Translate this page into:
Lyme disease in Haryana, India
Correspondence Address:
Vijayeeta Jairath
11-J/2 UH Medical Enclaves, Post Graduate Institute of Medical Sciences, Rohtak, Haryana - 124001
India
| How to cite this article: Jairath V, Sehrawat M, Jindal N, Jain V K, Aggarwal P. Lyme disease in Haryana, India. Indian J Dermatol Venereol Leprol 2014;80:320-323 |
Abstract
Lyme disease is a multiorgan animal-borne disease caused by the spirochete Borrelia burgdorferi. This case series highlights its presence in Haryana, a nonendemic zone. The first case was a 27-year-old housewife who presented with an annular erythematous patch with a central papule following an insect bite on the left upper arm. The second case was a 32-year-old farmer who gave a history of insect bite on the right arm followed by the development of an erythematous patch with a central blister. The third case, a 17-year-old boy presented with a history of tick bite over right thigh and a typical bull's eye lesion with central ulceration. These cases were managed with oral doxycycline 100 mg twice daily for 14 days. The fourth case was a 7-year-old boy with typical erythema migrans on the right check and neck while the fifth case, a 30-year-old housewife, presented with an erythematous patch with a central papule on the right buttock. These patients were treated with oral amoxycillin 25 mg/kg, thrice daily for 14 days. All patients showed IgM antibodies to B. burgdorferi. Treatment led to clearance of lesions in all the patients. Lyme borreliosis was diagnosed in these patients based on the history of established exposure to tick bites, presence of classic signs and symptoms, serology and the response to treatment.INTRODUCTION
Lyme disease, caused by the spirochete Borrelia burgdorferi, is a tick-borne disease, the global distribution of which corresponds to the distribution of Ixodes tick that transmits the organism. Borrelia burgdorferi is normally carried by mice, squirrels, birds, and other small animals. Ticks become infected while feeding on the infected animal and thus transmit the disease to humans. Deer have been found to be the reservoir for this disease. [1]
Lyme disease is a multisystem inflammatory disorder with a wide spectrum of skin manifestations. Skin lesions are often the first clinical manifestation of the disease; early identification of such lesions is important for prompt diagnosis and treatment which can prevent systemic complications. [2]
Most previously reported cases are from endemic regions like United States, Europe, Middle East, and southeast Asia which are the natural habitat for the vector, the Ixode sticks. [3] Recently, a rise has been seen in the incidence of disease and the ailment is now being reported from all countries which may be attributed to increased migration of people across nations. [3]
A literature search revealed only a few previously reported cases of Lyme disease from India. [4] This case series illustrates a rare clustering of five cases over a period of 3 months in a nonendemic region, Rohtak, Haryana.
Case Reports
Case 1
A 27-year-old housewife presented to our outpatient department in September 2013 with a history of insect bite over the left upper arm while farming outdoors. Six days later she developed a progressive itchy red rash at the site of the bite along with fever, headache and arthralgia. Examination revealed an erythematous, 7 cm × 8 cm, annular patch with a smooth surface and a central papule on the left upper arm. Left axillary lymphadenopathy was noted [Figure - 1].
 |
| Figure 1: Annular erythematous 7 cm × 8 cm patch with smooth surface and a papule in the center of the lesion present over left upper arm |
Case 2
About 2 weeks later, a 32-year-old farmer presented with a history of an insect bite on the right arm while working in the fields, 10 days after which he developed a fluid-filled lesion at the same site with surrounding erythema. This was associated with itching and a burning sensation along with fever, malaise, and arthralgia. On examination, a blister on an erythematous base was present over the right arm surrounded by a diffuse erythematous patch measuring 6 cm × 7 cm in size. Right axillary lymphadenopathy was present [Figure - 2].
 |
| Figure 2: Blister on an erythematous base over the right arm surrounded by a diffuse erythematous patch measuring 6 cm × 7 cm in size |
Case 3
A 17-year-old boy presented with a history of tick bite over the right thigh while playing football outdoors. A week later an ulcer developed at the same site followed by rapidly increasing redness around the ulcer associated with symptoms of myalgia, fatigue, and fever with chills. Examination revealed a typical bull′s eye lesion with a central necrotic ulcer with a ring of erythema of 10 cm diameter [Figure - 3].
