Translate this page into:
Lucio phenomenon in a patient of lepromatous leprosy from India
Corresponding author: Dr. Suman Patra, Department of Dermatology, All India Institute Medical Sciences, Saket Nagar, Bhopal - 462 020, Madhya Pradesh, India. patrohere@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kaur M, Patra S, Asati DP, Sharma T, Prasad S. Lucio phenomenon in a patient of lepromatous leprosy from India. Indian J Dermatol Venereol Leprol 2021;87:67-70.
Sir,
Lucio phenomenon is a rare type of reaction pattern found in untreated patients with diffuse non-nodular leprosy, endemic in Mexico. It has also been reported in South Asian countries and there are only a few case reports from India.1-4 We, hereby, describe the classical presentation of a case of Lucio phenomenon which showed significant improvement with antileprosy treatment only.
A 35-year-old woman presented with mildly painful, irregular dusky erythematous plaques on buttocks, thighs, legs and swelling of hands and feet for the last 3 days. It was associated with mild fever and malaise. Additionally, she gave a history of recurrent episodes of bullae on fingers healing with atrophic scars for past 2 years. There were multiple reticulate to stellate ecchymotic and necrotic plaques surrounded by dusky erythema on bilateral buttocks [Figure 1a], legs [Figure 1b], and ear helices associated with edema of distal extremities. Elaborate examination additionally revealed symmetrical hypoesthesia on bilateral distal extremities, atrophic scars on the lateral and dorsal aspect of fingers, thick bilateral ulnar and common peroneal nerves and diffuse infiltration on face [Figure 2] and bilateral earlobes. Nodules or hypoesthetic plaques were not present anywhere on the body. Motor examination and cranial nerve examination results were within normal limits. There was no evidence of neuritis. Clinical diagnosis of lepromatous leprosy with Lucio phenomenon, necrotic erythema nodosum leprosum, vasculopathy or medium vessel vasculitis were considered. Routine investigations including complete blood count, and liver function test were within normal limits except for low hemoglobin (10.5 gm/dl) and elevated erythrocyte sedimentation rate (24 mm). Slit skin smear from ear helices and forehead showed acid-fast bacilli with a bacteriological index of 3+. Investigations to look for underlying coagulopathy, connective tissue disease including antinuclear antibody, prothrombin time /international normalized ratio, activated partial thromboplastin time and lupus anticoagulant were within normal limits. Histopathology from center and margin of necrotic plaque revealed moderate to dense perivascular and interstitial inflammatory infiltrate composed of foamy histiocytes, neutrophils and epithelioid cells [Figure 3a]. Small and medium-sized vessels showed fibrin thrombi in their lumen with vessel wall infiltration by inflammatory cells and few areas of necrosis [Figure 3b]. Fite stain revealed acid-fast bacilli in the dermis and also inside vascular endothelial cells [Figure 4]. In view of classical morphology of lesions, absence of significant constitutional symptoms, and histopathological correlation, a final diagnosis of Lucio phenomenon was made. The patient was started on World Health Organization recommended multibacillary antileprosy therapy with rifampicin, clofazimine and dapsone. Rifampicin 600 mg was also given daily for 14 days. Significant improvement in the form of decreased perilesional erythema and pain was seen within 3–4 days. Lesions on legs healed completely in 1 month [Figure 5a]. The deep necrotic plaques on buttocks formed geographic ulcers [Figure 5b] which eventually healed with scarring in 2 months.

