (89.8%), whereas in females, labia majora was the predominant site involved (78.2%). Nearly one-third of cases (30.5%) of AGLSC had some other dermatoses in the anogenital region. Conclusions: Though psychological factors are thought to play an important role in disease causation and perpetuation among AGLSC patients, their significance could not be ascertained by us.Introduction
Lichen simplex chronicus (LSC) of the anogenital region, is a benign, but extremely uncomfortable disease characterized by skin thickening, hyperpigmentation and increased skin markings resulting from repetitive rubbing or scratching or picking of the skin. It is frequently a manifestation of an itch-scratch cycle. Anogenital LSC (AGLSC) develops predominantly in mid- to late adult life (30-50 years of age). [1] Despite being a common condition seen by the dermatologists, the incidence and prevalence figures have not been well established, and the factors operating in the causation as well as the perpetuation of the disease are poorly understood. Thus, this study was undertaken to determine the frequency of AGLSC among the patients presenting with anogenital pruritus, to explore the triggering factors for AGLSC and to look for the presence of other associated anogenital diseases contributing to LSC.
Methods
This was a descriptive study including 105 patients with AGLSC, which spanned over a period of 22 months, from September 2007 to June 2009. Institute ethics committee clearance was obtained. All patients attending the Dermatology OPD at JIPMER, Puducherry, with itching in the anogenital region were screened for LSC. Patients with other itchy dermatological diseases of the anogenital region, which were not associated with LSC, were excluded from the study. All consenting patients irrespective of their age and sex, with clinical diagnosis of LSC (thickened skin with accentuated skin markings resembling tree bark with or without signs of scratching like excoriations and crusting) in the anogenital region were enrolled in the study. Informed consent was taken; detailed history and examination findings were noted in a proforma. The severity of pruritus was rated on a 10-point Visual Analogue Scale (VAS). Results were tabulated and analyzed using SPSS 13.0 software.
Results
The frequency of AGLSC among the Dermatology OPD patients during the study period was 1.44 per 1000 patients. Among the patients presenting with anogenital pruritus, during the study period, frequency of AGLSC as a cause of anogenital pruritus was 2.54%. The mean age of the patients with AGLSC was 45.9 years with a range of 7-74 years. Most common age group was in 31-45 years (36.2%), followed by age groups of 46-60 years (32.4%), more than 60 years (16.2%), 15-30 years (14.2%) and <15 years (1 patient). There were 59 (56.2%) males and 46 (43.8%) females. The mean age in the males and females were 46.75 and 44.85 years, respectively. Majority of patients were farmers (35.2%), closely followed by housewives (30.5%). There were 17 (16.2%) laborers, 8 (7.6%) masons, 8 (7.6%) unemployed persons, 2 (1.9%) students and 1 (1%) shop owner.
The mean duration of AGLSC was 30.6 months with a range of 1 month-22 years. The mean duration in males and females were 31.6 and 29.4 months, respectively (not statistically significant). Itching was universally observed in all patients, which was paroxysmal in most patients (98/105, 93.3%). Seven patients (6.7%) were found to have continuous itching, and one patient reported that itching occurred at regular intervals. Itching was observed maximum during nighttime in majority of our patients (78/105, 74.2%). Ten patients had maximum itching during day time and 17 patients had no diurnal variations. Nighttime itching was more common in males (76.2%) than in females (71.7%), (not statistically significant).
Most common pruritus severity score (VAS) was 8, which was noted in 21.9% patients, followed by scores of 6 (20%), 5 (16.2%), and 7 and 9 (12.4% each). Three patients had a pruritus severity score of 10. The mean VAS in our patients was 6.39. The proportion of patients with a VAS score of 6-10 (73/105, 69.5%) was higher than that with VAS score of ≤5 or less. VAS of 6-10 was more common in the higher age groups, as shown in [Figure - 1]. VAS of 6-10 was seen in higher percentage of female patients compared to males (76.1% vs. 64.4%). But the difference in VAS in male and female gender was not statistically significant (P value = 0.197).
