Translate this page into:
Lipoid proteinosis
Correspondence Address:
Angoori Gnaneshwar Rao
F12, B8, HIG-2 APHB, Baghlingampally, Hyderabad - 500 044, Telangana
India
| How to cite this article: Rao AG, Koppada D. Lipoid proteinosis. Indian J Dermatol Venereol Leprol 2015;81:549 |
Sir,
Lipoid proteinosis (Urbach and Wiethe disease), a rare genodermatosis inherited autosomal recessive trait, was first described in 1929. It occurs due to mutations in the extracellular matrix gene 1 on chromosome 1q21 though its exact role is unclear. Nonetheless, Kowalewski et al. have postulated that extracellular matrix gene 1 glycoprotein plays an important role in regulating blood physiology and anatomy of the skin, as evidenced by gross alteration in the microvasculature of mid- and deep dermis in their study on patients with lipoid proteinosis. [1] So far, 26 different inherited mutations in the extracellular matrix gene 1 have been reported in lipoid proteinosis. Among them, mutations of exon 6 result in severe clinical manifestations, while exon 7 mutations display mild features. [2] Around 300 cases have been reported in the literature; 25% of them are from South Africa and many of them are of Dutch or German ancestry. [3]
A 30-year-old male, born of a consanguineous marriage, presented with thickening and disfigurement of face since childhood and hoarseness of voice and convulsions for the last 1-year. No one else in the family had similar complaints. He was diabetic and epileptic and was on regular treatment for the last 1 year. He was apparently normal at birth but subsequently started developing scars initially involving the face and later involving the trunk and upper and lower limbs. Cutaneous examination revealed firm, knobby papules distributed on the upper and lower eyelids (moniliform papules) and lid margins. Facial skin was waxy and there were multiple papules and varioliform scars of varying sizes and shapes [Figure - 1]a. There were multiple papules and plaques on both lips and angles of the mouth and his tongue was woody with erosions and indentations [Figure - 1]b. Hyperkeratotic papules and plaques were distributed on both elbows, knees, scrotum and natal cleft [Figure - 1]c. Palms and soles showed keratoderma. There were multiple, well-defined, oval atrophic scars on the back of [Figure - 1]d. He was provisionally diagnosed as having lipoid proteinosis. Erythropoietic protoporphyria and systemic amyloidosis were considered in the differential diagnosis. Direct laryngoscopy showed bulky, pear-shaped arytenoids and fleshy deposits on the palate and vocal cords with restricted movement [Figure - 2]a. Computed tomography of brain showed bilateral temporal bean-shaped calcifications [Figure - 2]b. Skin biopsy from the plaque on the right elbow showed hyaline material in the dermis surrounding blood vessels and adnexal structures, which was Periodic acid-Schiff positive and diastase resistant [Figure - 2]c and d and negative with Congo red, confirming the diagnosis of lipoid proteinosis. It was clinically differentiated from erythropoietic protoporphyria as there were oral lesions and there was no photosensitivity nor involvement of sun-exposed areas. Histopathologically, in erythropoietic protoporphyria, the deposition of periodic acid-Schiff positive material is less dense around the blood vessels and not seen around the sweat gland coils.
