Translate this page into:
Linear and whorled nevoid hypermelanosis in three successive generations
Correspondence Address:
Arun Kumar Metta
Department of Dermatology, Venereology, and Leprology, Kamineni Institute of Medical Sciences, Narketpally, Nalgonda - 508 254, Andhra Pradesh
India
| How to cite this article: Metta AK, Ramachandra S, Sadath N, Manupati S. Linear and whorled nevoid hypermelanosis in three successive generations. Indian J Dermatol Venereol Leprol 2011;77:403 |
Sir,
Linear and whorled nevoid hypermelanosis (LWNH) is characterized by hyperpigmented macules in a streaky configuration along the lines of Blaschko, without preceding inflammation or atrophy. [1],[2],[3] Lesions are distributed mainly on the trunk and extremities, sparing palms, soles, and mucosae. The usual age of the onset of hyperpigmentation occurs within the first few weeks of life, continues to progress for a year or two before stabilization. [4] There are very few case reports from India and abroad. We are reporting one such rare case of familial LWNH.
A 12-year-old girl, her 45-year-old mother, and 65-year-old grandmother presented to our out-patient department with chief complaints of asymptomatic, dark coloured skin lesions over the body since early life. In the child, lesions appeared over the buttocks at the age of 6 months and gradually progressed to involve both upper and lower limbs by the age of 2 years. The lesions darkened with age and no new lesions appeared after the age of 5 years. There was history of fading of lesions with time, in her mother and grandmother. None of them had any history of warty lesions or blisters. There was no history suggestive of any recurrent lower respiratory infections, involvement of cardiovascular and central nervous systems.
The child was born of full term, normal vaginal delivery, with normal growth and development. There was no history of consanguinity in the family. There was no history of foetal deaths in the family. Apart from the three of them, no other family members have been affected. Systemic examination was unremarkable. Cutaneous examination in the child revealed multiple, whorled, hyperpigmented macules, arranged bilateral and symmetrical, along the lines of Blaschko on the abdomen, chest, and back [Figure - 1]. Similar lesions were arranged linearly on extensor and flexor aspects of both the upper and lower limbs. The texture of skin was normal over the streaks as well as the intervening skin.
 |
| Figure 1: Child: classical whorled, hyperpigmented macules along the lines of Blaschko on the trunk |
Mother had similar hyperpigmented macules along the Blaschko′s lines, on the flexor and extensor aspects of the right upper limb, both the buttocks and flexor aspect of the right lower limb [Figure - 2]. Grandmother had similar lesions on both the buttocks and the right thigh [Figure - 3]. There was evidence of partial to complete disappearance of pigmentation along the lines of Blaschko on the extremities and trunk, in both the mother and grandmother. Scalp, face, palms, soles, and genitalia were spared. Hair, nails, teeth, eyes, and mucosae were normal.
 |
| Figure 2: Mother and child: linear, hyperpigmented streaks over the extensor aspect of the forearms, with near complete disappearance on the left forearm in the mother |
 |
| Figure 3: Grandmother: remnant of whorled pigmentation over both the buttocks |
Hemogram and routine biochemical tests revealed no abnormalities. Radiological investigations including X-ray, CT scan, and 2D echo detected no congenital anomalies. Histopathological evaluation of the pigmented macules revealed increased pigmentation of the basal cell layer with melanocytes present up to the mid epidermis [Figure - 4]. There were focal areas of pigmentary incontinence noticed in the dermis. Genetic studies performed on the peripheral blood from the mother revealed trisomy on chromosome 20, but this study was found to be negative in the child. Fluorescence in situ hybridization (FISH) was advised to rule out similar trisomy in the daughter.Based on clinicopathological correlation, a diagnosis of LWNH was made in all the three family members. The family was reassured of the benign nature of the disorder. A periodic follow up was recommended at our dermatology unit.