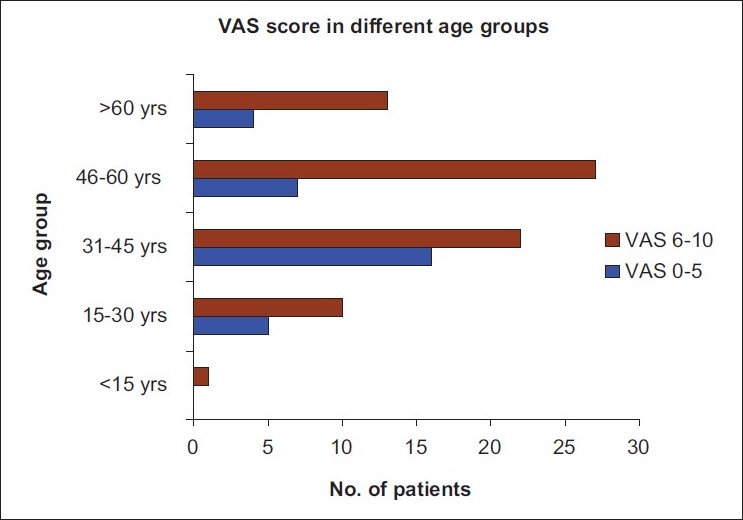 |
| Figure 1 :Bar chart showing VAS score in different age groups |
Response to the itching was scratching (78/105, 74.2%), rubbing (35/105, 33.3%) and picking (3/105, 2.8%) the itchy areas. Sensation perceived during scratching, rubbing or picking of the itchy areas was burning sensation (56.5%), relief or pleasure (30.6%), exacerbation of itch sensation (6.5%), pain (4.8%), non-descript discomfort and pricking sensation (0.8% each). The mean duration of time taken for scratching/rubbing/picking to relieve itching was 10.94 minutes, with a range of 1-90 minutes. The most common end point of intense scratching/rubbing/ picking was burning sensation (32.1%), closely followed by oozing (29.2%), pain (16.1%), relief of itching or pleasure on scratching (13.7%), bleeding (8.3%) and a non-descript discomfort (0.6%).
Majority of the patients (66/105, 62.9%) in our study used their non-dominant hand for scratching or rubbing or picking the itchy lesions. Twenty-four out of 105 patients (22.0%) used their dominant hand, whereas 15/105 patients (14.3%) used both the hands for the same. For scratching the itchy lesions in the anogenital region, majority (66/105, 62.9%) of the patients used the nails alone, 3 patients (1.9%) used a comb, and one patient also used blade. One patient used to rub with the palm of the hand or sometimes rub his penis and scrotum against the floor to get relief from itching. Majority of the patients (84/105, 61%) experienced an exacerbation of itching during the summer season, and 2/105 (1.9%) patients experienced a winter exacerbation.
Most common triggering factor for itching was sweating observed in 44 patients (41.9%). Other initiating factors for the itching were rubbing of the thighs while walking for long distances (10/105, 9.5%), patients′ mental stress (6/105, 5.7%), crawling sensation (2), micturition (2), pain (2), burning (1), coitus (1), constipation (1), defecation (1), physical stress (1), pricking sensation (1) and shaving the pubic hair (1). Personal and/or family history of atopy was present in 27 patients (25.7%), whereas 78 patients (74.3%) had no features of atopy (personal/family). Among the 105 patients, 39 (37.1%) gave a history of increased itching after eating various food items. Most common food item was brinjal (29 patients), followed by dried fish (25 patients) as shown in [Table - 1].

A large majority of the patients 99/105 (94.3%) used topical preparations of medications, cosmetics (soap, oil, talcum powder), irritants and various chemicals like KMnO 4 solution, dettol, shikakai (a herbal preparation commonly used by the villagers in Tamil Nadu). Seventeen out of 105 (16.2%) patients used antifungal creams or powder, 12/105 (11.4%) patients used steroid-antifungal combination preparations, 6/105 (5.7%) patients used plain steroids, 3/105 (2.9%) patients used steroid-antibiotic combination preparations, and one patient each used steroid and antifungal-antibiotic combination. Self-medication (details of which were not known) was used by 25 (23.8%) patients. Overall, 90 patients used some kind of cosmetics in the anogenital region. Soap was the commonest one used by 88 patients (97.7%), followed by talcum powder (4/105, 3.8% patients) and oil (3/105, 2.8% patients), either alone or in combinations.
