Translate this page into:
Linear lesions in dermatology
Correspondence Address:
Dipali D Malvankar
Department of Skin, STD and Leprosy, # 52, OPD Block, Victoria Hospital, Bangalore-560 002
India
| How to cite this article: Malvankar DD, Sacchidanand S, Mallikarjun M, Nataraj H V. Linear lesions in dermatology. Indian J Dermatol Venereol Leprol 2011;77:722-726 |
Introduction
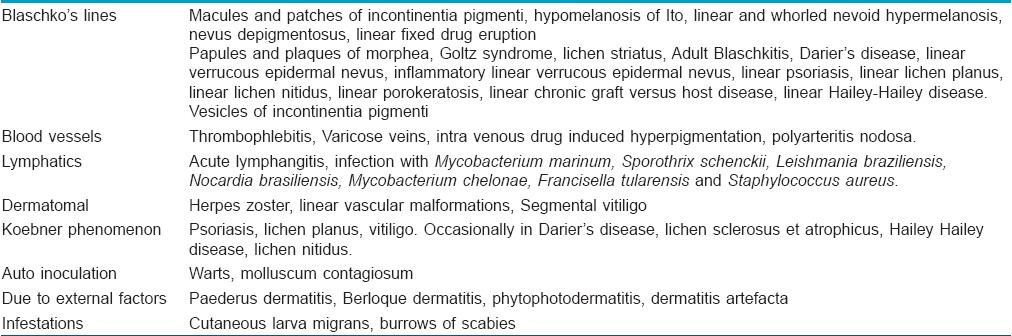
Linear lesions in dermatology are commonly encountered. They vary in cause; being congenital or acquired; vary in morphology and can present as macules, papules, patches, plaques, vesicles or nodules; they can be inflammatory or non inflammatory; it can be a single lesion which is linear or multiple lesions which are arranged in a linear pattern. The causes for occurrence in a linear pattern include lesions following Blaschko′s lines, blood vessels, lymphatics and dermatomes; due to Koebner′s phenomenon and auto inoculation; external factors; infestations like cutaneous larva migrans and burrows of scabies. We review each of these causes one by one.
Blaschko′s Lines
Blaschko′s lines are imaginary skin lines which various skin conditions are known to follow. They do not follow neural, vascular, or lymphatic structures and are distinct from dermatomes as well as Langer′s lines. [1] These were first described by Alfred Blaschko in 1901. The most widely accepted basis for these lines is genotypic mosaicism, i.e., presence of more than one type of cell lines within the body. [2],[3] The causes for mosaicism are half chromatid mutation, lyonization, post zygotic mutation, chromosomal non disjunction, and chimerism. [3] The most common disorders following Blaschko′s lines are enlisted in [Table - 1]. [2],[3],[4],[5]
[Figure - 1], [Figure - 2] and [Figure - 3] show a few conditions following Blaschko′s lines.
 |
| Figure 1: Case of linear verrucous epidermal nevus showing multiple linear verrucous papules since birth with superimposed warts in the proximal part |
 |
| Figure 2: Case of incontinentia pigmenti with multiple linear and whorled papulo-vesicular lesions and streaks of hyperpigmentation |
 |
| Figure 3: Case of linear porokeratosis presenting with multiple asymptomatic plaques on the lower limb |
There are case reports of hypermelanotic macules of McCune-Albright syndrome, [6] extragenital lichen sclerosis, [7] eosinophilic cellulitis, [8] erythematous rash of scarlet fever, [9] Bart syndrome, [10] linear scalp lupus profundus, [11] all following Blaschko′s lines.
Blood Vessels
Blood vessels have a longitudinal course in the body. Hence, lesions which occur in blood vessels are likely to have a linear pattern. These include the following:
- Thrombophlebitis refers to blood vessel inflammation along with thrombus formation. Two types are recognised - superficial and deep. Superficial thrombophlebitis is visible and presents with erythema and tenderness in the skin along the distribution of the affected blood vessel. [12] Mondor′s disease is a type of superficial thrombophlebitis which affects the breast and sometimes the penis, which presents with a linear and tender cord- like thickening of the affected vein. [13],[14]
- Varicose veins present with dilated and tortuous veins commonly occurring in the lower limbs due to insufficient closure of valves causing backflow from deep to superficial veins. [15] Veins being linearly arranged, these lesions show a linear distribution.