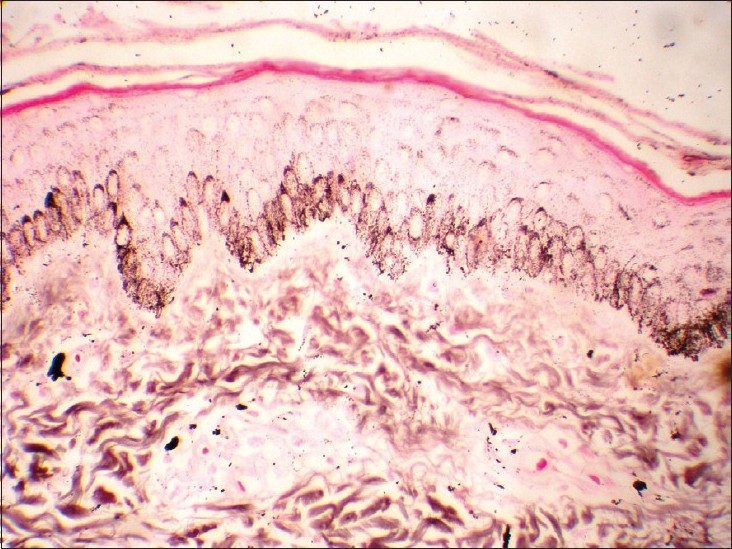 |
| Figure 4: Photomicrograph showing basal layer hypermelanosis and focal areas of pigmentary incontinence in the dermis. (Fontana masson ×40) |
Linear and whorled nevoid hypermelanosis is a rare disorder of pigmentation. Similar cases have been described in the literature bearing different names such as zosteriform hyperpigmentation, zosteriform lentiginous nevus, and zebra-like hyperpigmentation. Kalter et al., [1] described LWNH as having onset within a few weeks of age with no preceding inflammation or palpable lesion. Gradual spread occurs during the first 1 to 2 years of life with subsequent stabilization. The macules may become less prominent with age in some patients. Streaks and whorls follow the lines of Blaschko and do not cross the midline. There is sparing of the face, palms and soles, eyes, and mucous membranes. Similar observations were made in our patients.
Various skeletal anomalies, central nervous system diseases (microcephaly, arhinencephaly and epilepsy), [2] congenital heart diseases (ventricular septal defect and tetralogy of Fallot), [3] psychomotor delay, deafness and brachydactyly have been mentioned in the literature in association with LWNH. No such abnormalities were noticed in our patients.
Histopathology reveals an increase in pigmentation of the basal layer and prominence or vacuolization of melanocytes. Pigmentary incontinence is usually, but not always absent. Similar findings were noticed in our cases.
Genetic studies have been performed on both peripheral blood lymphocytes and cultured dermal fibroblasts. There is increasing evidence to suggest somatic mosaicism as a cause for LWNH. Mosaic trisomy of 7, 14, 18, 20 [3] and X-chromosomal mosaicism have been reported. Trisomy 20 has been noticed in the mother.
The differential diagnosis includes incontinentia pigmenti, hypomelanosis of Ito, and epidermal nevus. The skin lesions pass through four successive stages of vesicles, verrucous lesions, whorls or streak like hyperpigmentation and hypopigmented scars in incontinentia pigmenti. [1] Histopathologically, there is basal cell degeneration, pigmentary incontinence, tissue eosinophilia, and dermal melanophages. The lack of the above-mentioned features both clinically and histopathologically helped us in ruling out incontinentia pigmenti. [5] The pattern of pigmentation in hypomelanosis of Ito resembles "marble cake" or the reverse pattern of the late hypermelanosis in incontinentia pigmenti. [1] Epidermal nevi often present during infancy as hyperpigmented macules along lines of Blaschko. With time, they turn hyperkeratotic and papillomatous. The absence of verrucous lesions along with the absence of hyperkeratosis, acanthosis, papillomatosis, and elongation of rete ridges in histopathology, ruled out the possibility of epidermal nevus. [5]
The familial occurrence of LWNH is extremely rare with a single case being reported [4] in the literature, occurring in two successive generations.
To the best of our knowledge, this is most probably the first case of LWNH occurring in three successive generations being reported in the English literature.
| 1. |
Kalter DC, Griffiths WA, Atherton DJ. Linear and whorled nevoid hypermelanosis. J Am Acad Dermatol 1988;19:1037-44.
[Google Scholar]
|
| 2. |
Alrobaee AA, Alsaif F. Linear and whorled hypermelanosis associated with developmental delay and generalized convulsions. Int J Dermatol 2004;43:145-7.
[Google Scholar]
|
| 3. |
Hartmann A, Hoffman UB, Hoehn H, Broecker EB, Hamm H. Postnatal confirmation of prenatally diagnosed trisomy 20 mosaicism in a patient with linear and whorled nevoid hypermelanosis. Paediatr Dermatol 2004;21:636-41.
[Google Scholar]
|
| 4. |
Akiyama M, Aranami A, Sasaki Y, Ebihara T, Sugiura M. Familial linear and whorled nevoid hypermelanosis. J Am Acad Dermatol 1994;30:831-3.
[Google Scholar]
|
| 5. |
Brar BK, Mahajan BB, Puri N. Linear and whorled nevoid hypermelanosis. Indian J Dermatol Venereol Leprol 2009;74:512-3.
[Google Scholar]
|
Fulltext Views
4,408
PDF downloads
3,174