Only 68 (64.7%) patients used to wear undergarments regularly. Among them, 65 patients used cotton undergarments and 3 patients used polyester undergarments. Majority of the patients used colored undergarments (61 - colored cotton, 3 - colored polyester, 4 - white cotton). Thirty-seven out of 105 patients (35.2%) did not use undergarments, out of which two patients stopped using that because of increased itching. Out of the 20 females in the reproductive age group, 18 patients (90%) used cotton cloth during menstrual periods. Only 2 patients (10%) used sanitary napkin pads available in the market. Among the 18 patients who used cotton cloth, 14 (77.7%) had symptoms of irritation due to the cloth, and one among the two patients using sanitary napkin pads had symptoms of irritation. None of the female patients in our study used vaginal tampons or perfumes in the anogenital region.
Our patients suffered from dermatophyte infections (10 patients, 8.8%), scabies (4 patients, 3.5%), folliculitis of the groin region (2 patients, 1.8%), vulvovaginal candidiasis (2 patients, 1.8%), and one each of candidal intertrigo, bacterial vaginosis, gonorrhea, recurrent herpes genitalis, and undiagnosed vaginal discharge. Some patients had anal complaints of bleeding per rectum (13/105, 12.4%), fissure-in-ano (7/105, 6.7%), pain during defecation (15/105, 14.3%), constipation (18/105, 17.1%).
In our study, only 7 out of 105 patients (6.7%) had psychiatric disorders, 14/105 patients (13.3%) had worries about their family matters, 10/105 patients (9.5%) had worries about their personal health and financial issues and one patient (Turner′s syndrome) was found to have mental retardation. One patient mentioned that anogenital lesions started after stopping the promiscuous behavior and one patient mentioned that guilty feeling about his promiscuous behavior aggravated his anogenital lesions.
The lichenified plaque was the key feature to identify cases of LSC in our study. These lesions were localized plaques in 65 (61.9%) patients and lesions were diffuse in nature in 42 (40%) patients (involving entire labia majora, labia minora, perineum or scrotum). Entire scrotum was involved by lichenification in 18/59 (30.5%) male patients. The lichenified plaques showed one of the following characteristics: (a) lichenified plaques surrounded by multiple papules in the margin [in 21/105 (20%) patients], (b) multiple discrete papules overlying the lichenified plaque [in 12/105 (11.4%) patients], and (c) excoriations in the lichenified plaque [in 11/105 (10.4%) patients]. Scaling and crusting were seen in two patients (1.9%) each, and one patient each showed fissuring, maceration, nodules, postinflammatory hypopigmentation, intense hyperpigmentation and small papules (in the perianal region).
The predominant sites of involvement in male and female patients were scrotum (89.8%) and labia majora (78.2%), respectively [Figure - 2],[Figure - 3],[Figure - 4],[Figure - 5],[Figure - 6],[Figure - 7].
 |
| Figure 2 :Pie chart showing different sites of involvement in males |
 |
| Figure 3 :Pie chart showing different sites of involvement in females |
 |
| Figure 4 :Lichenified plaque with papules involving both labia majora |
 |
| Figure 5 :Lichenified plaque with excoriation involving the perianal region with skin tag |
 |
| Figure 6 :Diffuse lichenification of the entire scrotum |
 |
| Figure 7 :Secondary lichenification due to scabies |
The lesions of LSC in the anogenital region were found to be symmetrical in 92 patients and asymmetrical in 13 patients. Among the asymmetrical lesions, majority (10/13) were seen on the right side, and only 3 were seen on the left side. The distribution of the asymmetrical lesions did not coincide with the predominant hand used for scratching/rubbing/ picking.
Evidence of side effects to topical steroids in the form of atrophy of the skin was seen in three patients who had history of long-term application of superpotent topical steroids (clobetasol propionate) in the anogenital region.
