Translate this page into:
Linear orofacial lichen sclerosus
Correspondence Address:
Yongfeng Chen
Dermatology Hospital, Southern Medical University, Guangdong Provincial Dermatology Hospital, Lujing Road, No. 2, Guangdong 510091
China
| How to cite this article: Zhang J, Xue R, Lin E, Pan H, Chen Y. Linear orofacial lichen sclerosus. Indian J Dermatol Venereol Leprol 2018;84:197-199 |
Sir,
Lichen sclerosus is a chronic mucocutaneous inflammatory disorder that preferentially affects female genitalia. It is characterized clinically by atrophic papules or plaques, occurring most commonly in the anogenital area. Oral lesions of lichen sclerosus are rare and appear as demarcated, whitish, smooth plaques similar to those affecting genitalia.
A 22-year-old Chinese male presented with a 3-months history of a smooth band-like depigmented midline orofacial plaque. Originally, the lesion had appeared just on the left nostril and slowly progressed downward in a linear pattern to involve the upper labial and gingival mucosa. The lesion was completely asymptomatic and he had not received any treatment. He denied history of alcoholism, smoking, trauma, and familial occurrence of similar disease. There was no evidence of genital or skin lesion.
Cutaneous examination revealed a smooth, depigmented, shiny, well-defined plaque without atrophy beneath the left side of the nose in a linear pattern [Figure - 1]a. The lesion originated in the left nostril, extended over the vermillion border, labial mucosa and the gingival margin, and ended at the left upper incisor [Figure - 1]b. The lesion involved the labial mucosa and appeared as reddish areas with mild erosion. The teeth present in the involved region did not show any mobility. Oral hygiene was good.
 |
| Figure 1a: Depigmented macule originates in the left nostril and upper lip |
 |
| Figure 1b: Whitish patches extend over the labial mucosa, gingival, and end at the left upper incisor with mild erosion |
According to the clinical features, lichen sclerosus, lichen planus, and vitiligo were considered. A biopsy from the labial mucosa revealed atrophic epithelium, focal parakeratosis, basal cell vacuolization, and upper dermal edema and hyalinization of dermal collagen along with band-like lymphocytic infiltration [Figure - 2]. Direct immunofluorescence test was negative. Laboratory examination including routine blood test, serum anti-nuclear antibodies, rheumatoid factor, and serum complements were within normal range. These findings were consistent with the diagnosis of linear orofacial lichen sclerosus. Unfortunately, the patient refused any treatment and was lost to follow-up.
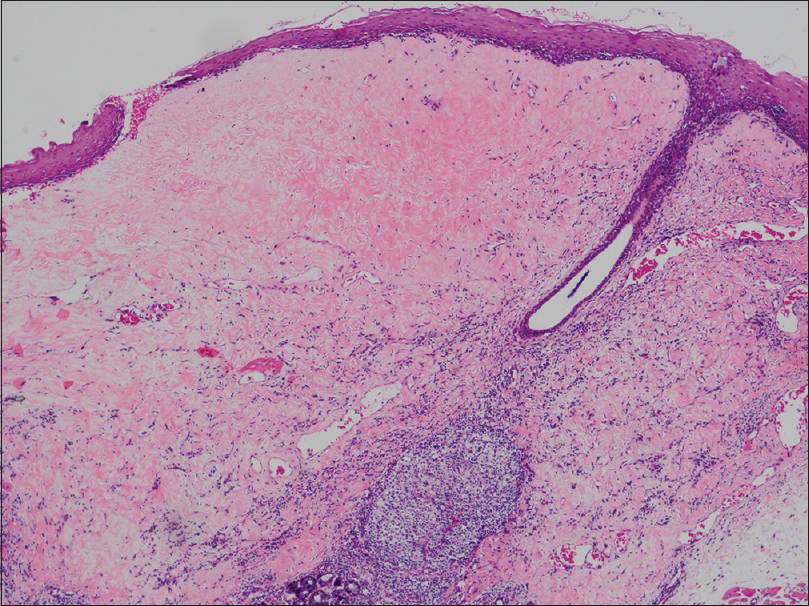 |
| Figure 2a: Atrophic epithelium, focal parakeratosis, basal cell vacuolization, and upper dermal edema and hyalinization of dermal collagen along with band-like lymphocytic infiltration (H and E, ×100) |
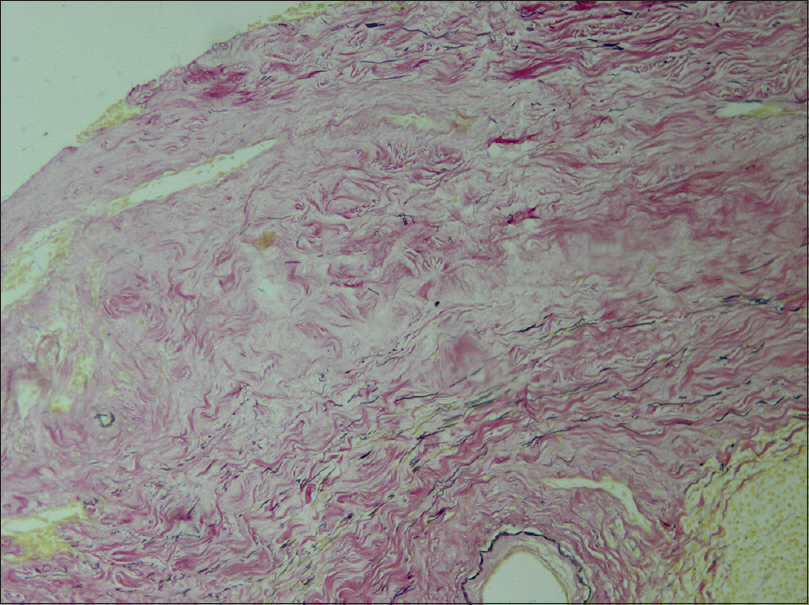 |
| Figure 2b: Scarce elastic fibers in the hyalinized area (Verhoff's stain, ×100) |
