Translate this page into:
Livedo reticularis after intra-articular hyaluronic acid injection
Correspondence Address:
Sara Leite de Azevedo Campos
Avenida Amália Rodrigues, n° 28, 3° Direito, 2870-073, Montijo
Portugal
| How to cite this article: de Azevedo Campos SL, Brasileiro A, João A, Lopes MJ. Livedo reticularis after intra-articular hyaluronic acid injection. Indian J Dermatol Venereol Leprol 2017;83:602-603 |
Sir,
Hyaluronic acid is a glycosaminoglycan. At high molecular weight it is viscoelastic and provides lubrication for joints.[1] Given its characteristics, intra-articular injections of hyaluronic acid are used to treat osteoarthritis.[2],[3]
Adverse events likely to be associated with the intra-articular injection are rare, benign and temporary. These include local effusion, arthralgia, warmth and erythema.[3] A rare yet potentially serious complication of intra-articular hyaluronic acid is livedo reticularis with tissue necrosis.[1]
A 74-year-old man presented with a 10-day history of painful skin eruption on the left knee. The eruption developed 1 week after intra-articular hyaluronic acid injections on both knees for treatment of osteoarthritis. Examination revealed a blanchable erythematous reticulate patch on the left knee with a violaceous center [Figure - 1]. The right knee was normal. Doppler ultrasonography and blood analysis revealed no pathological findings. A punch biopsy of the skin was performed. Histopathological examination showed an amorphous basophilic foreign material consistent with hyaluronic acid present within the vessels of the dermis and hypodermis with associated thrombus formation [Figure - 2] and [Figure - 3]. With a clinical and histological correlation, a diagnosis of livedo reticularis due to intra-articular hyaluronic acid injection entering the cutaneous vasculature was confirmed. Since there was no evidence of necrosis, the patient was advised rest and treated conservatively with analgesic. The lesion resolved after 4 weeks.
 |
| Figure 1: Livedo reticularis on the left knee with a violaceous center |
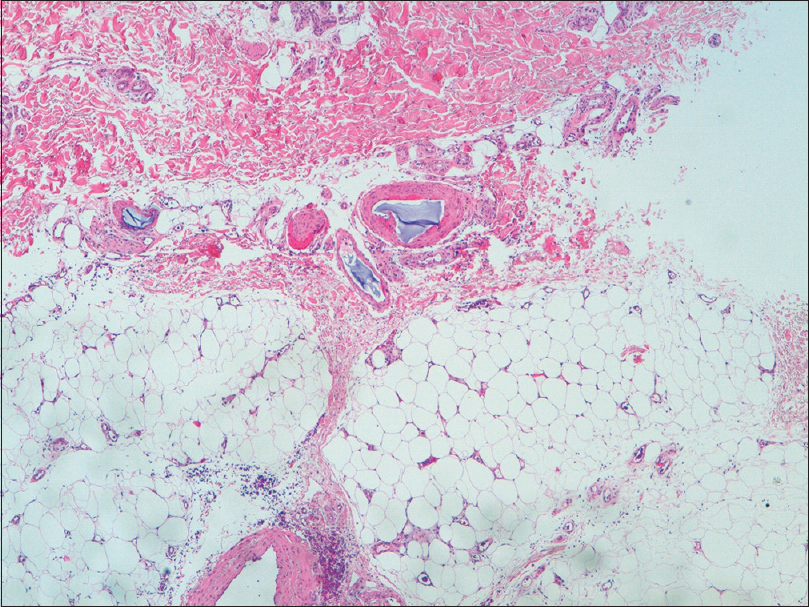 |
| Figure 2: Foreign material consistent with hyaluronic acid within the vessels of the dermis and hypodermis (H and E, ×400) |
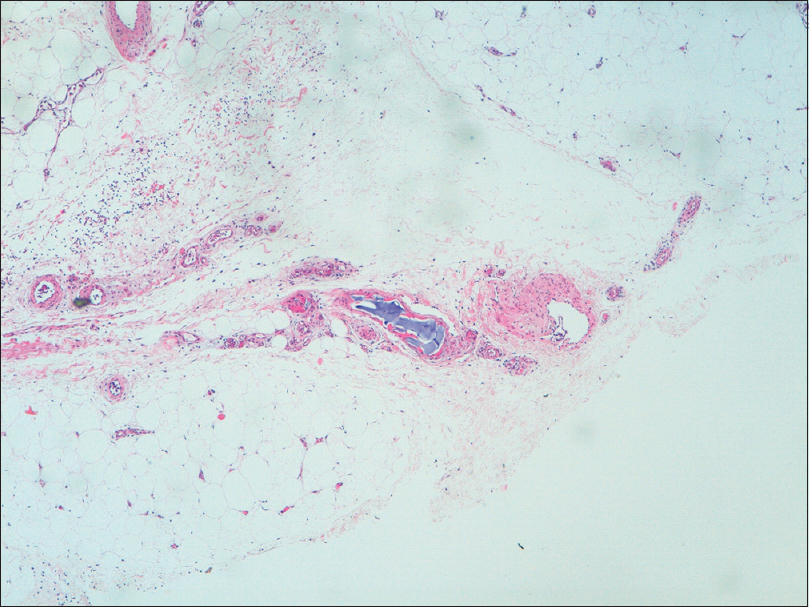 |
| Figure 3: Hyaluronic acid inside blood vessels of the hypodermis with an associated thrombus forming (H and E, ×400) |
Our patient presented with livedo reticularis without skin necrosis, at the site of intra-articular hyaluronic acid knee injection taken 1 week prior to the onset of lesions. In literature, we found only two case reports of skin necrosis following intra-articular hyaluronic acid injection.[1],[2]
Kim and Alhusayendescribed a case of a 64-year-old man with livedoid epidermal necrosis on the right knee that developed 48 hours after intra-articular hyaluronic acid injections on both knees for treatment of osteoarthritis. The histology revealed atrophic epidermis with patchy necrosis and in the dermis, there was an amorphous basophilic foreign material consistent with hyaluronic acid present within both the dermal stroma and medium-sized vessels with associated thrombus formation. The patient was treated conservatively and the lesion resolved in 4 months.[1]
Borregón-Nofuentes et al. described a similar case in which the lesions of livedo reticularis with two necrotic areas appeared 1 month after intra-articular hyaluronic acid injection.[2]
These two cases had clinical and histologic characteristics of tissue necrosis after intra-articular hyaluronic acid injection, but with different timings of the onset of the lesions. In our case, livedo reticularis appeared 1 week after the injection and there was no tissue necrosis.