Hypertrophy of labia minora was seen in 8/46 females in our study. Atrophy of labia minora was seen in four females. Atrophy of the clitoris was seen in six females, out of whom five patients had lichen sclerosus et atrophicus (LSA), which could have been the cause of atrophy of the clitoris. Vaginal introitus was erythematous, edematous and showed erosions in five patients, of whom four had vulvovaginal candidiasis and three had associated LSA. Vaginal discharge was seen in five patients, (4 - vulvovaginal candidiasis, 1 - bacterial vaginosis). Uterine prolapse with rectocele and candidal intertrigo was seen in one patient. Lichenification of the crural folds was seen in 59/105 (56.2%) patients.
Thirty-two patients (30.5%) had other anogenital dermatoses like tinea cruris (8.6%), erythrasma (4.8%) and LSA (4.8%), acrochordons (five patients), vulvovaginal candidiasis (four patients), intertrigo, scabies and psoriasis in two patients each, and bacterial vaginosis in one patient. None of our patients with vulvovaginal candidiasis had oral candidiasis.
Discussion
LSC is a common pruritic skin disorder characterized by lichenified plaques resulting from irresistible and persistent scratching or rubbing. It can be either primary arising de novo on tissue with a normal appearance or secondary due to various dermatological disorders. [1],[2] AGLSC is quite a common condition seen by the dermatologists; yet there is only limited literature available on this subject. What remains more challenging is characterizing the obscure nature of the etiologic factors in a majority of cases and appropriately addressing the psychological morbidity that may accompany any disorder involving the anogenital region.
The prevalence of AGLSC varies depending on the population in question, age of the patients, gender, and the presence of other dermatological disorders, etc. The prevalence of AGLSC was about 0.5% in the general population of the western Europe and America, [1] 10% in a study in a multidisciplinary vulvar clinic, [3] 30.5% in a specialist referral vulvar clinic [4] and 35% among non-neoplastic vulvar biopsies. [5] In our study, the frequency of AGLSC among patients attending the Dermatology OPD was 1.44 per 1000 population. AGLSC also contributed to 2.5% of patients presenting with AG pruritus in our study.
AGLSC is common in mid- to late adult life (30-50 years of age). [2],[6] The mean age of patients with vulvar LSC in studies conducted by Singh et al. [7] and O′Keefe et al. [5] were 49.9 and 42 years (range 22-76 years), respectively. These findings are in concordance with our study where we found that the mean age of AGLSC cases was 45.9 years with a vast majority of cases (89/105 patients, 84.7%) being more than 30 years of age.
AGLSC in adults occurs more commonly in the females, [2],[6] with a female to male ratio of 2:1. [8] There are various reasons for vulva being commonly involved by irritant and/or allergic contact dermatitis, which can predispose to the development of vulvar LSC. [9] For example, the skin of the labia majora exhibits elevated hydration, occlusion and frictional properties, which may increase susceptibility to irritants and contact sensitizers. Furthermore, the non-keratinized vulvar vestibule is likely to be more permeable than keratinized regions. [9] The vulva is also more prone to maceration, overheating and excessive friction as a result of occlusive clothing and physical activity. Exposure to urine, vaginal secretions, sweat and seminal fluid can be irritating, particularly on skin that is chronically inflamed. [10] Contrary to the existing literature, we found that the AGLSC was more common in the males than in females (59 males vs. 46 females) with a male to female ratio of 1.2:1. The reasons for females being less commonly affected in our study could be partly explained by the rarity of use of undergarments (35.2% did not use undergarments) and/or any cosmetics other than soaps (perfumes, sprays, panty liners) by the females in this part of South India, and also the reluctance to expose the genitals.
Patients with atopic dermatitis have a low tolerance for soap and other irritating substances which are often excessively used on the vulva, particularly by women who fear lack of cleanliness may be the cause of their problem. [10] Singh [11] found a significant association between LSC and a personal and family history of atopic disorders. The incidence of asthma and allergic rhinitis in his patients with LSC was significantly higher than in controls. Family history of atopy was positive in 44.1% of patients as compared to 17% of controls in that study. [11] In our study, personal and/or family history of atopy (allergic rhinoconjunctivitis, asthma, atopic dermatitis) was present in 27 patients (25.7%).