- Multiple irregular necrotic plaques on buttocks
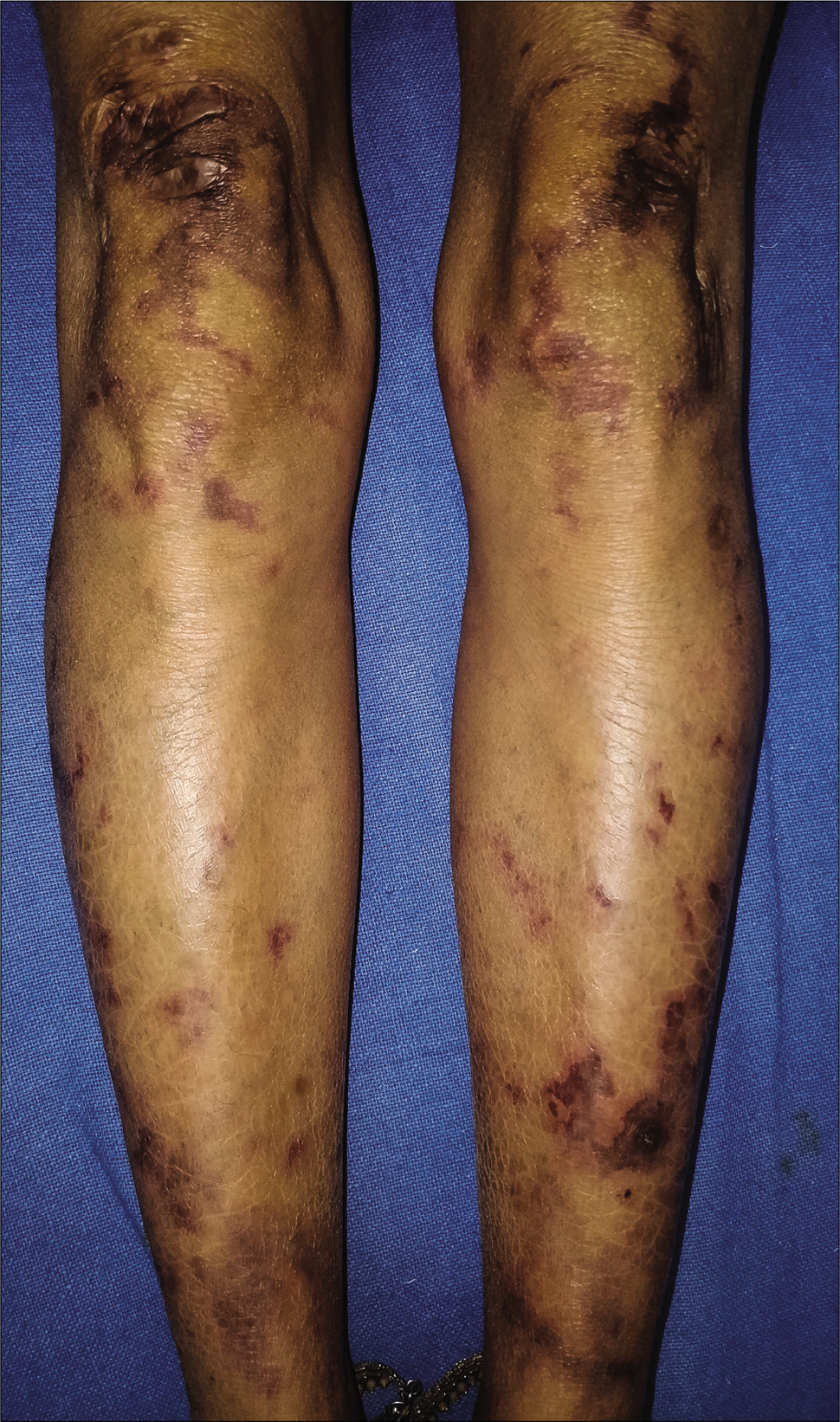
- Irregular stellate plaques on legs

- Diffuse infiltration on face
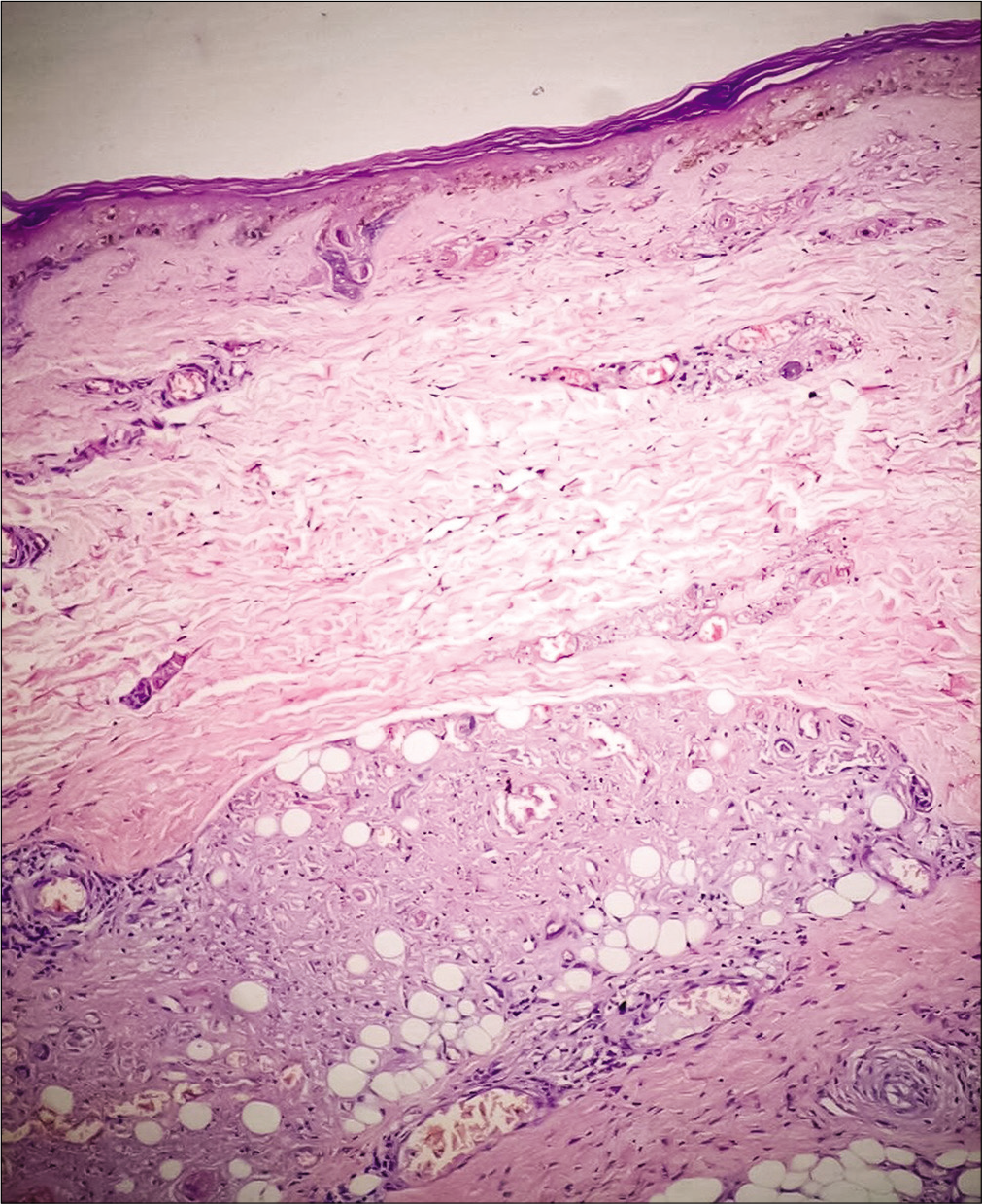
- Perivascular and periappendageal infiltrate of foamy histiocytes and few epithelioid cells (hematoxylin and eosin, 100×)
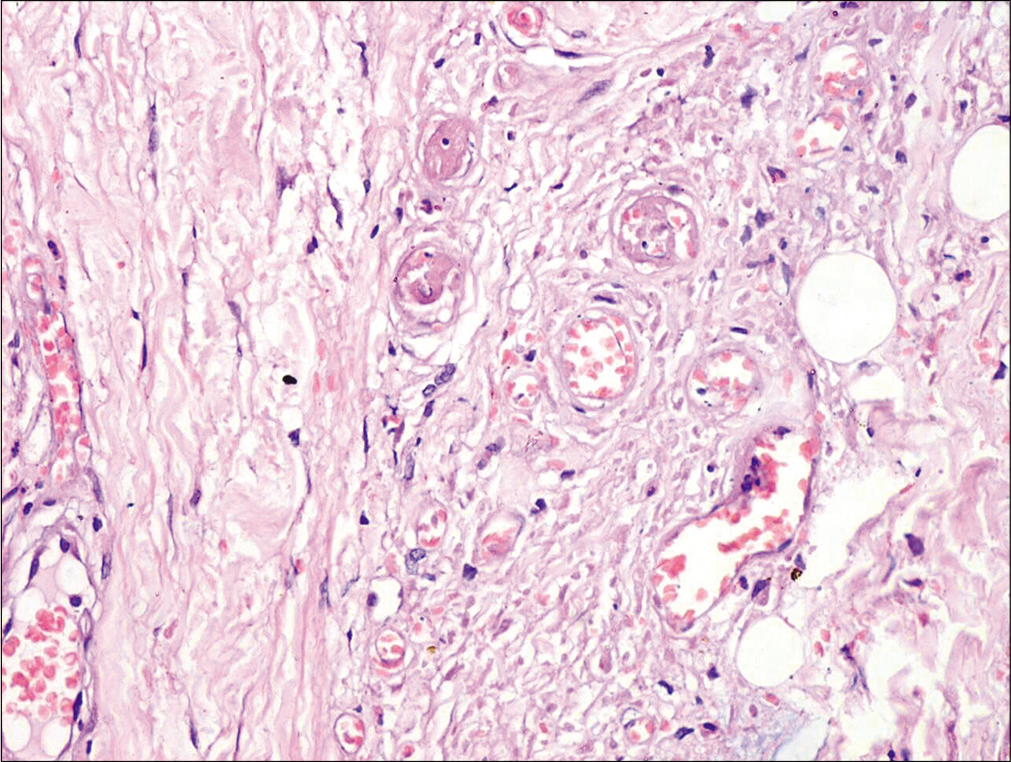
- Thrombosed and congested capillaries (hematoxylin and eosin, 200×)
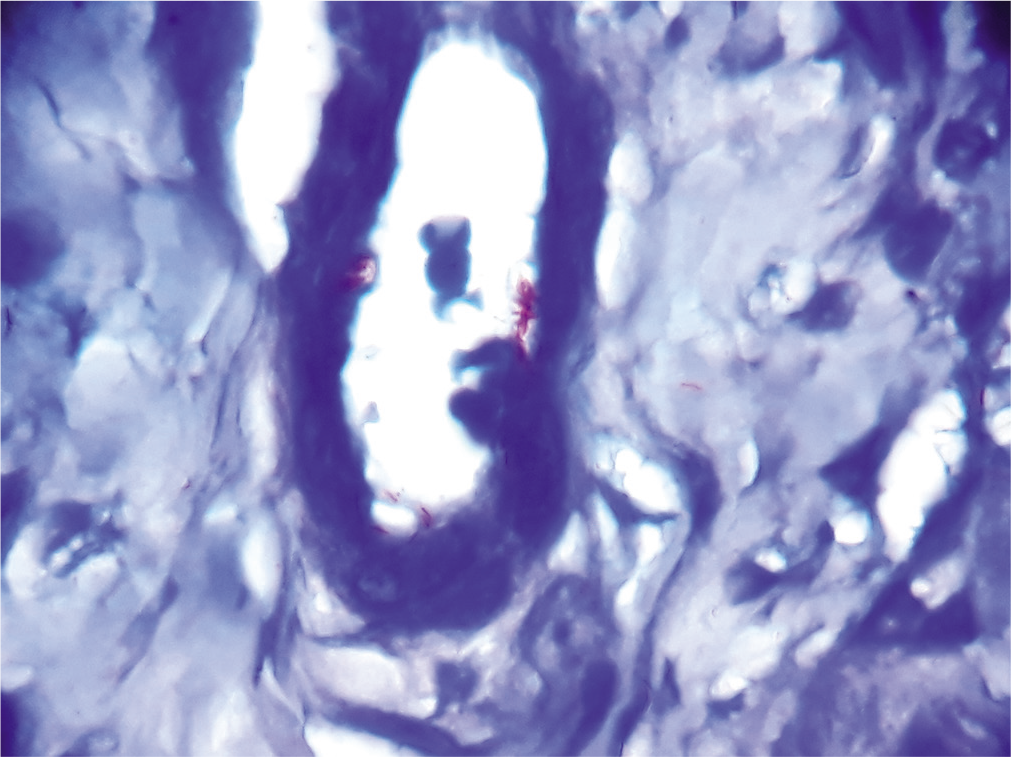
- Acid-fast bacilli inside endothelial cells (Ziehl-Neelsen stain, 1000×)
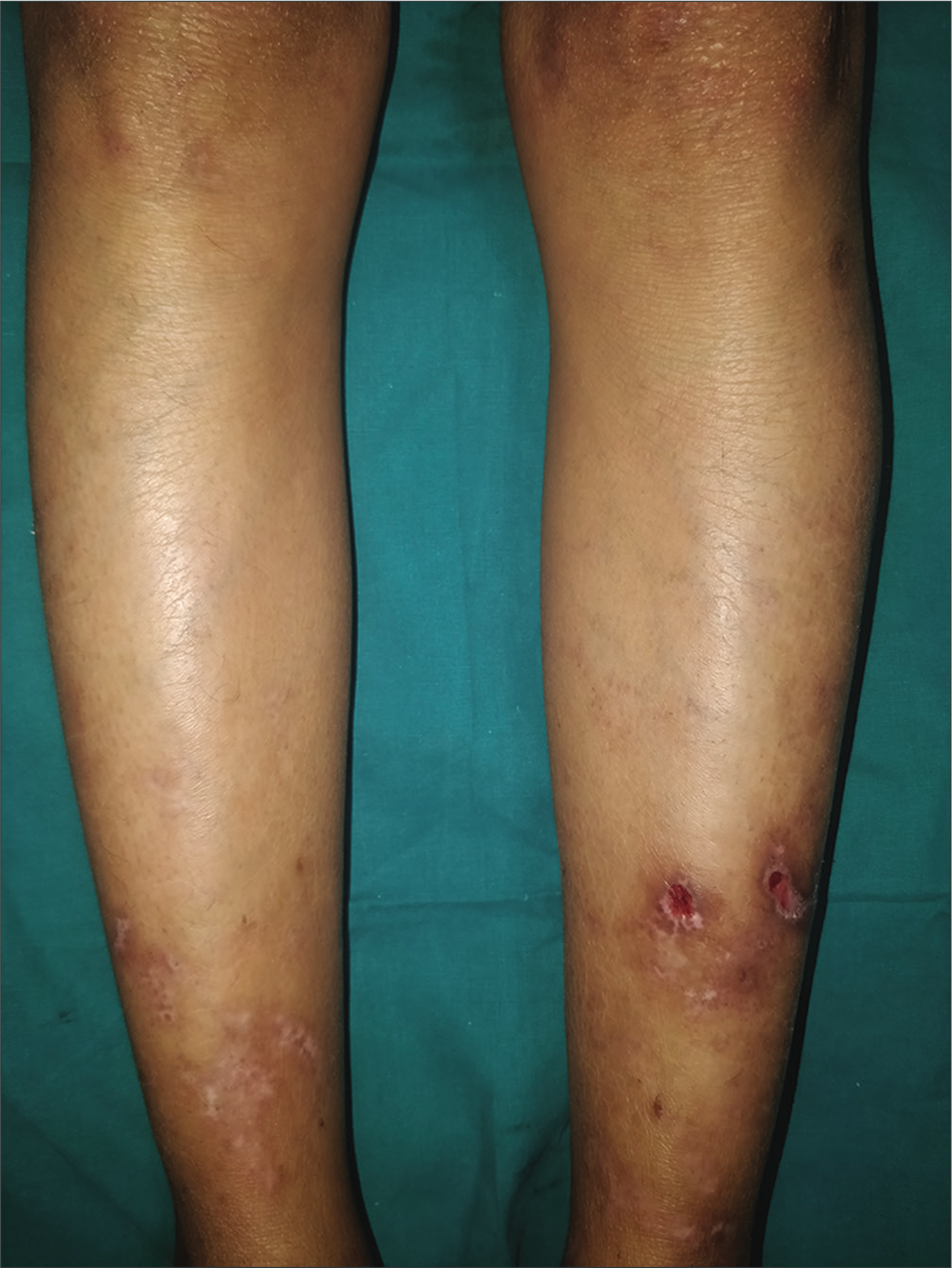
- Improvement in skin lesions on legs after 2 months

- Ulcers on buttocks after 2 months at the site of necrotic eschars
Immunologic reactions in the context of leprosy are commonly of two types, namely type I and type II lepra reaction. A rare form of lepra reaction is Lucio phenomenon which occurs due to the proliferation of lepra bacilli inside endothelial cells resulting in vascular occlusion and vasculitis. It is usually seen in untreated patients with diffuse lepromatous leprosy within 3 to 4 years of the onset of disease. They begin as erythematous painful plaques with a geographic margin on extremities which later