Translate this page into:
Localized bullous pemphigoid occurring on surgical scars
2 Department of Pathology, Mustafa Kemal University School of Medicine, Hatay, Turkey
Correspondence Address:
Bilge B�lb�l Sen
Department of Dermatology, Mustafa Kemal University, Tayfur Ata Sokmen Medical School, Serinyol, Antakya, Hatay, 31005
Turkey
| How to cite this article: Sen BB, Ekiz �, Rifaioglu EN, Sen T, Atik E, Dogramaci A�. Localized bullous pemphigoid occurring on surgical scars. Indian J Dermatol Venereol Leprol 2013;79:554 |
Sir,
A 39-year-old woman presented with blisters on the old surgical scars for a month. Fifteen years ago she had undergone surgical operation due to a traffic accident. In dermatological examination, there were intact, tense bullae, located linearly along the scars on her legs [Figure - 1]. Nikolsky phenomenon was negative. There were no bullae in any other mucocutaneous site. No milia were seen. Histopathological examination of the biopsy revealed subepidermal separation and bullous formation. There were abundant neutrophils and eosinophils in bullae [Figure - 2]. In dermis, dilated vessels and perivascular chronic inflammatory cell infiltration and less neutrophils and eosinophils were seen. Direct immunofluorescence showed linear complement C3 deposition at the epidermal basement membrane [Figure - 3]. IgG, IgA, IgM, and fibrinogen were negative. According to these signs, bullous pemphigoid (BP) was diagnosed. The patient was treated with 0.05% clobetasol propionate cream and her lesions disappeared and no new lesions were observed.
 |
| Figure 1: (a, b) Tense bullae along the scars |
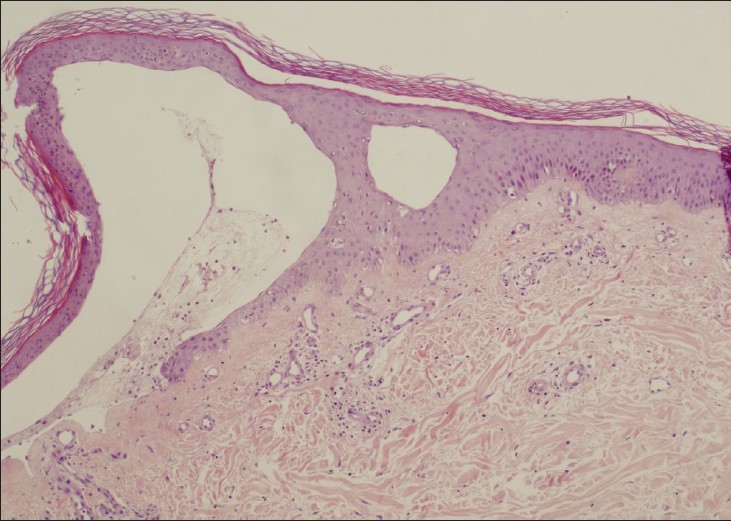 |
| Figure 2: Subepidermal bulla with eosinophils (H and E, ×100) |
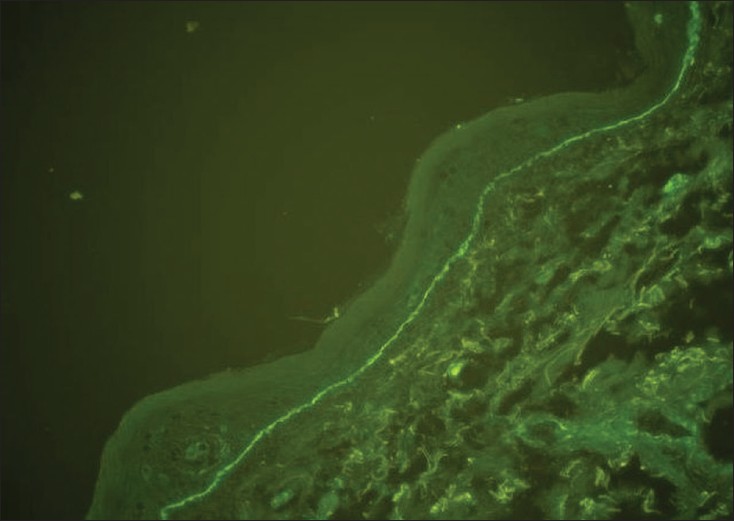 |
| Figure 3: Linear complement C3 deposition along the dermoepidermal junction in direct immunofluorescence examination (×200) |
BP is an acquired, chronic, autoimmune skin disease with itchy generalized bullous lesions that is usually seen in elderly people. Subepidermal bullae are characteristic histological pattern of BP. In patients with or without BP, trauma is one of the triggers for new lesions, which is known as Koebner phenomenon. In the literature, trauma [1],[2] and surgical operation [3],[4] associated BP cases have been rarely reported. Usually, after trauma, localized form of BP can be seen and it has been hypothesized that these triggering factors initiate production of antibodies against basement membrane of previously damaged skin of person prone to BP. [1] However, this issue is still unclear. "Koebnerization" or "isomorphic phenomenon" is defined as occurrence of new lesions after trauma