To the best of our knowledge, there is no study addressing the role of food items in aggravating the itching in LSC. In our study, 39 (37.1%) patients among the 105 patients gave a history of increased itching after eating various food items like brinjal, dried fish, egg, chicken, mutton or potato. Most common food item was brinjal (29 patients) followed by dried fish (25 patients). The limitation of our study was that we did not undertake oral provocation test to confirm their true role.
AGLSC may be primary or secondary. Certain pruritic diseases [candidiasis, dermatophyte infections, psoriasis, human papillomavirus (HPV) infections, infestations with scabies and lice, neoplasia, allergic contact dermatitis, and in females, lichen sclerosus], presumably through dysfunction of the barrier layer, allow for the peripheral nerve endings to be stimulated and act as stimulus for the development of a superimposed itch-scratch cycle. [1],[8],[12] Other factors which contribute to the development of LSC include heat and sweat retention, rubbing of clothing, irritating topical products like over-the-counter preparations such as medications containing benzocaine, tea-tree oil and aloe vera, antiseptics, antifungals, douches, lubricants, preservatives, plastic-backed sanitary pads, panty liners, perfumed sprays, and irritation of menstrual products. [1],[10]
All the cases of vulvar LSC were primary in the study conducted by Singh et al. [7] In our study, 73 cases (69.5%) were primary LSC, whereas 32 (30.5%) were secondary to various conditions like tinea cruris (9 patients, 8.6%), erythrasma (5 patients, 4.8%), LSA (5 patients, 4.8%), vulvovaginal candidiasis (4 patients), intertrigo, scabies and psoriasis in 2 patients each, and bacterial vaginosis in one patient. Perianal skin tags were seen in 5 patients out of 17 patients with LSC in the perianal region.
Any irritant or allergic contact dermatitis can predispose to the development of AGLSC. [1],[8] The role of contact sensitization in vulvar LSC has been evaluated by Virgili et al. [12] with the help of patch testing with the Italian standard series and with a wide battery of allergens (preservatives, perfumes, emulsifiers, medicaments). In their study, they found that 47.5% of women with vulvar LSC had at least one positive patch test, and relevant positivities (mostly medicaments and preservatives) were observed in 26% patients. [12] Contact dermatitis to rubber compounds is not uncommon and accounts for 5-10% of positive patch test results. With the increased use of condoms, contact dermatitis to rubber is being seen more often. [13] Nowadays, most of the condoms are made up of latex. In our study, however, only 7/105 (6.7%) patients had a history of latex condom use but none of them had any symptoms after using latex condoms. Forty-four patients (41.9%) in our study observed that sweating (while working in a hot environment) triggered the anogenital itching. Other main factors which triggered the itching were rubbing of the thighs while walking for long distances (10/105 patients, 9.5%) and mental stress (6/105 patients, 5.7%). Eighteen out of 20 (90%) females in the reproductive age group in our study used cotton cloth during menstrual periods and 14 (77.7%) patients among them had symptoms of irritation. None of the female patients in our study used vaginal tampons, panty liners, perfumed sprays or vaginal douches in the anogenital region.
LSC has been found to be associated with anxiety, depression, and obsessive-compulsive disorder. [1],[2],[6] According to Lynch, patients with LSC only rarely volunteer that psychological factors play a role in their disease. [1] Psychological factors have been shown to be associated with neurodermatitis in different studies by Shrivastava et al., [14] Ayyar and Bagadia, [15] Konuk et al., [16] and Singh et al. [7] In our study, 31/105, (29.5%) patients admitted having some psychological factors playing a role in their disease causation and perpetuation. We found that 7 out of 105 patients (6.7%) were diagnosed to be suffering from psychiatric disorders.
Severe, intractable pruritus is the hallmark of LSC and is present in almost all patients. [1],[2],[6] Most patients with AGLSC claim that they can control the amount of scratching they do so during the daytime. In contrast, patients generally recognize that they are not able to control the scratching that occurs at night. [1] In our study, itching was universally observed in all patients and it was maximum during nighttime in majority of our patients (78/105, 74.2%).
