Translate this page into:
Lupus vulgaris and borderline tuberculoid leprosy: An interesting co-occurrence
Correspondence Address:
G Raghurama Rao
Surya Skin Care and Research Center, # 15-1-2, Gopal Sadan, Naoroji Road, Maharanipeta, Visakhapatnam - 530 002, Andhra Pradesh
India
| How to cite this article: Rao G R, Sandhya S, Sridevi M, Amareswar A, Narayana BL, S. Lupus vulgaris and borderline tuberculoid leprosy: An interesting co-occurrence. Indian J Dermatol Venereol Leprol 2011;77:111 |
Sir,
The concomitant occurrence of leprosy and cutaneous tuberculosis is rare even in endemic countries. The reported incidence of pulmonary tuberculosis in patients with known leprosy has ranged from 2.5% to 7.7% in India to as high as 13.4% in South Africa. [1],[2],[3] However the prevalence of cutaneous tuberculosis is much less than that of pulmonary tuberculosis and simultaneous occurrence with leprosy is rare. [4],[5],[6],[7] We report an uncommon case of lupus vulgaris with borderline tuberculoid leprosy and their complex relationship is discussed.
A 17-year-old boy presented with two different cutaneous lesions [Figure - 1], one large plaque on the dorsum of the right foot of 1 year duration and another hypopigmented patch on the right forearm of 6 months duration. On examination, there was a large plaque of 15 x 10 cm with hypertrophic and verrucous margins on the dorsum of the right foot [Figure - 1]. There was no sensory impairment and no thickening of peripheral nerves. Right inguinal lymph nodes were palpable, discrete, and not matted. There was one hypopigmented patch of 7 x 5 cm in size with ill-defined margins [Figure - 1] on the ventral aspect of right forearm with a small satellite lesion. All sensations were impaired over the patch. Right ulnar nerve and cutaneous nerve proximal to the patch (branch of medial cutaneous nerve of forearm) were thickened and non-tender. The regional lymph nodes were not palpable. There were no similar lesions elsewhere over the body. There was no family history of either pulmonary tuberculosis or cutaneous tuberculosis or leprosy.
 |
| Figure 1: Close-up view of lupus vulgaris (dorsa of right foot) and BT leprosy (right forearm) |
Routine hematological and biochemical investigations were within normal limits. HIV screening tests and VDRL were non-reactive. The radiograph of chest was normal. Mantoux test was hyper-reactive (18 mm induration). Slit skin smears from the lesions and also ear lobes were negative for acid fast bacilli. Fine needle aspiration cytology from the right inguinal lymph node revealed granulomatous lymphadenitis compatible with tuberculous etiology. Skin biopsies were taken from both the skin lesions. Histopathology of right foot lesion showed hyperplastic epidermis with hyperkeratosis and acanthosis. Upper dermis is infiltrated with lymphocytes, epithelioid cells, and Langhans giant cells. The picture was suggestive of lupus vulgaris [Figure - 2]. A skin biopsy specimen of right forearm skin lesion showed partly thickened epidermis with patchy inflammatory cell infiltrates including lymphocytes, epithelioid cells, and a few Langhans giant cells [Figure - 3]. Fite-Farraco stain revealed no acid fast bacilli. On the basis of clinical and histopathological features two separate diagnoses were made as lupus vulgaris on the right foot and as borderline tuberculoid leprosy for forearm lesion. Lupus vulgaris was treated with DOTS-category III (Directly Observed Treatment, Short Course Strategy) with three drugs, rifampicin (450 mg), INH (600 mg) and pyrazinamide (1500 mg) daily, on alternate days three times weekly for the first 2 months, followed by two drugs, rifampicin and INH for the following 4 months. In addition, dapsone 100 mg daily for 6 months for borderline tuberculoid leprosy was also given. After 6 months of therapy, both the lesions regressed and completely healed. There were no side effects and patient′s compliance was very good. No relapse was noted during the follow up period of 3 months.
