Translate this page into:
Lues maligna with neurosyphilis presenting in a diabetic, HIV-negative man
Corresponding author: Dr. Longfei Zhu, Department of Dermatology, The Second Affiliated Hospital, Xi’an Jiaotong University, No. 157 Xiwu Road, Xincheng District, Xi’an, Shaanxi, China. Zhulongfei008@126.com
-
Received: ,
Accepted: ,
How to cite this article: Wang Y, Yuan Y, Xiao S, Zhu L. Lues maligna with neurosyphilis presenting in a diabetic, HIV-negative man. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1362_2023
Dear Editor,
A 33-year-old unmarried man complained of multiple ulcerated nodules on his scalp for one and a half months. Before that, the patient developed mucous patches on his tongue mucosa that were persisting. [Figure 1a]. There was no itching, headache or any other accompanying symptoms and he denied drug abuse and high risk sexual behaviour. However, he had a 3-year history of untreated diabetes mellitus (fasting blood glucose 18.3 mmol/L). We observed multiple, rounded, yellow-red to dull-red, firm, non-tender nodules ranging in size from 0.5 to 3 cm in diameter distributed over his scalp, some showing crusting and erosion [Figure 1b]. Additionally, a skin-coloured papillary nodule involved his right nasolabial fold [Figure 1a]. Condyloma lata were also detected in the periumbilical and perianal areas [Figures 1c–1d].

- Split papule of the nasolabial fold and mucous patches.

- Multiple ulcerated and crusted nodules on the scalp.

- Condyloma lata on the umbilicus.