When severity of pruritus was assessed based on the scale devised by Sanjana and Fernandez, [17] significantly higher proportions of patients had VAS score of 6-10 (73/105, 69.5%) compared to 32 (30.5%) patients with VAS score of 5 or less. Most common pruritus severity score was 8 (23 patients, 21.9%), followed by scores of 6 (21 patients, 20%) and 5 (17 patients, 16.2%). All these findings substantiated the fact that itching was severe in AGLSC. VAS of 6-10 was seen in a higher percentage of female patients compared to males (76.1% vs. 64.4%), indicating that female patients probably experienced more intense pruritus.
Most of the patients respond to pruritus of LSC with vigorous rubbing or scratching. [18] Majority of our patients (78/105, 74.2%) responded to itch by scratching rather than rubbing (35/105, 33.3%) or picking (3/105, 2.8%). Lynch observed that in most instances, scratching occurs in multiple bouts of several minutes each, totaling about 15 minutes per night. [1] In our study, the mean duration of time taken by the patients for scratching/rubbing/picking to relieve itching (in each bout) was 10.94 minutes with a range of 1-90 minutes. There are other responses like pleasure, pain on scratching/ rubbing, but adequate data in this regard are lacking. In our study, we found that a majority of the patients scratched/rubbed the itchy areas until a burning sensation (32.1%) or pain (16.1%) was perceived, or oozing (29.2%) from the lesions.
Patients with AGLSC regularly report that the severity of itching worsens with heat and sweating. [1] Pruritus-specific C neurons are also temperature sensitive, which could explain the observation that itching is worse in a warm environment. [19] In our study, majority of the patients (84/105, 61%) experienced an exacerbation of itching during the summer season which could be attributed to the above fact. Singh et al. [7] did not find any correlation between occupation and LSC of the vulva. But in our study, farmers and housewives were found to be more commonly affected compared to other occupational groups like laborers, mason, students, and unemployed individuals. This could be partly explained by the prevailing hot environmental conditions the farmers and housewives are exposed to. High percentage of farmers (78.3%) and housewives (68.7%) also had higher VAS of 6-10.
Thickening of the skin is the most dominant clinical feature in almost all instances of LSC. In the anogenital region, thickened stratum corneum appears white and wrinkled and somewhat smoother as a result of absorption of moisture present in these areas. [1] One or more relatively well-defined lichenified plaques are seen with thick white debris, and varying degrees of overlying excoriation, described as "dermatological worry beads", are usually seen. The lesions of AGLSC of longstanding duration show areas of hyperpigmentation and hypopigmentation. [1],[18] Lichenified papules, which are usually follicular or perifollicular, may be found at the periphery of the lichenified plaques. [1] The lichenified plaques in our patients showed one or more of the following three patterns: plaques surrounded by multiple papules at the margin, multiple discrete papules overlying the lichenified plaque, or lichenified plaques with excoriations. Other changes that were evident in the AGLSC plaques were scaling, crusting, fissuring, maceration, nodules, post-inflammatory hypopigmentation, and intense hyperpigmentation.
LSC of the anogenital region is usually bilateral, but the distribution may be asymmetrical or even unilateral, reflecting a preference for scratching with the dominant hand. [1] Singh et al., [7] in their study found that 15 out of 16 patients with vulvar LSC had bilaterally symmetrical lesions and one patient had asymmetrical involvement with lichenification only on the side of dominant hand. Our study also revealed lesions of AGLSC to be symmetrical in 92 (87.6%) patients and asymmetrical in only 13 (12.3%) patients. Among the asymmetrical lesions, majority (10/13) were seen on the right side, which was also the dominant hand in them.
In men, the scrotum is the most frequently involved site, but lesions also commonly occur on the proximal portion of the penis and the penile shaft. Entire scrotum may be rarely involved. [20] Rajashekhar et al. [20] reported a rare case of LSC diffusely involving the entire scrotum in a middle-aged male with history of psychological upset for not conceiving a male child. In our study, we found that scrotum was the predominant site of involvement in 53 out of 59 (89.8%) male patients, followed by perineum (9 patients, 15.2%), perianal region (7 patients, 11.8%), and shaft of penis (5 patients, 8.4%). Contrary to the existing report of the rarity of the involvement of the entire scrotum by AGLSC, diffuse involvement of the scrotum was seen in 18 out of 53 male patients. Among them, scrotal rugosities were found to be prominently increased in 9 patients. Rest of the 35 patients with scrotal LSC had localized lichenified plaques over the lateral, dorsal and/or ventral surface of scrotum.