Lichen sclerosus is an uncommon mucocutaneous disease preferentially affecting the anogenital areas of females, rarely involving the oral mucosa.[1] Kaur et al. and Walsh et al., respectively, reported a case of linear orofacial lichen sclerosus in 2002 and 2008.[2],[3] All these cases along with our present case of orofacial lichen sclerosus showed a similar course with the first lesion originating in or beneath the nose and slowly progressing downward in a linear form to involve the upper lip, labial, and gingival mucosa. We were unable to find any previous reports of linear orofacial lichen sclerosus in China.
According to literature reports, the lip, labial mucosa and buccal mucosa are the most common intraoral sites affected.[4],[5],[6] Differentiation between morphea/scleroderma and lichen sclerosus. presents a clinical challenge because both conditions may present as white, sclerotic and indurated plaques. However, the pathological changes in morphoea/scleroderma occur especially in the deep dermis, in contrast to the superficial dermis in lichen sclerosus. Elastic fibers are normal in morphea/scleroderma but are scanty or lost in lichen sclerosus; moreover, collagen synthesis increases in morphea/scleroderma while reducing in lichen sclerosus. So, the case is lichen sclerosus rather than morphea/scleroderma or the overlapping entities. The microscopic features of oral lichen sclerosus can be used to distinguish oral lichen sclerosus from oral lichen planus, oral submucous fibrosis, oral scleroderma, and oral mucosal vitiligo.
Since the majority of the patients are asymptomatic, treatment of oral lichen sclerosus is unnecessary. Topical corticosteroid and calcineurin inhibitors (tacrolimus and pimecrolimus) may be considered as preferred treatments when patients have requirements.[7]
In conclusion, oral lichen sclerosus is a rare manifestation of a mucocutaneous disorder with a predilection for oral mucosa. Notwithstanding that lesions may be asymptomatic, malignant transformation in oral lichen sclerosus has not been reported. Long-term follow-up is necessary. Treatment of patients with oral lichen sclerosus should be decided on an individual basis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Meffert JJ, Davis BM, Grimwood RE. Lichen sclerosus. J Am Acad Dermatol 1995;32:393-416.
[Google Scholar]
|
| 2. |
Kaur S, Thami GP, Kanwar AJ, Mohan H. Linear oro-facial lichen sclerosus. Clin Exp Dermatol 2002;27:467-70.
[Google Scholar]
|
| 3. |
Walsh SN, Jorizzo JL, Haverstock C, Sangüeza OP. A linear orofacial macule. Am J Dermatopathol 2008;30:194-5.
[Google Scholar]
|
| 4. |
Azevedo RS, Romañach MJ, de Almeida OP, Mosqueda-Taylor A, Vega-Memije ME, Carlos-Bregni R, et al. Lichen sclerosus of the oral mucosa: Clinicopathological features of six cases. Int J Oral Maxillofac Surg 2009;38:855-60.
[Google Scholar]
|
| 5. |
Sherlin HJ, Ramalingam K, Natesan A, Ramani P, Premkumar P, Thiruvenkadam C. Lichen sclerosus of the oral cavity. Case report and review of literature. J Dermatol Case Rep 2010;4:38-43.
[Google Scholar]
|
| 6. |
Attili VR, Attili SK. Lichen sclerosus of lips: a clinical and histopathologic study of 27 cases. Int J Dermatol 2010;49:520-5.
[Google Scholar]
|
| 7. |
Kirtschig G, Becker K, Günthert A, Jasaitiene D, Cooper S, Chi CC, et al. Evidence-based (S3) guideline on (anogenital) lichen sclerosus. J Eur Acad Dermatol Venereol 2015;29:e1-43.
[Google Scholar]
|
Fulltext Views
5,218
PDF downloads
1,678