- Condyloma lata in the perianal area.
Skin biopsy from an ulcerated scalp nodule revealed epidermal verrucous hyperplasia and extensive dermal perivascular infiltration, primarily composed of plasma cells and lymphocytes [Figures 2a-2b]. Serological tests for Treponema pallidum (TP) were positive with the toluidine red unheated serum test (TRUST) and treponema pallidum particle agglutination assay (TPPA) test. The rapid plasma reagin (RPR) test was reactive at dilutions of 1:32. The test for HIV was nonreactive. The biopsy specimen subsequently showed a positive immunohistochemical staining result of TP [Figure 2c].
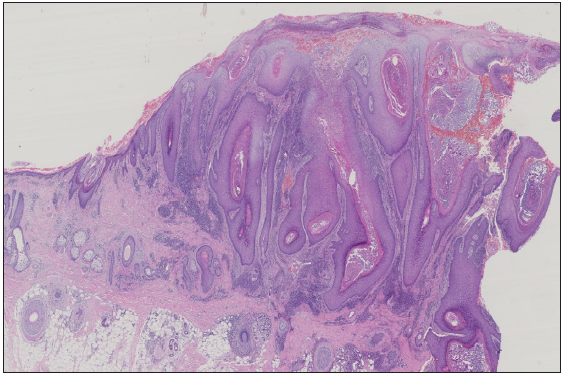
- Histopathology showing verrucous hyperplasia of the epidermis, abundant plasma cells and perivascular lymphocytic infiltrate in the dermis. (Haematoxylin and Eosin; 200x).
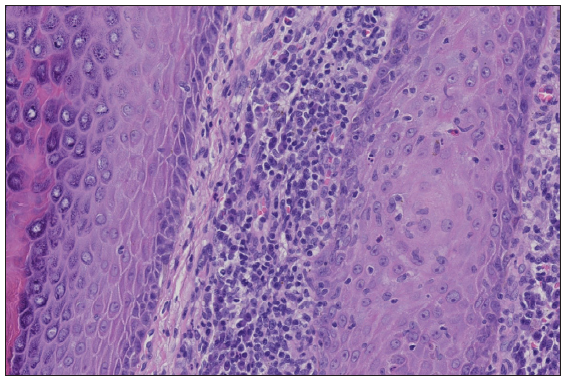
- High power view of perivascular infiltration (Haematoxylin and Eosin; 400x).
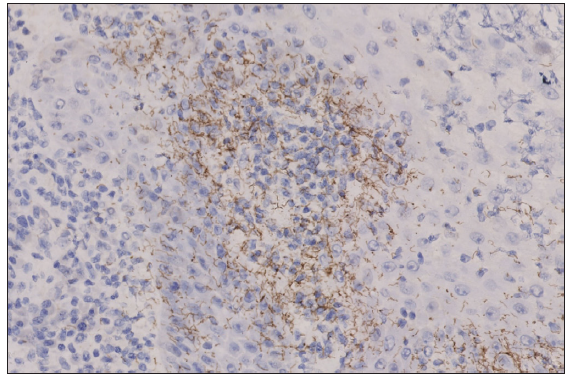
- Immunohistochemical staining result of Treponame pallidum (600x).
He improved remarkably after receiving weekly intramuscular benzathine penicillin 2.4 million IU for 3 weeks [Figure 3]. However, the patient returned to us after one month with neck mass and lymphadenectasis. A subsequent cerebrospinal fluid (CSF) examination demonstrated increased levels of protein (1.07 g/L) and glucose (6.47 mmol/L), while the TP-Ab and TPPA tests were also positive. So, we advised intravenous infusion of aqueous penicillin 18 million IU for 10 days along with incision and drainage of abscess on his mass. Two months later, the mass and lymph nodes shrank and the RPR titre reduced to 1:16.
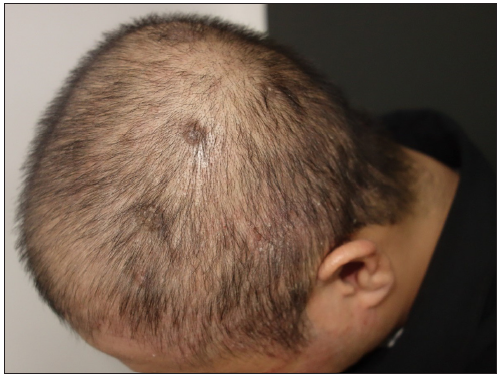
- Scalp nodules shrank and faded after treatment for 3 weeks.
Lues maligna (LM) is a rare and severe presentation of secondary syphilis, usually affecting immunocompromised people, particularly those with HIV infection.1 The occurrence of LM in HIV-negative patients with comorbidities such as diabetes mellitus, hepatitis and psoriasis raises the possibility of abnormal immune response, triggering a more severe skin manifestation and possibly more virulent strains of TP.2 The previous studies have found that the blood–brain barrier is frequently disrupted in patients with diabetes mellitus. We believe that our patient’s diabetes mellitus contributed to the severe skin manifestations and neurosyphilis. The diagnostic criteria for LM include typical clinical and histological features; a high titre serologic test for syphilis; a Jarisch–Herxheimer reaction (JHR); and a dramatic response to antibiotic therapy. However, the positive rate of JHR in LM is about 20% according to existing literature. Our patient did not present with JHR, and we diagnosed LM based on a combination of clinical, serological and histological evidence. He also had neurosyphilis and previous research has reported an increased frequency of LM neurosyphilis compared to other secondary syphilis variants.3 The most common clinical features of LM are ulceronodular cutaneous lesions with adherent crust on the central surface which primarily involve the trunk and limbs, usually sparing the head and neck.4 Mucous patches and condyloma lata are two highly infectious syphillis. Mucous patches are primarily found on the tongue, buccal mucosa and lips most prevalent subtype being ‘leukoplakia-like’.5 Condyloma lata are flat-topped, well-demarcated hypertrophic papules or plaques that often involve warm areas. In our case, mucous patches were observed on the tongue, while condyloma lata were found in the nasolabial fold, umbilicus and perianal area. Interestingly, we noticed pathological alteration of epidermal verrucous hyperplasia as revealed by a few prior studies which explained the verrucous and crater-like clinical appearance of our case. We speculate reactive epidermal hyperplasia secondary to massive inflammatory cells in the dermal papillae and intraepidermal TP. The differential diagnoses of our case include cutaneous T-cell lymphoma, eruptive keratoacanthomas and deep mycosis.
In conclusion, we report an infrequent case of LM complicated with neurosyphilis and diabetes in an HIV-negative male, presenting with multiple nodules and necrosis on the scalp. Given the recent global rise in syphilis cases, it is important for clinicians to be familiar with the unusual dermatologic manifestations of this infection.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Foundation of Shaanxi Provincial Science and Technology Department (No. 2016LCZX-03).
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Lues maligna in an immunocompetent male: A case report. J Cosmet Dermatol-US. 2022;21:3160-2.
- [CrossRef] [PubMed] [Google Scholar]
- Syphilis maligna: A presentation to bear in mind. Actas Dermosifiliogr (Engl Ed). 2019;110:232-7.
- [CrossRef] [PubMed] [Google Scholar]
- Neurosyphilis is more common in malignant syphilis: A case series and review ofthe literature. Int J STD AIDS. 2019;30:779-85.
- [CrossRef] [PubMed] [Google Scholar]
- Lues maligna. Open Forum Infect Dl. 2017;4:ofx139.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Oral manifestations of secondary syphilis. Int J Infect Dis. 2015;35:40-2.
- [CrossRef] [PubMed] [Google Scholar]





