Translate this page into:
Lip swelling: An unusual presentation of post kala-azar dermal leishmaniasis
2 Department of Dermatology, All Institute of Medical Sciences, Patna, Bihar, India
3 Department of Dermatology, KPC Medical College and Hospital, Kolkata, West Bengal, India
Correspondence Address:
Piyush Kumar
Department of Dermatology, Katihar Medical College, Katihar, Bihar
India
| How to cite this article: Kumar P, Jha A, Das A. Lip swelling: An unusual presentation of post kala-azar dermal leishmaniasis. Indian J Dermatol Venereol Leprol 2017;83:136 |
Sir,
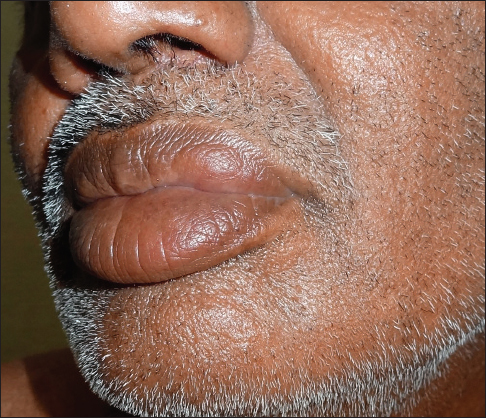
A 55-year-old otherwise healthy man presented with an asymptomatic, gradually increasing, firm, non-tender localized swelling affecting the left half of the upper lip for the preceding 8 months [Figure - 1]a. There were no surface changes and the cervical lymph nodes were unremarkable. In the recent past, he had also developed many hypopigmented lesions on the trunk which were diagnosed as pityriasis versicolor by a physician and was treated with antifungals, without any improvement. Multiple hypopigmented macules, coalescing to form patches were seen over the trunk [Figure - 1]a. There was no sensory loss over the hypopigmented lesions or elsewhere and none of the peripheral nerves were thickened. A provisional diagnosis of granulomatous cheilitis was considered for the lip lesion and a biopsy was performed for confirmation. Histopathologic examination showed an atrophic epidermis and a diffuse dense infiltrate of lymphocytes, plasma cells and macrophages involving the upper and mid-dermis [Figure - 2]a. Many of the macrophages contained tiny, slightly basophilic, intracytoplasmic dots of size 1–2 microns, suggesting Leishman–Donovan bodies [Figure - 2]b. Based on the clinicpathological findings, a diagnosis of post kala-azar dermal leishmaniasis was made.
 |
| Figure 1a: Multiple hypopigmented macules coalescing to form patches on trunk |
 |
| Figure 1b: Resolution of the lip lesion, 3 months after treatment with miltefosine |
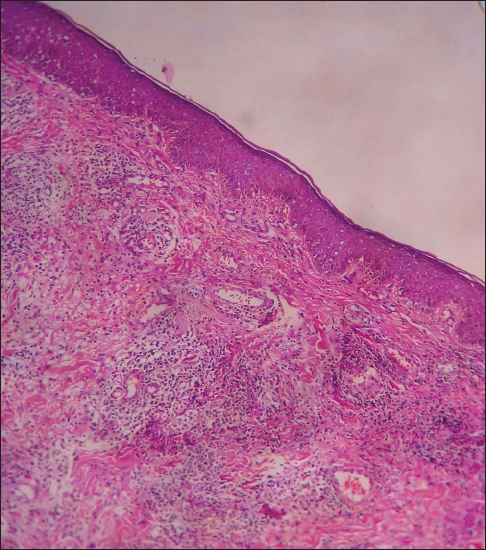 |
| Figure 2a: Atrophic epidermis and dense infiltration of lymphocytes, plasma cells and macrophages in upper dermis (H and E, ×100) |
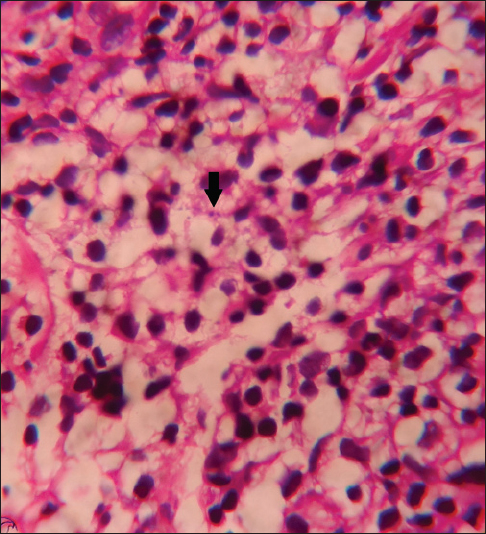 |
| Figure 2b: Leishman–Donovan body (Arrow) (H and E, ×1000) |
The patient was specifically probed for a history of kala-azar. He remembered having prolonged fever 15 years back for which he was treated with some injections after which the fever subsided. We treated him with oral miltefosine, 50 mg twice daily for 28 days, available under the national vector-borne diseases control programme in India. Following treatment for 28 days, the lip lesion showed significant improvement but resolution was incomplete. Treatment was continued for another 2 months followed by almost complete subsidence of the lesion [Figure - 1]b.