In women, the labia majora are the most frequently affected sites. Other sites involved are labia minora, vulvar vestibule, mons pubis, perineum and along the upper inner thighs, but lesions are never found within the vagina. [1] In Singh et al.′s study, [7] labia majora was found involved in all the 16 cases of vulvar LSC, and two cases also had involvement of labia minora. Literature suggests that the perianal area is another site of predilection in both men and women, [1] but the exact prevalence of it is not known in either gender. In our study, 17 out of 105 patients had LSC involving the perianal region, which was marginally more common in the females (10 females vs. 7 males). Out of 17 patients with perianal LSC, 7 (5 females and 2 males) also had fissure-in-ano.
AGLSC as such is considered to be a benign disease, [1] but in occasional cases, due to vigorous scratching architectural distortion in the form of genital distortion (clitoral or labial hypertrophy), [21] scarring and fibrosis can occur. [1] Singh et al. [7] noted clitoral hypertrophy in one of their patients with vulvar LSC. In our study, hypertrophy of labia minora was seen in 8/46 females. Atrophy of labia minora was seen in four females. Atrophy of the clitoris was seen in six females, out of whom five patients had LSA of the vulva. None of the patients with clitoral atrophy gave history of using topical steroids. Vaginal introitus was erythematous, edematous and showed erosions in five patients, out of whom four had vulvovaginal candidiasis and three had associated LSA of the vulva. Lichenification of the crural folds was seen in 59/105 (56.2%) patients. Hydrocele was seen in two male patients and inguinal hernia was seen in one male patient. Both hydrocele and inguinal hernia probably produce occlusion in the inguinal region, inducing itch sensation.
Conclusions
To conclude, AGLSC commonly occurs after 30 years of age. AGLSC is more common in males than in females, probably due to the rarity of use of undergarments and/or any cosmetics other than soaps (perfumes, sprays, panty liners) by the females in this part of South India, also the reluctance of females to expose their genitals to physicians, and willingness to visit their gynecologist rather than dermatologist. Primary AGLSC is more common than secondary AGLSC. In one-third of cases, AGLSC can occur secondary to various conditions like tinea cruris, erythrasma, LSA, vulvovaginal candidiasis, intertrigo, scabies, psoriasis, bacterial vaginosis and perianal skin tags. Hydrocele and inguinal hernia in males can produce occlusion in the inguinal region, inducing itch sensation and LSC. Though psychological factors are thought to play an important role in disease causation and perpetuation among the AGLSC patients, their significance could not be ascertained by us. Pruritus of AGLSC can be related to the intake of various food items like brinjal, dried fish, egg, chicken, mutton or potato in our population. Pruritus of AGLSC can be triggered by sweating (while working in a hot environment), rubbing of the thighs while walking for long distances and mental stress. Patients with AGLSC respond to itch by scratching rather than rubbing or picking. Scrotum is the predominant site of involvement in males, followed by perineum, perianal region, shaft of penis, mons pubis and penoscrotal junction. LSC diffusely involving the entire scrotum is not uncommon. Labia majora is the predominant site of involvement in females, followed by perianal region, labia minora, perineum, gluteal cleft, mons pubis and introitus. Hypertrophy of the labia minora can occur in longstanding cases of vulvar LSC. LSC involving the perianal region may be more common in females than in males.
| 1. |
Lynch PJ. Lichen simplex chronicus (atopic/neurodermatitis) of the anogenital region. Dermatol Ther 2004;17:8-19.
[Google Scholar]
|
| 2. |
Holden CA, Berth-Jones J. Eczema, lichenification, prurigo and erythroderma. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7 th ed. Oxford: Blackwell Science Ltd; 2004. p. 17.1-55.
th ed. Oxford: Blackwell Science Ltd; 2004. p. 17.1-55.'>[Google Scholar]
|
| 3. |
Sullivan AK, Straughair GJ, Marwood RP, Staughton RC, Barton SE. A multidisciplinary vulva clinic: The role of genito-urinary medicine. J Eur Acad Dermatol Venereol 1999;13:36-40.
