Translate this page into:
Lionfish envenomation: Relapses controlled by intralesional triamcinolone
2 Department of Dermatology, Maidstone and Tunbridge Wells NHS Trust and Medway Hospitals NHS Trust, Kent, United Kingdom
Correspondence Address:
Lianne Thomas
Borough Green Dermatology Department, Quarry Hill Road, Borough Green, Kent, TN15 8RQ
United Kingdom
| How to cite this article: Thomas L, Tharakaram S. Lionfish envenomation: Relapses controlled by intralesional triamcinolone. Indian J Dermatol Venereol Leprol 2016;82:438-439 |
Sir,
A 44-year-old woman returned to the United Kingdom from a vacation in Egypt with an erythematous eruption on her limbs. While snorkeling along a coral reef, she had been stung on her forearms, thighs, and legs by several lionfish [Figure - 1]. Subsequently, these areas had become red and swollen with an associated burning sensation. She had no past medical history of note and denied any current medications or allergies. On return to the United Kingdom, her initial treatment comprised of oral flucloxacillin and chlorphenamine which did not result in any improvement. Three weeks later, she presented to our dermatology clinic with some urticated, tender nodules and plaques on her limbs [Figure - 2].
 |
| Figure 1: Lionfish |
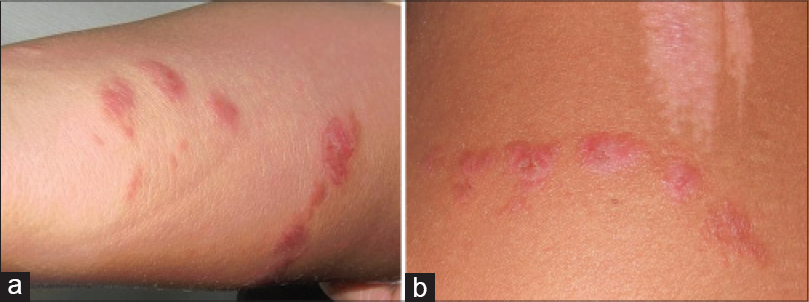 |
| Figure 2: (a) Urticated plaques on arm following lionfish stings. (b) Urticated plaques on thigh with associated white area following abrasion on coral |
Haematological and blood chemistry parameters were normal. A skin biopsy showed acanthosis, spongiosis with scattered eosinophils and exocytosis of lymphocytes. In the superficial and deep dermis, there were perivascular and interstitial mixed cell infiltrates composed of lymphocytes, histiocytes, numerous eosinophils and a few larger, more atypical lymphoid cells likely to represent activated T-cells [Figure - 3]. These histological features favored the diagnosis of reaction to a sting.
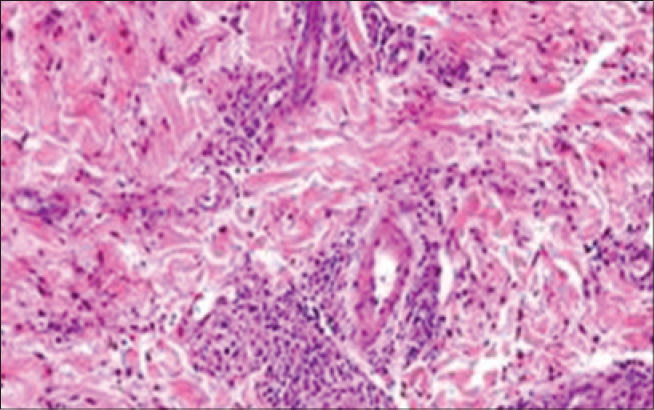 |
| Figure 3: Biopsy of an urticated plaque showing a perivascular infiltrate with many eosinophils in the mid-dermis (H and E, ×200) |
She was treated with oral prednisolone in a dose of 30 mg/day, tapered over 4 weeks along with topical clobetasol propionate ointment, applied twice daily on the affected areas. This was followed by a steady clinical improvement and moderate resolution of the lesions. Initially, she suffered relapses every 2–3 months and these were controlled by intralesional triamcinolone injections, 10 mg/ml. Slowly, the interval between relapses became longer and she has remained in remission for 3 years to date.
Marine sports such as snorkeling can lead to hazardous encounters with marine life. The lionfish (Pterois volitans) is a member of the family Scorpaenidae, a venomous fish inhabiting tropical waters. When provoked, the spines of these fish inject venom which may cause pain locally. There may also be bleeding from the mechanical entry of fish spines into the skin and an inflammatory reaction to the pieces of the spine left in the skin. Lionfish spine extract contains acetylcholine and is a toxin affecting neuromuscular transmission.[1]
Systemic effects of lionfish envenomation are related to the amount of venom injected. Nausea, sweating, dyspnea, abdominal pain, weakness, hypotension, syncope and chills are the more common systemic symptoms.[2],[3] In a published series of 101 cases of lionfish stings, 92% of patients experienced local pain, 60% local oedema and 13% systemic symptoms.[4]
The immediate step to be taken following a lionfish sting is to inactivate the proteinaceous venom by placing the affected site in hot (up to 45°C) water for 30–90 min or until pain improves.[1] This treatment theoretically inactivates or destroys the heat-labile components of the venom in vivo. Local anesthetics, antihistamines, oral and topical steroids and oral antibiotics are given as and when required.
Scorpaenidae is second only to stingrays in the estimated 40,000–50,000 marine fish envenomations that occur worldwide annually.[5] We can expect to see increasing numbers of lionfish envenomations on both sides of the Atlantic and with increasing global travel, dermatologists need to be aware of the presentation of this condition. Our case highlights that lionfish stings often follow a relapsing and remitting course and that relapses can be controlled with intralesional triamcinolone.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Vetrano SJ, Lebowitz JB, Marcus S. Lionfish envenomation. J Emerg Med 2002;23:379-82.
[Google Scholar]
|
| 2. |
Trestrail JH 3rd, al-Mahasneh QM. Lionfish string experiences of an inland poison center: A retrospective study of 23 cases. Vet Hum Toxicol 1989;31:173-5.
[Google Scholar]
|
| 3. |
Kizer KW, McKinney HE, Auerbach PS. Scorpaenidae envenomation. A five-year poison center experience. JAMA 1985;253:807-10.
[Google Scholar]
|
| 4. |
Gallagher SA. Lionfish and stonefish. E Med Journal 2001; 2-7.
[Google Scholar]
|
| 5. |
Auerbach PS, McKinney HE, Rees RS, Heggers JP. Analysis of vesicle fluid following the sting of the lionfish Pterois volitans. Toxicon 1987;25:1350-3.
[Google Scholar]
|
Fulltext Views
1,809
PDF downloads
1,625





