Translate this page into:
Lucio phenomenon: A case report
Corresponding author: Dr. Rita Vora, Department of Dermatology, Pramukhswami Medical College, Karamsad, Anand, Gujarat, India. ritavv@charutarhealth.org
-
Received: ,
Accepted: ,
How to cite this article: Bodar P, Patel J, Pillai D, Vora R. Lucio phenomenon: A case report. Indian J Dermatol Venereol Leprol. 2025;91:91-3. doi: 10.25259/IJDVL_357_2023
Dear Editor,
Lucio phenomenon is a rare reactional state seen peculiarly in the pure and primitive untreated diffuse form of lepromatous leprosy. It is a life-threatening medical emergency commonly found in Mexico and Costa Rica but relatively rare in the rest of the world. This has also been reported in South Asian countries, and there are only a few case reports from India.1 It is characterised by vascular thrombosis and invasion of blood vessel walls by leprosy bacilli, causing extensive skin ulcers.
A 35-year-old man presented to the dermatology outpatient with multiple haemorrhagic bullae of size ranging from 1 × 2 cm to 5 × 6 cm involving both the upper and lower limbs for 2-3 days. He complained of swelling and blackening of both fingertips and toes, slippage of the chappals, and decreased and tingling sensations on both extremities for one week. There was history of two episodes of erythema on the face, falling of objects from hands six-months back and one episode of epistaxis in the past three months. There was no history of leprosy among the family members or in the neighbourhood. Cutaneous examination revealed multiple, widespread, necrotising, haemorrhagic bullae and purpuric lesions on the ears, buttocks, and all limbs. Patient had diffuse facial infiltration with tense and shiny skin [Figures 1a and 1b]. and bilateral superciliary madarosis. Ear infiltration was present, with a few nodular lesions on the pinna. A single stellate necrotic plaque of size 1 × 2 cm was present on the left knee. A few hypopigmented patches of approximately 1 × 2 cm to 3 × 4 cm were present on the trunk. Pitting oedema with shiny, xerotic skin was seen on both lower limbs. Sensory examination showed symmetrical hypoesthesia on both distal extremities. Nerve examination revealed thickened and non-tender ulnar and superficial radial cutaneous nerves. Motor examination revealed weakness of the palmar interossei of both the hands. Arterial pulses were normally palpable in all the four limbs. Routine haematological and biochemical investigations were within normal limits. D-dimer was elevated at 1805 ng/ml (D-Dimer normal range 220 to 500 ng/ml). Fibrinogen was 549.7 mg/dl (Fibrinogen Normal range 200 to 400 mg/dl). Anti-phospholipid antibody IgG and IgM were negative. Slit skin smear from earlobes, eyebrows and hypopigmented lesions revealed plenty of uniformly stained acid-fast bacilli arranged singly and in globi [Figure 2a]. Fite-Faraco stain showed plenty of intracellular and extracellular lepra bacilli lying singly and in cigar bundles [Figure 2b]. Histopathological examination showed epidermal thinning with artefactual separation at dermo-epidermal junction. Dermis showed moderate to intense pan-dermal nodular perivascular infiltrate along with thrombosed vessels with predominantly lymphocytic infiltrate, necrotic debris and extravasation of RBCs with endothelial proliferation [Figure 3a]. Focal destruction of the vessel wall was also seen [Figure 3b]. Based on the clinical and histopathological findings, a diagnosis of Lucio phenomenon was made. He was treated with multibacillary antileprosy therapy, injectable corticosteroids in tapering doses, injection heparin 5000 IU subcutaneously twice a day for five days for severe haemorrhagic blisters as advised by the vascular surgeon, and antibiotics. He is on regular follow-up, with gradual improvement of the lesions.

- Diffuse infiltrated face with tense, shiny skin.

- Multiple, widespread, necrotising, purpuric lesions and haemorrhagic bullae on both lower limbs.