evolve into necrotic jagged ulcers which heal in about 2–4 weeks with atrophic scars. Occasionally, hemorrhagic blisters and edema on hands, feet and ear conchae have been described. Untreated patients can have widespread cutaneous ulceration and even death has been reported.4 Typically, there are minimal or absent constitutional symptoms. Histopathology is considered diagnostic with infiltration of acid-fast bacilli singly or as globi within macrophages and endothelial cells in vessel walls; mostly of muscular/medium-sized arteries, less commonly in arterioles, venules and medium-sized veins. Smaller vessels can exhibit leukocytoclastic vasculitis. Endothelial cell proliferation, thrombosis, and ischemic necrosis are among the other features commonly seen.5 There can be considerable overlap between necrotic erythema nodosum leprosum and Lucio phenomenon both in clinical presentation and histopathology. All those features described in histopathology of Lucio phenomenon can be present in necrotic erythema nodosum leprosum.6 Even acid-fast bacilli in endothelial cells have been demonstrated in the biopsy of erythema nodosum leprosum lesions.7 However, the involvement of medium-sized vessels with thrombosis and endothelial infiltration by acid-fast bacilli is more diagnostic for Lucio phenomenon. Though there was a history of fever and malaise in our case, they were mild and much less in proportion to the severity of skin lesions. There were no painful nodules in history or examination and angular, geographic necrotic lesions were favoring vasculopathy (supported by thrombosis of vessels in the histopathology) in the setting of Lucio phenomenon rather than vasculitis, seen as a part of erythema nodosum leprosum . Positive treatment response to only antileprosy treatment further supported the diagnosis. Autoaggressive hanseniasis is another diagnosis to be considered in this setting, but those cases usually present with more systemic features and mimic one of the connective tissue disorders.8 There is no consensus regarding the treatment of Lucio phenomena due to its rarity and considerable overlap with necrotic erythema nodosum leprosum in diagnosis. Multibacillary multidrug therapy is the treatment of choice. This theory is supported by the fact that the massive replication of Mycobacterium leprae is the triggering event in Lucio phenomenon and that must be arrested to stop the reaction. In many cases, only