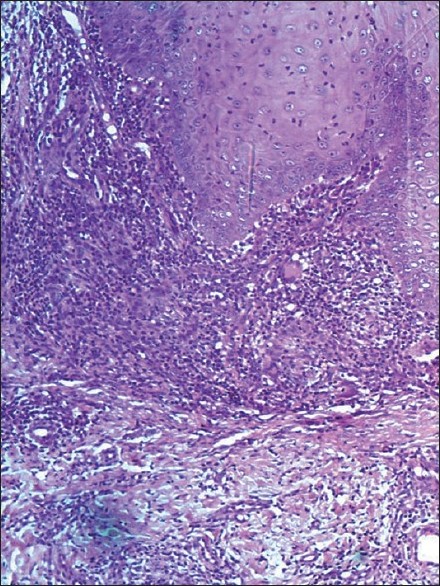 |
| Figure 2: Histopathology of right foot lesion (lupus vulgaris). Epidermis is acanthotic, upper dermis is infiltrated with lymphocytes, epithelioid cells and Langhans giant cells (H and E, ×100) |
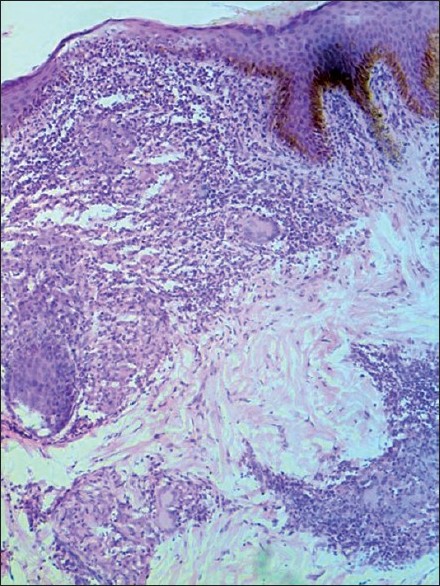 |
| Figure 3: Histopathology of the right forearm lesion (BT leprosy). Epidermis is of normal thickness. The infiltrate in the upper dermis shows an increase in number of lymphocytes, a few epithelioid cells, and Langhans giant cells (H and E, ×100) |
The exact nature of relationship between leprosy and tuberculosis still remains enigmatic. They share similarities like both diseases being caused by gram-positive, acid-fast mycobacteria that are characterized by chronic granulomatous reaction and host-specific cell-mediated immune response plays a vital role in defining the clinical spectrum. [8] In addition, they share common antigens as evidenced by conversion of tuberculin and lepromin intradermal tests after administration of BCG vaccine. [7] Our clinical report leads to an important area that needs to be investigated---Does the presence of one mycobacterial disease prevent or modify the course of other one? Some investigators believed that leprosy and tuberculosis are antagonistic diseases on the basis of immunologic, clinical, and epidemiologic data. [9],[10] Although an increased incidence of pulmonary tuberculosis has been observed in patients with leprosy, the converse is not observed in patients with tuberculosis. [3],[9] They were of the opinion that prior infection with pulmonary tuberculosis has a protective effect against infection with Mycobacterium leprae. [10] In our case, cutaneous tuberculosis lesion (lupus vulgaris) was first to appear with a specific cell-mediated immunity (Mantoux 18 mm) and the borderline tuberculoid leprosy developed 6 months later due to long incubation period of the disease. This case and the previous reports [4],[5],[6] clearly illustrate that there is no absolute antagonism between these two infections and there is no cross immunity. It is possible that M. tuberculosis and M. leprae elicit-specific cell-mediated immunity by affecting different CD4/CD8 sub populations. The host impaired inherent immunity may be responsible for the co-occurrence of dual mycobacterial diseases in our case.
| 1. |
Kumar B, Kaur S, Kataria S, Roy SN. Concomitant occurrence of leprosy and tuberculosis - a clinical, bacteriological and radiological evaluation. Lepr India 1982;54:671-6.
[Google Scholar]
|
| 2. |
Singh M, Kaur S, Kumar B, Kaur I, Sharma VK. The associated diseases with leprosy. Indian J Lepr 1987;59:315-21.
[Google Scholar]
|
| 3. |
Gatner EM, Glatthaar E, Imkamp FM, Kok SH. Association of tuberculosis and leprosy in South Africa. Lepr Rev 1980;51:5-10.
[Google Scholar]
|
| 4. |
Patki AH, Jadhav VH, Mehta JM. Leprosy and multicentric lupus vulgaris: A case report. Indian J Lepr 1990;62:368-70.
[Google Scholar]
|
| 5. |
Pinto J, Pai GS, Kamat N. Cutaneous tuberculosis and leprosy: A case report. Indian J Dermatol Venereol Leprol 1991;57:303-4.
[Google Scholar]
|
| 6. |
Inamadar AC, Sampagavi VV. Concomitant occurrence of leprosy, cutaneous tuberculosis and pulmonary tuberculosis: A case report. Lepr Rev 1994;65:282-5.
[Google Scholar]
|
| 7. |
Kumaran MS, Dogra S, Kaur I, Kumar B. Lichen scrofulosorum in a patient with lepromatous leprosy after BCG immunotherapy: A case report. Lepr Rev 2005;76:170-4.
[Google Scholar]
|
| 8. |
Lee HN, Embi CS, Vigeland KM, White CR Jr. Concomitant pulmonary tuberculosis and leprosy. J Am Acad Dermatol 2003;49:755-7.
[Google Scholar]
|
| 9. |
Fernandez JM. Leprosy and tuberculosis. Arch Dermatol 1957;75:101-6.
[Google Scholar]
|
| 10. |
Lietman T, Porco T, Blower S. Leprosy and tuberculosis: The epidemiological consequences of cross-immunity. Am J Public Health 1997;87:1923-7.
[Google Scholar]
|
Fulltext Views
5,295
PDF downloads
3,593