 |
| Figure 1: (a) Knobby papules (moniliform papules) on upper and lower eye lid margins. Skin around the eye is waxy with multiple papules and varioliform scars, (b) Multiple papules and plaques on both lips, angles of mouth, and woody tongue with erosions and indentations, (c) Hyperkeratotic papules, nodules, and plaques on both elbows, (d) Multiple well-defined oval atrophic scars on the back of trunk |
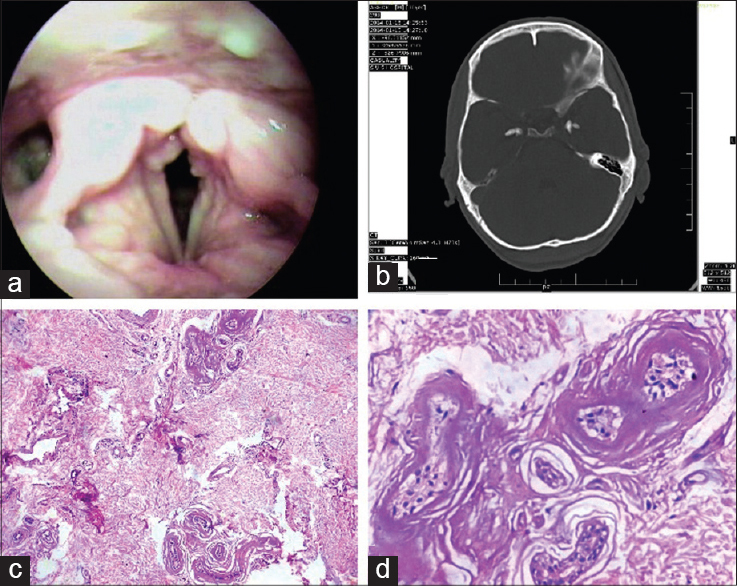 |
| Figure 2: (a) Bulky pear-shaped arytenoids and fleshy deposits on vocal cords and palate visualized on direct laryngoscopy, (b) Axial plain computed tomography of brain showing bean-shaped bilateral, symmetrical calcification on the anterior and medial aspects of both temporal horns, (c) Periodic acid– Schiff (PAS)-positive, diastase-resistant hyaline material in the dermis with dilated capillaries and around blood vessels and adnexal structures (H and E with PAS 100×), (d) PAS-positive, diastase-resistant hyaline material in the dermis and surrounding adnexal structures (H and E with PAS, 400×) |
Lipoid proteinosis presents with varied clinical manifestations involving multiple systems; however, skin and mucous membranes of the respiratory and digestive systems are primarily affected. The basic pathology is the deposition of periodic acid-Schiff-positive hyaline-like material in the dermis, around blood vessels and adnexae with resultant skin thickening, abnormal scarring, abnormal wound healing and premature aging. Onset of lipoid proteinosis is usually in early infancy, heralded by hoarseness of voice due to laryngeal infiltration. [4] This should alert the physician particularly when encountered in early childhood. Our patient had hoarseness of voice since childhood in the and direct laryngoscopy confirmed the presence of fleshy deposits on the palate and vocal cords with restricted movement. Diffuse infiltration of the pharynx and larynx may cause respiratory distress, at times requiring tracheostomy. Lung and bronchial involvement was also reported in lipoid proteinosis. [5] Diffuse skin infiltration leads to yellowish or waxy papules on knuckles, elbows and knees which are followed by nodules or plaques or pock-like scars, as were evident our patient. [6] The eye may be involved in lipoid proteinosis due to infiltration of the trabeculum and ocular manifestations include corneal opacities and secondary glaucoma. [7] Various neurological manifestations have been described in the literature including epilepsy, schizophrenia and memory loss. [8] Our patient also demonstrated neurological involvement in the form of epilepsy accompanied by bilateral bean-shaped temporal calcification on computed tomography of brain. Moreover, Shivaswamy et al., while reporting lipoid proteinosis in two siblings have also documented bean-shaped calcification in suprasellar area in the elder sibling. [9] Similarly, calcification in limbic area was also reported by Kumar et al. in a 17-year-old patient of lipoid proteinosis. [10] Association of diabetes mellitus has been reported in lipoid proteinosis, as noted in our patient, and it was postulated that diabetes in lipoid proteinosis is due to deposition of amorphous material in the capillary vessels or in pancreas. [11] Similarly, deposition of hyaline material in the intestine may cause intestinal bleeding. There is no effective treatment and there are no large case series to evaluate therapeutic options.
