Translate this page into:
Localized purpuric lesions in a case of classical pityriasis rosea
2 Consultant Dermatologist, Skin Diseases Centre, Nasik, Maharashtra, India
Correspondence Address:
Neha Bhalla
C-904, Crystal Court, Hiranandani Complex, Sector 7, Kharghar, Navi Mumbai - 410 210, Maharashtra
India
| How to cite this article: Bhalla N, Tambe S, Zawar V, Joshi R, Jerajani H. Localized purpuric lesions in a case of classical pityriasis rosea . Indian J Dermatol Venereol Leprol 2014;80:551-553 |
Sir,
Pityriasis rosea is an acute inflammatory self-limiting dermatosis characterized by oval papulo-squamous lesions on the trunk and extremities. Its typical presentation is easily recognized. Many atypical forms are known which may be challenging to diagnose. Purpuric pityriasis rosea is an unusual variant with less than 15 cases reported in English literature. [1] We report a patient with typical pityriasis rosea who developed purpuric lesions during the course of the disease that were confined to the upper extremities.
A 36-year-old male presented with a progressive eruption of mildly itchy erythematous papules and plaques mainly over the trunk with a few lesions on the extremities. Truncal lesions were arranged in a "Christmas tree" pattern and a single herald patch was seen on the medial aspect of the thigh. There was no history of recent upper respiratory tract infection or drug ingestion and there were no prodromal symptoms prior to appearance of the rash. A clinical diagnosis of Pityriasis rosea was made and the patient was prescribed oral erythromycin 500 mg 4 times daily for 7 days along with antihistamines and emollients.
Five days after starting erythromycin, the patient suddenly developed multiple bilaterally symmetrical, mildly itchy, tiny, flat, purpuric lesions over the anteo-medial aspect of both upper limbs [Figure - 1]a and b. The older lesions [Figure - 1]c and d continued to persist. Mucosae, palms, and soles were spared. There was no peripheral lymphadenopathy. Systemic examination was within normal limits. The differential diagnoses of purpuric pityriasis rosea, erythromycin-induced purpura, contact dermatitis and coexistent viral illness causing purpura were considered.
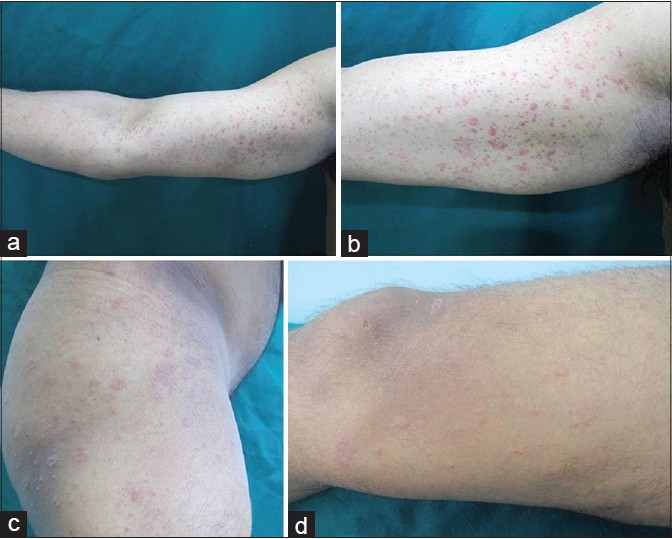 |
| Figure 1: (a and b) Purpuric lesions over the flexor and medial aspect of right upper extremity. (c) Classical lesions of pityriasis rosea (PR) on lateral aspect of right thigh. (d) Classical lesions of PR on medial aspect of right thigh |
Skin biopsy of a purpuric lesion on the arm showed an acanthotic epidermis with mild hyperkeratosis, slight spongiosis and parakeratosis. The upper dermis had a sparse perivascular infiltrate of lymphocytes with several eosinophils and extravasated erythrocytes. There was no evidence of leukocytoclastic vasculitis [Figure - 2]a and b. Other investigations including complete blood counts, blood sugar, Venereal Disease Research Laboratory (VDRL) test, HIV serology, antistreptolysin O titer, coagulation profile, and urine analysis did not reveal any abnormality.
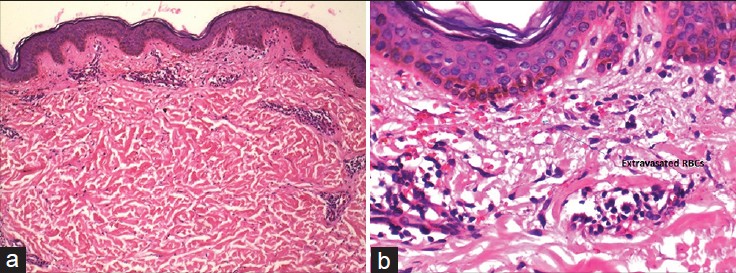 |
| Figure 2: (a) Histopathology of the purpuric lesion showing a mildly thickened orthokeratotic stratum corneum with mild spongiosis and sparse perivascular infiltrate in upper and mid dermis. H and E stain, ×100. (b) H and E stain, ×400. Acanthotic epidermis with sparse perivascular infiltrate in upper dermis and numerous extravasated erythrocytes with no evidence of leucocytoclastic vasculitis. H and E stain, ×100 |
The patient denied the use of non-prescriptional topical applications including home remedies and over-the-counter products. He was asked to stop erythromycin while emollients and antihistamines were continued. The purpuric lesions disappeared completely within 1 week of stopping erythromycin [Figure - 3]a and b although the original lesions persisted and resolved only over the next 2 weeks. To rule out the possibilty of drug hypersensitivity due to erythromycin, 4 weeks after complete clinical resolution, we administered a challenge dose of 500 mg of erythromycin to the patient under clinical supervision and followed him up for one week thereafter. No recurrence of purpuric lesions was noted thus ruling out erythromycin-induced purpura and confirming the diagnosis of purpuric variant of pityriasis rosea.
