Translate this page into:
Lichen simplex chronicus of the scalp: A clinical and trichoscopic perspective
Corresponding author: Dr. Anuradha Bishnoi, Department of Dermatology, Venereology and Leprology, PGIMER, Chandigarh, India. dranha14@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Malhi K, Singh S, Mehta H, De D, Dogra S, Bishnoi A, et al. Lichen simplex chronicus of the scalp: A clinical and trichoscopic perspective. Indian J Dermatol Venereol Leprol. 2024;90:819-22. doi: 10.25259/IJDVL_1274_2023
Dear Editor,
Lichen simplex chronicus (LSC) of the scalp is a chronic pruritic neurodermatitis characterised by non-scarring hair loss. This disorder often resembles alopecia areata or trichotillomania (TTM). However, there are subtle clinical and trichoscopic clues to differentiate these disorders. Herein, we describe three cases of LSC of the scalp, in which trichoscopy proved valuable and indispensable in arriving at a definitive diagnosis [Table 1].
| Case | Age/Sex | Clinical | Trichiscopy | Histopathology |
|---|---|---|---|---|
| Patient 1 | 50/F | 10 × 6 cm irregularly shaped, non-cicatricial alopecic patch on the vertex and mid-frontal scalp with variable length hair shafts and non-adherent greyish-white scaling | Multiple broken hairs, black dots, ‘broom hairs’, yellowish-white perifollicular scaling, erythema and perifollicular brown halo | Marked hyperkeratosis, keratotic plugging, parakeratosis, hypergranulosis, acanthosis and papillomatosis with perifollicular fibrosis and dermal inflammation |
| Patient 2 | 60/F | Well-defined, non-scarring 5 × 4 cm alopecic patch on the vertex, with broken hair shafts, lichenification and greyish-white scaling | Trichoscopy exhibited characteristic features, including ‘broom fibres’, diffuse perifollicular scaling and hyperpigmentation | Hyperkeratosis, acanthosis, dermal inflammation around perifollicular region |
| Patient 3 | 64/F | Well-defined 8 × 12 cm alopecic patch with lichenification over vertex and occiput was noted along with hyperpigmentation, erythema and scaling | Multiple broom fibres along with perifollicular scales | Characteristic hamburger sign with splitting of hair shaft due to hyperkeratosis at the level of infundibulum over the background of perifollicular fibrosis and inflammation |
The first case was a middle-aged female with year-long progressive scalp hair loss accompanied by severe pruritus and burning sensation. Clinical examination revealed a 10 × 6 cm irregularly shaped, non-cicatricial alopecic patch on the vertex and mid-frontal scalp with variable length hair shafts and non-adherent greyish-white scaling [Figure 1a]. Dermoscopic examination unveiled multiple broken hairs, black dots, ‘broom hairs’, yellowish-white perifollicular scaling, erythema and perifollicular brown halo [Figure 2a]. Histopathology indicated marked hyperkeratosis, keratotic plugging, parakeratosis, hypergranulosis, acanthosis and papillomatosis with perifollicular fibrosis and dermal inflammation leading to a diagnosis of LSC scalp [Figure 3a]. Intralesional triamcinolone acetonide injections and antihistamines resulted in partial hair regrowth and symptom resolution within two months.

- Irregular alopecic patch over mid-frontal scalp extending up to vertex.

- A delineated alopecic patch present over the vertex with broken hair shafts and background lichenification.

- Well-defined, alopecic patch over vertex and occiput with background lichenification.
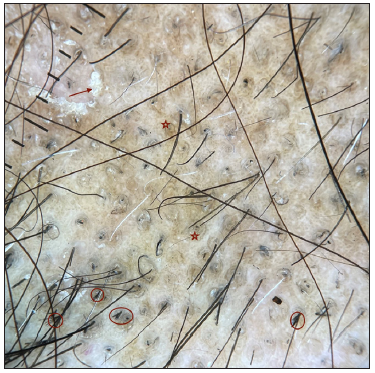
- Trichoscopy (patient 1)- blackdots, broom fibres (red circle) with white perifollicular scales (red arrow) and perifollicular brown halo (red star). (Dermlite DL4, non polarised, 10x).

- Multiple ‘broom fibres’ (red circle), diffuse perifollicular scaling (red star) and hyperpigmentation were evident on the trichoscopy of patient two. (Dermlite DL4, non-polarised, 10x).