However, anecdotal reports suggest short-lived satisfactory results with dimethyl sulfoxide, [12] acetretin, [13] etretinate, [14] D-pencillamine, [15] dermabrasion, and carbondioxide laser surgery (for vocal cords and beaded papules). Life expectancy is usually normal, barring infrequent attacks of respiratory obstruction that rarely require tracheostomy. [16] Parents of affected children should be counseled regarding the risk of having other affected offspring.
| 1. |
Kowalewski C, Kozłowska A, Chan I, Górska M, WoŸniak K, Jabłoñska S, et al. Three-dimensional imaging reveals major changes in skin microvasculature in lipoid proteinosis and lichen sclerosus. J Dermatol Sci 2005;38:215-24.
[Google Scholar]
|
| 2. |
Hamada T, Wessagowit V, South AP, Ashton GH, Chan I, Oyama N, et al. Extracellular matrix protein 1 gene (ECM1) mutations in lipoid proteinosis and genotype phenotype correlation. J Invest Dermatol 2003;120:345-50.
[Google Scholar]
|
| 3. |
Heyl T. Geological study of lipoid proteinosis in South Africa. Br J Dermatol 1970;83:338-40.
[Google Scholar]
|
| 4. |
Bergenholtz A, Hofer PA, Ohman J. Oral, pharyngeal and laryngeal manifestations in Urbach-Wiethe disease. Ann Clin Res 1977;9:1-7.
[Google Scholar]
|
| 5. |
Al-Bitar Y, Samdani AJ. Lipoid proteinosis in two brothers with multiple organ involvement from Saudi Arabia. Int J Dermatol 2004;43:360-1.
[Google Scholar]
|
| 6. |
Galadari I, Al-Kuwaiti R. Lipoid proteinosis: A case report. Int J Dermatol 2004;43:368-70.
[Google Scholar]
|
| 7. |
François J, Bacskulin J, Follmann P. Ocular manifestations of the Urbach-Wiethe Syndrome. Hyalitis of the skin and the mucosa. Opthalmologica 1968;155:433-48.
[Google Scholar]
|
| 8. |
Kleinert R, Cervos-Navarro J, Kleinert G, Walter GF, Steiner H. Predominantly cerebral manifestation in Urbach-Wiethe′s syndrome (lipoid proteinosis cutis et mucosae): A clinical and pathomorphological study. Clin Neuropathol 1987;6:43-5.
[Google Scholar]
|
| 9. |
Shivaswamy KN, Thappa DM, Laxmisha C, Jayanthi S. Lipoid proteinosis in two siblings: A report from south India. Dermatol Online J 2003;9:12.
[Google Scholar]
|
| 10. |
Kumar AS, Seetharam KA, Singh MK, Neena V. Lipoid proteinosis. Indian J Dermatol Venereol Leprol 1986;52:95-8.
[Google Scholar]
|
| 11. |
Deniz KG, Alpaslan T, Mithat B, Mzeyyen Y, Sedat A, Selver Z, et al. Possible mechanism of diabetes mellitus may be result of the diffuse deposition of amorphous material into the capillary vessels or in pancreas. Turk J Endocrinol Metabol 2009;13:60.
[Google Scholar]
|
| 12. |
Wong CK, Lin CS. Remarkable response of lipoid proteinosis to oral dimethyl sulfoxide. Br J Dermatol 1988;119:541-4.
[Google Scholar]
|
| 13. |
Toosi S, Ehsani AH. Treatment of lipoid proteinosis with acitretin: A case report. J Eur Acad Dermatol Venereol 2009;23:482-3.
[Google Scholar]
|
| 14. |
Gruber F, Manestar D, Stasic A, Grgurevic Z. Treatment of lipoid proteinosis with Etretinate. Acta Derm Venereol 1996;76:154-5.
[Google Scholar]
|
| 15. |
Kaya TI, Kokturk A, Tursen U, Ikizoglu G, Polat A. D-penicillamine treatment for lipoid proteinosis. Pediatr Dermatol 2002;19:359-62.
[Google Scholar]
|
| 16. |
Hamada T. Lipoid proteinosis. Clin Exp Dermatol 2002;27:624-9.
[Google Scholar]
|
Fulltext Views
6,531
PDF downloads
2,796