 |
| Figure 3: Bull's eye lesion with a central necrotic ulcer with a 10 cm ×10 cm diameter ring of erythema |
Case 4
A 7-year-old boy presented with a 4-day history of an asymptomatic reddish discoloration over the right cheek and neck. He was not aware of an insect bite prior to the erythema but had visited a local resort with his family 2 weeks back. He also had fever, fatigue, and myalgia. On examination, a homogenous erythematous patch measuring 15 cm × 10 cm was present around the right ear extending onto the right side of neck. Cervical and posterior auricular lymphadenopathy was noted [Figure - 4].
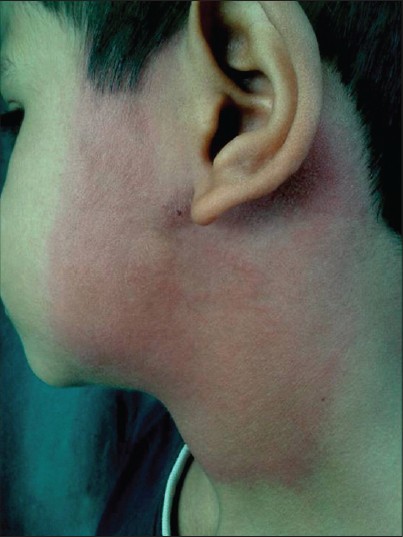 |
| Figure 4: Homogenous erythematous patch measuring 15 cm × 10 cm was present over right pre- and postauricular region and over right side of neck |
Case 5
A 30-year-old housewife presented to our outpatient department in mid-November, 2013 with a 2-day history of skin rash. She gave a history of tick bite in the fields around 10 days back. The tick had been detached manually almost immediately. On examination, a typical erythema migrans (EM)-like lesion measuring 10 × 8 cm with a central crusted papule was noted [Figure - 5].
 |
| Figure 5: Typical erythema migrans (EM) lesion over left gluteal region, 10 cm × 14 cm in size. Note the crusted papule in the center representing the tick bite |
All these cases were clustered over a period of 3 months. All the five patients were subjected to baseline investigations which included a complete hemogram with peripheral blood smear which were normal in all cases. Serological tests were done following the two-test approach, involving initial screening with enzyme-linked immunosorbent assay (ELISA) and confirmation by Western blot using commercial ELISA and Western blot kits (Novatech, Germany). IgM antibodies to the purified antigens of B.burgdorferi were detected in all the patients and IgG antibodies in two of them thus confirming the diagnosis (positive p41 band and OspC band). All the cases had a negative Treponema pallidum hemagglutination test.
Biopsy from the active margin of the lesions in all patients revealed a normal epidermis and a perivascular inflammatory infiltrate of lymphocytes and plasma cells in the dermis. However, Warthin-Starry stain could demonstrate the spirochete in only three patients. Culture could not be done due to unavailability of the bacteriologic agar in our institution.
Treatment was initiated in all cases without awaiting test results. The first three cases were managed with doxycycline, 100mg twice daily for 14 days. Treatment was continued for a further 7 days in the third patient. The remaining two patients were started on amoxicillin, 25 mg/kg thrice daily for 14 days. Treatment led to clearance of erythema migrans. No secondary manifestations or systemic complaints were noted on the follow-up visits.
DISCUSSION
Lyme disease is generally caused by three species of Borrelia: B. burgdorferi, B. burgdorferi sensustricto, B. afzelii, and B. garinii; the latter two being more frequently reported from Asia. [4]
Clinically, Lyme borreliosis is divided into three stages: early localized disease, early disseminated disease, and chronic disease. Erythema migrans is a prominent clinical feature of early disease seen in 60-70% of cases appearing as an erythematous, growing annular plaque. Resembling a bull′s eye and is referred to as the target lesion. The surface is usually smooth, though sometimes a crusted or advancing edge may be observed. It appears after 7-15 days of tick detachment. [5]
As per the Centers for Disease Control and Prevention (CDC) guidelines for a lesion to qualify as erythema migrans, it should be at least 5 cm in diameter; however, smaller lesions may be considered in appropriate clinical circumstances. All our cases were of diameter greater than 5 cm with the typical target appearance of the lesion.