 |
| Figure 3: (a) Purpuric lesions of pityriasis rosea on right upper extremity. (b) Complete resolution of purpuric lesions of PR |
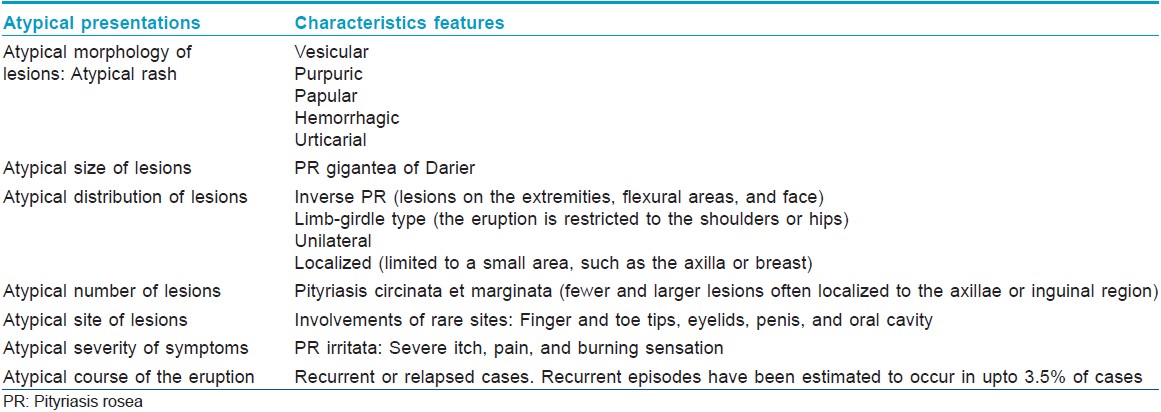
Pityriasis rosea has been etiologically associated with viral infections, especially human herpes virus-6 and -7, recent upper respiratory tract infections and several drugs, including barbiturates, clonidine, captopril, omeprazole, imatinib, isotretinoin, D-penicillamine, terbinafine, arsenicals, bismuth, and gold compounds. "Atypical pityriasis rosea" refers to cases presenting with atypical morphology or distribution of lesions and may be seen in approximately 20% of patients. [2] Various atypical types have been reported [Table - 1]. [3] Purpuric pityriasis rosea is a rare variant, first described by Hartman in 1944. [4] It is characterized by round to oval purpuric macules or papules over the trunk and limbs. Extravasation of erythrocytes without any evidence of capillaritis or vasculitis is a characteristic histopathological finding. The course and prognosis of purpuric pityriasis rosea have been described to be similar to classical disease and emollients and oral antihistamines are often the only treatment required. However, purpuric pityriasis rosea may not always be benign. A case of purpuric pityriasis rosea associated with myeloid leukemia has been reported. [5] Therefore, careful clinical examination, appropriate investigations and good follow-up is a must in all cases of atypical pityriasis rosea, especially the purpuric variant.
| 1. |
Sonthalia S, Singal A, Pandhi D, Singh UR. Annular purpuric eruption in an adult male. Indian J Dermatol Venereol Leprol 2011;77:731.
[Google Scholar]
|
| 2. |
Zawar V. Pityriasis amiantacea-like eruptions in scalp: A novel manifestation of pityriasis rosea in a child. Int J Trichology 2010;2:113-5.
[Google Scholar]
|
| 3. |
Chuh A, Zawar V, Lee A. Atypical presentations of pityriasis rosea: Case presentations. J Eur Acad Dermatol Venereol 2005;19:120-6.
[Google Scholar]
|
| 4. |
Aliaðaoðlu C, Çayýr K, Atasoy M. Purpuric pityriasis rosea. Eur J Gen Med 2005;2:83-5.
[Google Scholar]
|
| 5. |
Singal A, Pandhi D, Rusia U. Purpuric pityriasis rosea-like eruption: A cutaneous marker of acute myeloid leukaemia. J Eur Acad Dermatol Venereol 2007;21:822-3.
[Google Scholar]
|
| 6. |
Pandhi D, Singal A, Verma P, Sharma R. The efficacy of azithromycin in pityriasis rosea: A randomized, double-blind, placebo-controlled trial. Indian J Dermatol Venereol Leprol 2014;80:36-40.
[Google Scholar]
|
Fulltext Views
4,761
PDF downloads
2,544