- Intravenous drug induced hyperpigmentation presents with linear hyperpigmented streaks along the course of veins. It commonly occurs in case of intravenous drugs given for malignancies [16] [Figure - 4].
- Polyarteritis nodosa is a necrotising inflammation of blood vessels which presents with nodules and ulcers mainly on the lower limbs along the distribution of blood vessels.
 |
| Figure 4: Case of gastric carcinoma on treatment with 5-fluorouracil having linear streaks of hyperpigmentation along the vein of injection |
Lymphatics
The following conditions follow lymphatics:
- Lymphangitis is the inflammation of lymph vessels. Acute lymphangitis is streptococcal infection of lymphatics of subcutaneous tissue presenting with erythematous linear streaks from the site of infection to the draining lymph nodes. [17] It also occurs in early stages of filariasis.
- Nodular lymphangitis is a clinical presentation in which erythematous papules and nodules occur along the course of lymphatics. [18] This occurs mainly in chronic suppurative inflammatory disorders of the skin in which causative organisms spread via lymphatics. This distribution commonly occurs in sporotrichosis and hence is also called sporotrichoid distribution [Figure - 5]. The differential diagnosis for this includes infection with Mycobacterium marinum, Sporothrix schenckii, Leishmania braziliensis, Nocardia species, Mycobacterium chelonae, Francisella tularensis, and Staphylococcus aureus. [18],[19],[20],[21]
 |
| Figure 5: Case of sporotrichosis showing linear distribution of nodular lesions over the upper limb |
Dermatomes
A dermatome is a linear area of skin supplied by a single spinal nerve. The following conditions follow dermatomes:
- Herpes zoster presents with multiple erythematous vesicles with burning sensation along the distribution of a particular spinal nerve.
- Vascular malformations like capillary malformations are sometimes are distributed along a dermatomal segment [22] [Figure - 6].
- Vitiligo is an acquired disorder which presents with depigmented macules and patches. Sometimes, this disorder follows dermatomal segments when it presents with linear macules and patches and is called as dermatomal, segmental, zosteriform or pseudosegmentalis type of vitiligo. [23] Segmental vitiligo has an early onset, rapid progression and no specific precipitating factors. [24] In one study, the most commonly involved dermatome was the trigeminal and only a few patients had an associated autoimmune disease. [24]
 |
| Figure 6: Case of segmental vascular malformation affecting the upper limb |
Koebner′s Phenomenon
Koebner′s phenomenon was first described by Heinrich Koebner, [25] and refers to the development of isomorphic lesions at the sites of trauma in case of cutaneous disorders. [26] Scratching being a common cause of cutaneous trauma, leads to linear lesions along the line of scratching. True Koebner′s phenomenon occurs in psoriasis, lichen planus and vitiligo and is also occasionally seen in other conditions [26] [Table - 1].
Auto Inoculation
This is also termed as pseudo Koebner′s phenomenon. It occurs in infectious disorders like due to implantation of infectious agent in the skin during trauma leading to development of isomorphic linear lesions like in Koebner′s phenomenon. Examples include warts and molluscum contagiosum [26] [Figure - 7].
 |
| Figure 7: Case of extensive verruca plana showing pseudo koebnerisation with linear lesions |
External Factors
- Paederus dermatitis (dermatitis linearis, [27] or blister beetle dermatitis [28] ) commonly occurs in tropical and subtropical regions. It is a peculiar irritant contact dermatitis characterized by sudden onset linear erythematous and bullous lesions and burning on exposed areas of the body. [28] It occurs when beetles of the genus Paederus (also called rove beetles) are crushed on the skin, releasing the vesicant pederin, which causes irritant dermatitis [29] [Figure - 8].
- Berloque dermatitis occurs when perfumes containing bergamot oil are applied followed by exposure to sunlight. It presents with erythema and hyperpigmentation along the pattern formed by the trickle of droplets, which is usually linear. [30]
- Phytophotodermatits (meadow dermatitis, strimmer dermatitis, weed wacker dermatitis) [30] occurs due to furocoumarins in plants which cause a phototoxic reaction. It commonly presents with linear streaks along the area of contact with the irritant. [31]
- Dermatitits artefacta: Dermatitis artefacta (factitious dermatitis) refers to self-inflicted skin injuries made consciously to elicit sympathy, escape responsibility, or collect disability insurance. The lesions are common on areas which are easily accessible and commonly arranged in a linear pattern. [32]
 |
| Figure 8: Case of paederus dermatitis showing multiple papulovesicular lesions arranged linearly over the face |
Infestations
- Cutaneous larva migrans is a skin infestation clinically characterized by erythematous linear serpiginous lesions caused by nematode larvae. [33]
- The burrows made by the scabies mite in the skin are also commonly linear.