[Google Scholar]
|
| 4. |
Cheung ST, Gach JE, Lewis FM. A retrospective study of the referral patterns to a vulval clinic: Highlighting educational needs in this subspecialty. J Obstet Gynaecol 2006;26:435-7.
[Google Scholar]
|
| 5. |
O'Keefe RJ, Scurry JP, Dennerstein G, Sfameni S, Brenan J. Audit of 114 non-neoplastic vulvar biopsies. Br J Obstet Gynaecol 1995;102:780-6.
[Google Scholar]
|
| 6. |
Burgin S. Nummular eczema and lichen simplex chronicus/prurigo nodularis. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's Dermatology in General Medicine. 7 th ed. New York: McGraw-Hill Companies; 2008. p. 158-62.
th ed. New York: McGraw-Hill Companies; 2008. p. 158-62.'>[Google Scholar]
|
| 7. |
Singh N, Thappa DM, Jaisankar TJ, Habeebullah S. Pattern of non-venereal dermatoses of female external genitalia in South India. Dermatol Online J 2008. Vol. 14.
[Google Scholar]
|
| 8. |
Lotti T, Buggiani G, Prignano F. Prurigo nodularis and lichen simplex chronicus. Dermatol Ther 2008;21:42-6.
[Google Scholar]
|
| 9. |
Farage MA. Vulvar susceptibility to contact irritants and allergens: A review. Arch Gynecol Obstet 2005;272:167-72.
[Google Scholar]
|
| 10. |
Fischer G, Spurrett B, Fischer A. The chronically symptomatic vulva: Aetiology and management. Br J Obstet Gynaecol 1995;102:773-9.
[Google Scholar]
|
| 11. |
Singh G. Atopy in lichen simplex (neurodermatitis circumscripta). Br J Dermatol 1973;89:625-7.
[Google Scholar]
|
| 12. |
Virgili A, Bacilieri S, Corazza M. Evaluation of contact sensitization in vulvar lichen simplex chronicus. J Reprod Med 2003;48:33-6.
[Google Scholar]
|
| 13. |
Rademaker M, Forsyth A. Allergic reactions to rubber condoms. Genitourin Med 1989;65:194-5.
[Google Scholar]
|
| 14. |
Srivastava ON, Bhat VK, Singh G. Personality profile in neurodermatitis. Indian J Psychiatry 1977;19:71-6.
[Google Scholar]
|
| 15. |
Ayyar KS, Bagadia VN. A controlled study of psychosocial factors in neurodermatitis. Indian J Psychiatry 1986;28:155-8.
[Google Scholar]
|
| 16. |
Konuk N, Koca R, Atik L, Muhtar S, Atasoy N, Bostanci B. Psychopathology, depression and dissociative experiences in patients with lichen simplex chronicus. Gen Hosp Psychiatry 2007;29:232-5.
[Google Scholar]
|
| 17. |
Sanjana VD, Fernandez RJ. Lichen simplex chronicus: A psychocutaneous disorder? Indian J Dermatol Venereol Leprol 1995;61:336-8.
[Google Scholar]
|
| 18. |
Millard LG, Cotterill JA. Psychocutaneous disorders. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7 th ed. Oxford: Blackwell Science Ltd; 2004. p. 61.1-41.
th ed. Oxford: Blackwell Science Ltd; 2004. p. 61.1-41.'>[Google Scholar]
|
| 19. |
Greaves MW. Pruritus. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7 th ed. Oxford: Blackwell Science Ltd; 2004. p. 16.1-15.
th ed. Oxford: Blackwell Science Ltd; 2004. p. 16.1-15.'>[Google Scholar]
|
| 20. |
Rajashekhar N, Thippeswamy C, Prasanna NB. Lichen simplex chronicus of scrotum. Indian J Dermatol Venereol Leprol 1999;65:91-2.
[Google Scholar]
|
| 21. |
Pincus SH. Vulvar dermatoses and pruritus vulvae. Dermatol Clin 1992;10:297-308.
[Google Scholar]
|
Fulltext Views
12,413
PDF downloads
4,702