Post kala-azar dermal leishmaniasis is a late cutaneous manifestation of visceral leishmaniasis caused by Leishmania donovani and is seen in 5–15% of visceral leishmaniasis cases in India.[1] The interval between the occurrence of kala-azar and post kala-azar dermal leishmaniasis ranges from 1 to 20 years (mean 6.2 years) in Indian post kala-azar dermal leishmaniasis, unlike African post kala-azar dermal leishmaniasis that usually develops some months to a year following visceral leishmaniasis.[2] In endemic areas, mucosal involvement can occur as granulomatous nodules on the angles of mouth, dorsum of tongue, buccal mucosa or soft palate.[3] In addition, mucosal leishmaniasis may affect the upper respiratory tract and/or oral mucosa leading to ulcerations, mainly in the hard or soft palate.[3]
Demonstration of parasites in slit-skin smear or by tissue culture is considered to be the gold standard, but such methods are invasive and less sensitive (58%) because of the low parasite burden and thus, not feasible in field conditions.[1] On the contrary, the recent availability of rapid serodiagnostic tools such as rK39 has revolutionized the diagnosis of visceral leishmaniasis as well as post kala-azar dermal leishmaniasis. The test has a sensitivity of around 95% for polymorphic post kala-azar dermal leishmaniasis and 78% for the macular variety.[4] Histopathology from the lesion is diagnostic and usually shows an infiltrate of chronic inflammatory cells with variable numbers of amastigotes in dermal macrophages.[1]
The synthetic phospholipid derivative, miltefosine, has been tried in different doses and duration for the treatment of post kala-azar dermal leishmaniasis. There has been a report on the efficacy of miltefosine at a higher dose of 50 mg thrice daily for 60 days (with a need to extend for 90 days if required) in a small number of patients of post kala-azar dermal leishmaniasis from Bangladesh.[5] Amphotericin B as a monotherapy and in combination has been found to be effective in doses of 5–20 mg/kg.[6]
To conclude, the index of suspicion for post kala-azar dermal leishmaniasis should be high in an endemic area, as atypical presentations are not uncommon.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Salotra P, Singh R. Challenges in the diagnosis of post kala-azar dermal leishmaniasis. Indian J Med Res 2006;123:295-310.
[Google Scholar]
|
| 2. |
Zijlstra EE, Musa AM, Khalil EA, el-Hassan IM, el-Hassan AM. Post-kala-azar dermal leishmaniasis. Lancet Infect Dis 2003;3:87-98.
[Google Scholar]
|
| 3. |
Motta AC, Lopes MA, Ito FA, Carlos-Bregni R, de Almeida OP, Roselino AM. Oral leishmaniasis: A clinicopathological study of 11 cases. Oral Dis 2007;13:335-40.
[Google Scholar]
|
| 4. |
Salotra P, Sreenivas G, Ramesh V, Sundar S. A simple and sensitive test for field diagnosis of post kala-azar dermal leishmaniasis. Br J Dermatol 2001;145:630-2.
[Google Scholar]
|
| 5. |
Ramesh V, Katara GK, Verma S, Salotra P. Miltefosine as an effective choice in the treatment of post-kala-azar dermal leishmaniasis. Br J Dermatol 2011;165:411-4.
[Google Scholar]
|
| 6. |
Sundar S, Sinha PK, Rai M, Verma DK, Nawin K, Alam S, et al. Comparison of short-course multidrug treatment with standard therapy for visceral leishmaniasis in India:An open-label, non-inferiority, randomised controlled trial. Lancet 2011;377:477-86.
[Google Scholar]
|
Fulltext Views
2,228
PDF downloads
2,482