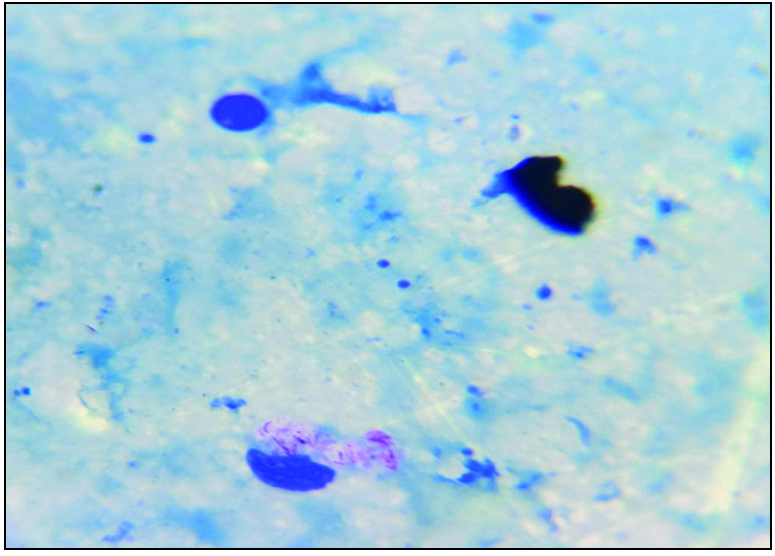
- Slit skin smear shows plenty of uniformly stained acid-fast bacilli arranged singly and in globi. (Haematoxylin & eosin, 1000x).
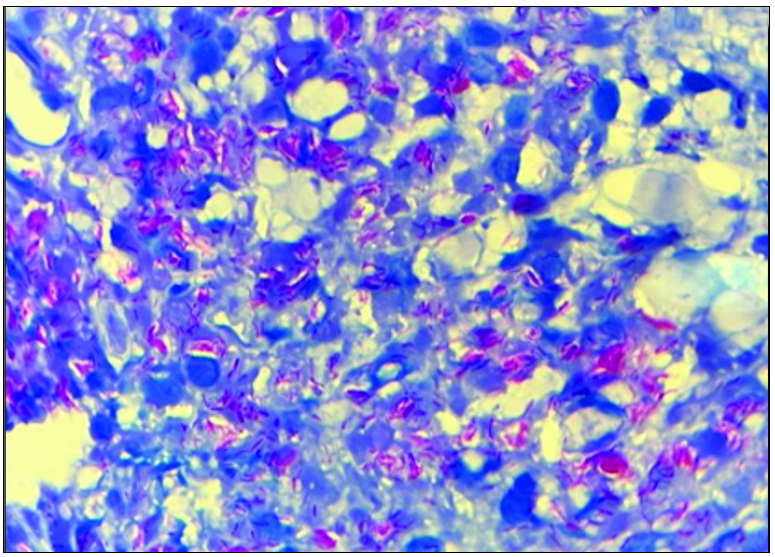
- Fite-Faraco stain shows plenty of intracellular and extracellular leprae bacilli lying singly and in cigar bundles. (Haematoxylin & eosin, 1000x).
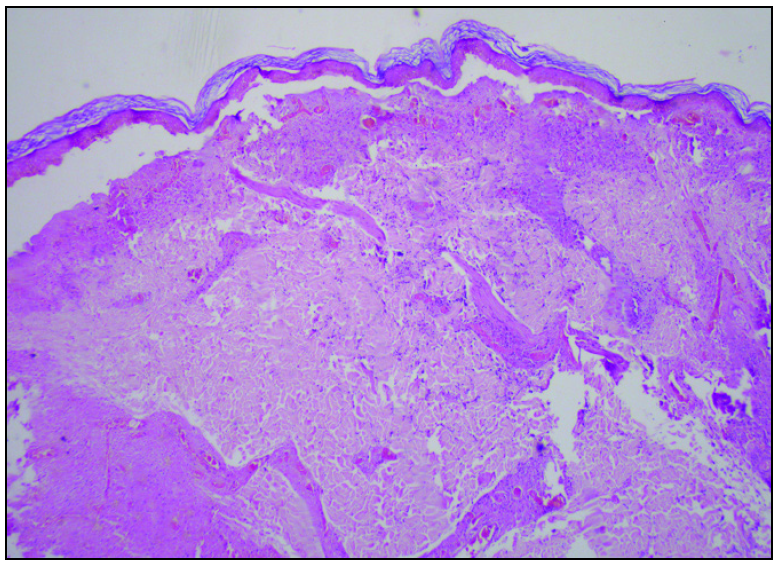
- Histopathology shows epidermal thinning with artefactual separation at the dermo-epidermal junction. Dermis shows moderate to intense pan-dermal nodular perivascular infiltrate. (Haematoxylin & eosin, 40x).