multibacillary multidrug therapy has been used successfully,9,10 however oral and injectable corticosteroids have also been combined with antileprosy treatment in many reports.11,12 Thalidomide, once considered to be ineffective, has been used successfully in one case report.13 The lesions tend to disappear 6–8 weeks after initiation of treatment. We treated our patient with antileprosy treatment alone and she improved significantly. This report highlights the importance of being aware of the pathogenesis and clinical presentations of Lucio phenomenon as it can occur even in lepromatous leprosy in nonendemic areas. Antileprosy drugs should be considered as the first line in treatment of the condition and may alleviate the need for immunosuppressants.
Acknowledgement
Dr. Pooja Gupta, Junior Resident, Departement of Dermatology, All India Institute of Medical Sciences, Bhopal.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- An interesting case of Lucio phenomenon triggered by activation of hepatitis C infection. Indian Dermatol Online J. 2016;7:406-9.
- [CrossRef] [PubMed] [Google Scholar]
- Is it lucio phenomenon or necrotic erythema nodosum leprosum? Indian J Dermatol. 2013;58:160.
- [CrossRef] [PubMed] [Google Scholar]
- Lucio's phenomenon is a necrotizing panvasculitis: Mostly a medium-sized granulomatous arteritis. Am J Dermatopathol. 2008;30:555-60.
- [CrossRef] [PubMed] [Google Scholar]
- Lucio phenomenon or necrotic erythema nodosum leprosum: Walking the thin line. Int J Dermatol. 2020;59:e33-e35.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnostic dilemma of erythema nodosum leprosum: A clinicohistological study. Lepr Rev. 2017;88:217-26.
- [CrossRef] [Google Scholar]
- Lucio's phenomenon, Case study of an exceptional response to treatment exclusively with multibacillary multidrug therapy. An Bras Dermatol. 2013;88:93-6.
- [CrossRef] [PubMed] [Google Scholar]
- Lucio's phenomenon, an uncommon occurrence among leprosy patients in Sri Lanka. BMC Res Notes. 2015;8:672.
- [CrossRef] [PubMed] [Google Scholar]
- Lucio's phenomenon: A life-threatening medical emergency. Int J Infect Dis. 2018;69:94-5.
- [CrossRef] [PubMed] [Google Scholar]
- Lucio's phenomenon: Report of five cases. Clin Rheumatol. 2016;35:1397-401.
- [CrossRef] [PubMed] [Google Scholar]
- Lucio's leprosy: A clinical and therapeutic challenge. Clin Dermatol. 2015;33:66-78.
- [CrossRef] [PubMed] [Google Scholar]