The term livedo reticularis refers to a reddish-violet reticular blanchable discoloration of the skin. It is caused by an interruption of blood flow in the dermal arteries, either due to spasm (cold and drugs), inflammation (infection and non-infection vasculitis) or vascular obstruction. Vascular obstruction can, in turn, be caused by thrombosis, embolic events or vessel wall abnormalities and clinically presents as necrosis, ulcers and nodules.[4] It is possible that livedo reticularis/tissue necrosis after intra-articular hyaluronic acid infection and Nicolau syndrome, an iatrogenic cutaneous necrosis due to intramuscular, intra-articular, subcutaneous and intravenous injections of medications, such as vitamin K, nonsteroidal anti-inflammatory drugs and glucocorticoids, share the same pathophysiological mechanism. Although not fully understood, it is plausible that hyaluronic acid limits vascular supply, leading to ischemia. Several explanations have been offered including vasospasm secondary to needle prick, embolization of the injected material or pressure due to the material placed around the vessels.[1]
The authors consider that in this case, as hyaluronic acid was present within the vessels of the dermis and hypodermis, the ischemia was due to wrong injection technique. Hyaluronic acid was either injected into the incorrect anatomic site or it escaped from the joint to the vessels due to rupture by direct injury with subsequent embolization. Although patient predisposition and anatomy should be considered as possible predisposing factors, in some cases, small amounts of hyaluronic acid can escape into the local vasculature after the injection procedure without any skin reaction and can cause findings like in our case. Nonetheless, taking all together, the causality assessment performed as per the Naranjo algorithm revealed the case to be probable (Naranjo score 7).[5]
There is no consensus on the optimal treatment of hyaluronic acid embolism. Low-molecular-weight heparin, heat, topical or intravenous vasodilators (sildenafil, nitroglycerin) and hyaluronidase to hydrolyze and diffuse the injected material have been proposed. Conservative treatment is also an alternative.[1],[2]
To prevent complications of intra-articular hyaluronic acid injections, the physician must be well aware of the relevant anatomy with radiography being recommended for better assessment of the bony anatomy of the individual knee joint. It is also important to know the best approach to a knee injection, namely, the path of least obstruction and maximal access to the synovial cavity, to minimize such adverse eventualities.[1]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kim WB, Alhusayen RO. Skin necrosis from Intra-articular hyaluronic acid injection. J Cutan Med Surg 2015;19:182-4.
[Google Scholar]
|
| 2. |
Borregón-Nofuentes P, Avilés-Izquierdo JA, Martínez-Izquierdo MÃ, Ribé-Bernal L, Pulido-Pérez A, Moya-González MD, et al. Livedo reticularis and skin necrosis due to hyaluronic acid embolism. JAMA Dermatol 2013;149:373-5.
[Google Scholar]
|
| 3. |
Altman RD, Akermark C, Beaulieu AD, Schnitzer T; Durolane International Study Group. Efficacy and safety of a single intra-articular injection of non-animal stabilized hyaluronic acid (NASHA) in patients with osteoarthritis of the knee. Osteoarthritis Cartilage 2004;12:642-9.
[Google Scholar]
|
| 4. |
Herrero C, Guilabert A, Mascaró-Galy JM. Diagnosis and treatment of livedo reticularis on the legs. Actas Dermosifiliogr 2008;99:598-607.
[Google Scholar]
|
| 5. |
Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. Amethod for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981;30:239-45.
[Google Scholar]
|
Fulltext Views
4,910
PDF downloads
1,334