- Multiple broom fibres (red circle) along with perifollicular scales in the trichoscopy of patient three. (Dermlite DL4, (Non-polarised, 10x).
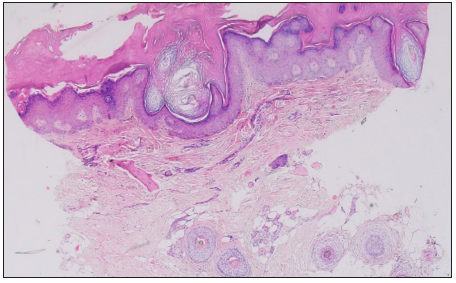
- Histopathology (patient 1) showing hyperkeratosis, acanthosis, hypergranulosis, dermal inflammation and perifollicular fibrosis. (Haematoylin and eosin, 40x).
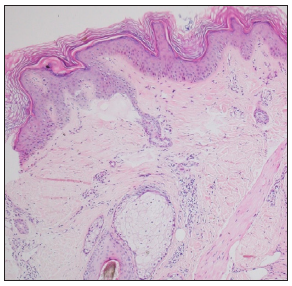
- Patient 2- Hyperkeratosis, acanthosis and dermal inammation (Haematoxylin and eosin, 200x).
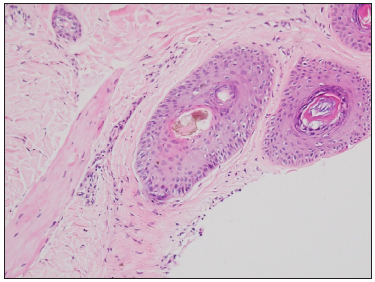
- Patient 3- Characteristic hamburger signs with the splitting of the hair shaft due to hyperkeratosis at the level of the infundibulum with background perifollicular fibrosis and inammation (Haematoxylin and eosin, 400x).
The second case was a 60-year-old healthy female presenting with severe pruritus and a four-month history of patchy hair loss over the scalp. Examination revealed a well-defined, non-scarring 5 × 4 cm alopecic patch on the vertex, with broken hair shafts, lichenification and greyish-white scaling [Figure 1b]. Trichoscopy exhibited characteristic features, including ‘broom fibres’, diffuse perifollicular scaling, and hyperpigmentation [Figure 2b]. Histopathology showed similar findings of hyperkeratosis, acanthosis and dermal inflammation [Figure 3b]. Based on the above findings, a diagnosis of scalp LSC was made. Treatment with potent topical corticosteroid lotion (mometasone furoate 0.1%) and antihistamines resulted in symptomatic improvement.
The third patient was a 64-year-old lady who presented with severe itching along with hair loss over the vertex for 18 months. On examination, a well-defined 8 × 12 cm alopecic patch with lichenification over the vertex and occiput was noted, along with hyperpigmentation, erythema and scaling [Figure 1c]. Trichoscopy showed multiple broom fibres along with scaling [Figure 2c]. Histopathology showed characteristic hamburger sign with the splitting of hair shaft due to hyperkeratosis at infundibular infundibulum over a background of perifollicular fibrosis and inflammation [Figure 3c]. Based on the above findings, a diagnosis of LSC scalp was made, and the patient was managed with potent topical steroids and antihistamines.
LSC is a vexing pruritic dermatosis with a notable female predominance, typically affecting the accessible sites such as shins, forearms and external genitalia.1 Scalp involvement, though uncommon, manifests as irregular alopecic patches with prominent scaling concealing underlying redness. The relentless pruritus compels repetitive scratching, often exacerbated by emotional and psychological factors, potentially leading to rubbing and secondary lichenification.
LSC is frequently misdiagnosed as tinea capitis, alopecia areata or TTM. However, specific clinical, trichoscopic and histopathological features may aid in its accurate diagnosis [Table 2]. Chronic, incessant pruritus, accompanied by perifollicular and interfollicular scaling and follicular plugging, is a hallmark of LSC. Trichoteiromania is a psychocutaneous disorder with perpetual rubbing of hair with minimal symptoms and absence of scaling, erythema and atrophy. In contrast, a patient with LSC scalp has severe pruritus resulting in scratching and subsequent lichenification. All our patients were evaluated for trichoteiromania, a close mimic of LSC scalp, utilising the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM V) criteria; none of our patients satisfied the proposed criteria. Trichoscopic findings in both LSC and trichoteiromania share similarities, featuring ‘broom fibres’, indicating short hairs emerging from a single follicular opening, breaking into two to three shafts due to repetitive frictional trauma.2,3 These broom fibres are distinctive markers of scalp LSC. As seen above in our cases, background erythema and hyperpigmentation frequently accompany LSC of the scalp. The trichoscopic findings in TTM include broken hairs of varying length, perifollicular haemorrhages, V sign, tulip hair and mace hair. Trichoteiromania, a variant of TTM, as described above, may show some features of TTM along with broom fibres.4
| LSC scalp | Alopecia areata | Trichotillomania | Trichoteiromania | Tinea capitis | |
|---|---|---|---|---|---|
| Clinical findings |
Irregular alopecic patches with broken hairs. Background scaling, thickening, hyperpigmentation and erythema prominent (lichenification). Presents with severe and incessant pruritus |