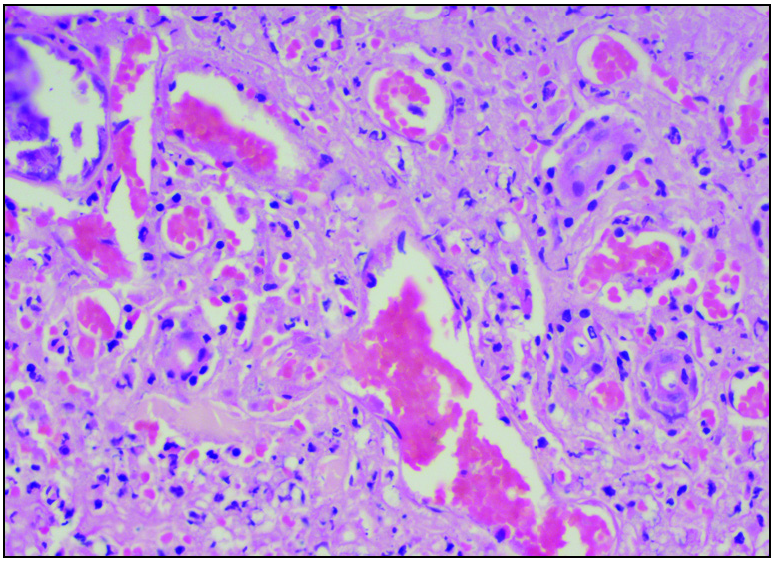
- The section shows thrombosed vessels with predominantly lymphocytic infiltrate, necrotic debris and extravasation of RBCs with endothelial proliferation and focal destruction of the vessel wall. (Haematoxylin & eosin, 400×).
Lucio phenomenon is a rare, aggressive, ulcerative and occasionally fatal type II lepra reaction. A few cases present with classical erythema nodosum leprosum after starting treatment. Type II lepra reaction (erythema nodosum leprosum) classically presents as multiple crops of evanescent, erythematous, tender nodules and plaques all over the body which can be differentiated from the Lucio phenomenon. It was first described in 1852 by Lucio and Alvarado as a necrotising skin reaction affecting patients with non-nodular lepromatous leprosy in Mexico and Central America.2 Lucio leprosy is reported to be caused by Mycobacterium lepromatosis, which was isolated from patients in Mexico.3 It is also known as “Lepra Bonita” and “Lepra Manchada”. It develops due to exacerbated proliferation of leprosy bacilli invading the walls of blood vessels and endothelial cells. This causes endothelial proliferation and reduction of the vascular lumen. The inflammatory reaction and changes in the coagulation system lead to vascular thrombosis, ischaemia, infarction and necrosis of tissues, giving rise to the histopathological features of the phenomenon.4 Lucio phenomenon meets three criteria: skin ulceration, vascular thrombosis and invasion of blood vessels by Hansen bacilli.5 Clinically, it presents as multiple, well-defined, wine–red coloured irregular macules, purpuric lesions that evolve into massive ulcerations on the extremities and heal with atrophic scarring. Differential diagnoses include antiphospholipid syndrome and disseminated intravascular coagulation. It usually begins in untreated leprosy, and anti-leprosy regimens containing rifampicin are quite effective. A short course of high-dose corticosteroids6 will help control immune reaction to M. leprae antigens. Thalidomide and clofazimine are less effective compared with their efficacy in erythema nodusum leprosum.
Here, we present a case of Lucio leprosy, unmasked by the Lucio phenomenon. Leprosy is a great mimicker of many connective tissue diseases, including vasculitis. A high index of suspicion is important for early diagnosis and prompt treatment in order to improve the disease outcome. Use of multibacillary multidrug therapy, immunosuppressants and anticoagulants, care of the cutaneous ulcers and potential infection and sepsis, are the mainstay of management in Lucio leprosy.7
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
References
- An interesting case of Lucio phenomenon triggered by activation of hepatitis C infection. Indian Dermatol Online J. 2016;7:406-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diffuse multibacillary leprosy of Lucio and Latapí with Lucio‘s phenomenon, Peru. Emerg Infect Dis. 2017;23:1929.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The leprosy agents Mycobacterium lepromatosis and Mycobacterium leprae in Mexico. Int J Dermatol. 2012;51:952-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lucio Leprosy with Lucio‘s phenomenon, digital gangrene and anticardiolipin antibodies. Lepr Rev. 2014;85:194-200.
- [PubMed] [Google Scholar]
- Lucio Phenomenon: Sequelae of Neglected Leprosy. Korean J Fam Med. 2021;42:245.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Vasculonecrotic reactions in leprosy. Braz J Infect Dis Off Publ Braz Soc Infect Dis. 2007;11:378-82.
- [Google Scholar]
- Antiphospholipid antibodies in a patient of Lucio phenomenon presenting with the gangrene of digits. Indian J Dermatol, Venereol and Leprology. 2021;87:97-101.
- [Google Scholar]