Conclusion
The importance of linear lesions in dermatology cannot be over emphasized. Linear lesions act as diagnostic clues in many disorders. They also help in elucidating the pathogenesis as they give a clue to the pathway of spread of the disease. Koebner phenomenon indicates the presence of active disease and helps to decide the line of management.
| 1. |
Jackson R. The lines of Blaschko: A review and reconsideration: Observations of the cause of certain unusual linear conditions of the skin. Br J Dermatol 1976;95:349-60.
[Google Scholar]
|
| 2. |
Tagra S, Talwar AK, Walia RS. Lines of Blaschko. Indian J Dermatol Venereol Leprol 2005;71:57-9.
[Google Scholar]
|
| 3. |
Moss C. Mosaicism and linear lesions. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2 nd ed. Spain: Mosby Elsevier; 2008. p. 841-5.
[Google Scholar]
|
| 4. |
Bolognia JL, Orlow SJ, Glick SA. Lines of Blaschko. J Am Acad Dermatol 1994;31:157-90.
[Google Scholar]
|
| 5. |
Moss C, Larkins S, Stacey M, Blight A, Farndon PA, Davison EV. Epidermal mosaicism and Blaschko's lines. J Med Genet 1993;30:752-5.
[Google Scholar]
|
| 6. |
Rieger E, Kofler R, Borkenstein M, Schwingshandl J, Soyer HP, Kerl H. Melanotic macules following Blaschko's lines in McCune-Albright syndrome. Br J Dermatol 1994;130:215-20.
[Google Scholar]
|
| 7. |
Choi SW, Yang JE, Park HJ, Kim CW. A case of extragenital lichen sclerosus following Blaschko's lines. J Am Acad Dermatol 2000;43:903-4.
[Google Scholar]
|
| 8. |
Sommer S, Wilkinson SM, Merchant WJ. Eosinophilic cellulitis following the lines of Blaschko. Clin Exp Dermatol 1999;24:449-51.
[Google Scholar]
|
| 9. |
Duran-McKinster C, Moises C, Rodriguez-Jurado R, Tamayo-Sanchez L, Orozco-Covarrubias L, Ruiz-Maldonado R. Streptococcal exanthem in a blaschkolinear pattern: Clinical evidence for genetic mosaicism in hypomelanosis of ito. Pediatr Dermatol 2002;19:423-5.
[Google Scholar]
|
| 10. |
Duran-McKinster C, Rivera-Franco A, Tamayo L, De La Luz Orozco-Covarrubias M, Ruiz-Maldonado R. Bart Syndrome: the congenital localized absence of skin may follow the lines of Blaschko: Report of Six Cases. Pediatr Dermatol 2000;17:179-82.
[Google Scholar]
|
| 11. |
Nagai Y, Ishikawa O, Hattori T, Ogawa T. Linear lupus erythematosus profundus on the scalp following the lines of Blaschko. Eur J Dermatol 2003;13:294-6.
[Google Scholar]
|
| 12. |
Torpy JM, Burke AE, Glass RM. JAMA patient page: Thrombophlebitis. JAMA 2006;296:468.
[Google Scholar]
|
| 13. |
Pugh CM, DeWitty RL. Mondor's disease. J Natl Med Assoc 1996;88:359-63.
[Google Scholar]
|
| 14. |
Kumar B, Narang T, Radotra BD, Gupta S. Mondor's disease of penis: A forgotten disease. Sex Transm Infect 2005;81:480-2.
[Google Scholar]
|
| 15. |
Nullen H, Noppeney T. Diagnosis and treatment of varicose veins, Part 1: Definition, epidemiology, etiology, classification, clinical aspects, diagnostic and indications. Chirurq 2010;81:1035-44.