in patients with skin disease. The disease can be pre-existing or newly occurred after trauma. In the emergence of BP, trauma′s role as a real Koebnerization is controversial. [5] However, in BP cases after burns and surgical scars, trauma is supposed to be Koebnerized factor. [3] BP after trauma is generally seen in localized form. However, it can rarely generalize to other parts of the body. [3] In our case, BP was seen on very old surgical scars and remained in localized form. Our case is original because the interval between surgery and the development of BP on the surgical scars was very long. In the literature, the other cases have shorter periods of time between scar formation and development of BP. [3],[4]
In differential diagnosis of localized BP, epidermolysis bullosa acquisita, bullous impetigo, contact dermatitis, bullous lichen planus, pemphigus vulgaris, bullous erythema multi-forme, bullous fixed drug eruption, scabies, radiation dermatitis, and viral causes such as herpes simplex and varicella zoster viruses can be considered. Skin biopsy should be taken in necessary cases. Furthermore, in our case the diagnosis of BP was proved after exclusion of all these diagnoses by the medical history of the patient, histopathological and direct immunofluorescence examination.
The treatment of BP on surgical scar is easier than other forms of BP because of limited disease. Furthermore, in our case, topical steroid was sufficient to treat lesions completely and similar to the literature recurrence was not seen in following 6 months. [2],[3],[4]
As a result, in our case, the lesions were seen 15 years after the operation that reduces the possibility of Koebnerization, so another mechanism may play a role in development of BP on old scars. Furthermore, clinicians should keep in mind the possibility of localized BP in differential diagnosis of bullous lesions on scars.
| 1. |
Macfarlane AW, Verbov JL. Trauma-induced bullous pemphigoid. Clin Exp Dermatol 1989;14:245-9.
[Google Scholar]
|
| 2. |
Yesudian PD, Dobson CM, Ahmad R, Azurdia RM. Trauma-induced bullous pemphigoid around venous access site in a haemodialysis patient. Clin Exp Dermatol 2002;27:70-2.
[Google Scholar]
|
| 3. |
Korfitis C, Gregoriou S, Georgala S, Christofidou E, Danopoulou I. Trauma-induced bullous pemphigoid. Indian J Dermatol Venereol Leprol 2009;75:617-9.
[Google Scholar]
|
| 4. |
Anderson CK, Mowad CM, Goff ME, Pelle MT. Bullous pemphigoid arising in surgical wounds. Br J Dermatol 2001;145:670-2.
[Google Scholar]
|
| 5. |
Thappa DM. The isomorphic phenomenon of Koebner. Indian J Dermatol Venereol Leprol 2004;70:187-9.
[Google Scholar]
|
Fulltext Views
4,888
PDF downloads
3,440