Predominantly regular shaped, smooth, non-cicatricial alopecic patches with no erythema or scaling. Can be itchy and scaly after topical application of irritants | Irregular, bizarre-shaped, multifocal, alopecic patches mainly over the vertex. ‘Friar Tuck’ sign may be seen | Single or multiple lesions may be observed, characterised by lichenified, often pruritic plaques containing broken short hairs. Patient usually denies pruritus; admits to habitual rubbing of the hair | Scaly erythematous alopecic patches with broken and lustreless hairs. Associated cervical lymphadenoapthy |
| Trichoscopic features |
‘Broom fibres’ Background erythema and hyperpigmentation |
Exclamation mark hairs, black dots, coudability hairs, yellow dots |
Broken hairs of irregular lengths, ‘V sign’, tulip hairs(broken hair with diagonal fracture), mace hair (broken terminal hairs with bulged distal end), and flame hairs (residues from recently pulled hairs) constitute the diverse trichoscopic findings |
The striking presence of consistent clusters of broom-like hairs, infrequent erosions, crusts with blood, and dilated blood vessels | Comma hairs, corkscrew hairs, broken hairs, block hairs, ‘morse code hairs’ (Microsporum infections) |
| Histopathological features | Epidermal hyperplasia, orthokeratosis and hypergranulosis with a perivascular lymphocytic infiltrate. Jagged projections at the infundibulum ‘gearwheel sign’ and hair shaft splitting into two layers secondary to infundibular hyperkeratosis ‘hamburger sign’4 | Peribulbar lymphocytic infiltrate affecting terminal hairs ‘swarm of bees’ appearance. ‘Shift out of anagen’ into telogen; dysmorphic hair casts | Increased number of catagen hair follicles (>75%). Bulbar epithelium distortion, haemorrhage, pigmentary incontinence and trichomalacia | Orthokeratosis and hyperkeratosis with minimal dermal inflammation and absent perifollicular infiltrates. Features in congruity with LSC scalp in the later stages | Mixed inflammatory infiltrate, damage of the follicular epithelium. Positive fungal stains (PAS, Grocott) |
Histopathology of the LSC scalp reveals distinct characteristics, including epidermal hyperplasia, orthokeratosis, hypergranulosis and a perivascular lymphocytic infiltrate with scattered eosinophils in those with atopic backgrounds. Notably, the number of terminal hairs remain unchanged, preserving follicular integrity. Jagged projections called the ‘gearwheel’ sign are observed at the infundibular level.4 Furthermore, hyperkeratosis at the infundibular ostia splits hair shafts into two layers, forming the ‘hamburger sign’.4 These histopathological findings serve as distinct indicators for LSC and are the basis of some dermoscopic signs described above.
Ruling out other differentials is essential asthe treatment strategy is different and aims to identify triggers and disrupt the itch-scratch cycle, encompassing psychological evaluation, counselling and the use of high-potency topical or intralesional steroids.5 Sedating antihistamines and tricyclic antidepressants like amitriptyline (10–25 mg/day) and doxepin (up to 280 mg/day) are viable options, albeit with consideration for potential adverse effects such as sedation and anticholinergic actions.5
This report highlights three cases of LSC scalp, a chronic and pruritic dermatological condition often misdiagnosed as other hair disorders. Trichoscopy can play a crucial role in diagnosing LSC and initiating appropriate management.
Acknowledgements
We extend our sincere appreciation to Dr. Vinay Keshavamurthy, Dr. Apoorva Sharma and Dr. Debajyoti Chatterjee for their invaluable contributions by providing clinical details and histopathological data pertaining to this manuscript.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Lichen simplex chronicus on the scalp: Exuberant clinical, dermoscopic, and histopathological findings. An Bras Dermatol. 2018;93:108-10.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Monotonous broom hairs: A feature of trichoteiromania. Skin Appendage Disord. 2020;6:168-70.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Weathering of hair in trichoteiromania. Australas J Dermatol. 2004;45:186-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopic-pathologic correlation of lichen simplex chronicus on the scalp: ‘Broom fibers, gear wheels and hamburgers’. J Eur Acad Dermatol Venereol. 2016;30:343-5.
- [CrossRef] [PubMed] [Google Scholar]
- Trichoscopic diagnosis and management of a case of scalp dysesthesia with lichen simplex chronicus. Int J Trichology. 2022;14:218-20.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