[Google Scholar]
|
| 16. |
Alley E, Green R, Schuchter L. Cutaneous toxicities of cancer therapy. Curr Opin Oncol 2002;14:212-6.
[Google Scholar]
|
| 17. |
Singh G, Kaur V, Singh S. Bacterial infections. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3 rd ed. Mumbai: Bhalani Publishing House; 2008. p. 232.
[Google Scholar]
|
| 18. |
Giordano CN, Kalb RE, Brass C, Lin L, Helm TN. Nodular lymphangitis: Report of a case with presentation of a diagnostic paradigm. Dermatol Online J 2010;16:1.
[Google Scholar]
|
| 19. |
Schneider P, Monsel G, Veziris N, Roujeau JC, Bricaire F, Caumes E. Successful treatment of nodular lymphangitis due to Mycobacterium chelonae in two immunosuppressed patients. Dermatol Online J 2011;17:8.
[Google Scholar]
|
| 20. |
Kostman JR, DiNubile MJ. Nodular lymphangitis: A distinctive but often unrecognized syndrome. Ann Intern Med 1993;118:883-8.
[Google Scholar]
|
| 21. |
Lieberman AA, Grossman ME, Bloomgarden D. Sporotrichoid lymphangitis due to Staphylococcus aureus in a diabetic patient. Clin Infect Dis 1995;21:433-4.
[Google Scholar]
|
| 22. |
Boon LM, Vikkula M. Vascular Malformations. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's Dermatology in General Medicine. 7 th ed. New York: McGraw Hill Book; 2008. p. 1652.
th ed. New York: McGraw Hill Book; 2008. p. 1652.'>[Google Scholar]
|
| 23. |
Dhar S, Dutta P, Malakar R. Pigmentary Disorders. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3 rd ed. Mumbai: Bhalani Publishing House; 2008. p. 753.
[Google Scholar]
|
| 24. |
Hann SK, Lee HJ. Segmental vitiligo: Clinical findings in 208 patients. J Am Acad Dermatol 1996;35:671-4.
[Google Scholar]
|
| 25. |
Kuner N, Hartschuh W, Khan-Durani B. Heinrich Kobner and the "isomorphic phenomenon: History and review of the literature. Hautarzt 2003;54:274-8.
[Google Scholar]
|
| 26. |
Thappa DM. The isomorphic phenomenon of Koebner. Indian J Dermatol Venereol Leprol 2004;70:187-9.
[Google Scholar]
|
| 27. |
Morsy TA, Arafa MA, Younis TA, Mahmoud IA. Studies on Paederus alfierii Koch (Coleoptera:Staphylinidae) with special reference to the medical importance. J Egypt Soc Parasitol 1996;26:337-51.
[Google Scholar]
|
| 28. |
Singh G, Yousuf Ali S. Paederus dermatitis. Indian J Dermatol Venereol Leprol 2007;73:13-5.
[Google Scholar]
|
| 29. |
Zargari O, Kimyai-Asadi A, Fathalikhani F, Panahi M. Paederus dermatitis in northern Iran: A report of 156 cases. Int J Dermatol 2003;42:608-12.
[Google Scholar]
|
| 30. |
Anstey AV. Disorders of skin colour. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8 th ed. Oxford: Wiley Blackwell; 2010. p. 58.32.
th ed. Oxford: Wiley Blackwell; 2010. p. 58.32.'>[Google Scholar]
|
| 31. |
Adams SP. Dermacase: Phytophotodermatitis. Can Fam Physician 1998;44:503,509.
[Google Scholar]
|
| 32. |
James WD, Berger TG, Elston DM, editors. Pruritus and neurocutaneous dermatoses. In: Andrews' Diseases of the Skin Clinical Dermatology. 10 th ed. Philadelphia: Saunders Elsevier; 2006. p. 61.
th ed. Philadelphia: Saunders Elsevier; 2006. p. 61.'>[Google Scholar]
|
| 33. |
Tomoviæ M, Skiljeviæ D, Zivanoviæ D, Tanasiloviæ S, Vesiæ S, Dakoviæ Z, et al . Two cases of probable endogenous extensive cutaneous larva migrans in Serbia. Acta Dermatovenerol Alp Panonica Adriat 2008;17:37-40.
[Google Scholar]
|
Fulltext Views
49,745
PDF downloads
7,112