Erythema migrans must be distinguished from a number of conditions such as exaggerated local arthropod reactions, erysipelas, non-pigmented fixed drug eruption, cellulitis, and allergic contact dermatitis. [6] The diagnostic test method for direct detection of B.burgdorferi is polymerase chain reaction (PCR)-based molecular technique done on skin biopsy samples. Spirochetal deoxyribonucleic acid (DNA) is detected using two primer sets targeting 23S rRNA (PCR I) and 66-kDa protein (PCR II) genes. It is more sensitive and specific in early erythema chronicum migrans (ECM) but has been reserved for atypical presentations. [7] Various treatment modalities for erythema migrans are available. Doxycycline (100 mg orally twice daily for 14-21 days) is the drug of choice, others being amoxicillin, azithromycin, and cefuroxime axetil. [2]
The clinical presentation, positive serologic tests and improvement with antibiotics and steroids confirmed our diagnosis of Lyme disease.
Ixodes ticks are present in Himalayan region of India, and thus, there is a likelihood that Lyme disease may exist in our country. Patial et al., have reported a 15-year-old boy with Lyme disease in Shimla diagnosed by demonstrating Borrelia in the blood smear. [8] A study carried out in north India by Handa et al., reported one positive case of Lyme borreliosis. [9] A study of 500 people from the northeastern states of India was done by Praharaj et al. to assess the seroprevalence of Borrelial antibodies; 13% of the population was seropositive to IgG antibody detected by a commercial ELISA kit (NovaTech, Germany). [10]
Recently, an outbreak of Lyme borreliosis in Wayanad district, Kerala, South India was reported in the lay press. Health officials believed that the vector was deer ticks. [11] No specific species of ticks causing Lyme borreliosis in India have been recognized; however, Ixodes ticks are present in the Himalayan region of India and an isolated case report of Lyme disease from south India identified the Haemophysalis species of ticks. [4]
The possible reason for emergence of Lyme borreliasis in Haryana, a state in northern India, could be the exposure of individuals to ticks in the fields as the population is predominantly rural. Another reason could be the favorable temperature for the mite, as they quest most actively from spring to autumn in microenvironments with more than 85% relative humidity. [2] However, there is no good explanation for the recent sudden rise in the incidence of Lyme disease in an area where no previous cases were reported and these findings require further exploration.
| 1. |
Grubhoffer L, Golovchenko M, Vancová M, Zacharovová-Slavícková K, Rudenko N, et al. Lyme borreliosis: Insights into tick-/host-borrelia relations. Folia Parasitol (Praha) 2005;52:279-94.
[Google Scholar]
|
| 2. |
Izzoli A, Hauffe H, Carpi G, Vourc HG, Neteler M, Rosà R. Lyme borreliosis in Europe. Euro Surveill 2011;16:19906.
[Google Scholar]
|
| 3. |
Murray TS, Shapiro ED. Lyme disease. Clin Lab Med 2010;30:311-28.
[Google Scholar]
|
| 4. |
Vasudevan B, Chatterjee M. Lyme borreliosis and skin. Indian J Dermatol 2013;58:167-74.
[Google Scholar]
|
| 5. |
España A. Figurate Erythema. In: Jorizzo JL, Rapini RP, editors. Bolognia textbook of Dermatology. Dermatology. 2 nd ed. British Library Cataloguing in Publication Data; 2008. Vol 1, p. 1717-20.
[Google Scholar]
|
| 6. |
Biesiada G, Czepiel J, Lesniak MR, Garlicki A, Mach T. Lyme disease: Review. Arch Med Sci 2012;8:978-82.
[Google Scholar]
|
| 7. |
Brettschneider S, Bruckbauer H, Klugbauer N, Hofmann H. Diagnostic value of PCR for detection of Borreliaburgdorferi in skin biopsy and urine samples from patients with skin borreliosis. J ClinMicrobiol 1998;36:2658-65.
[Google Scholar]
|
| 8. |
Patial RK, Kashyap S, Bansal SK, Sood A. Lyme disease in a Shimla boy. J Assoc Physicians India 1990;38:503-4.
[Google Scholar]
|
| 9. |
Handa R, Wali JP, Singh S, Aggarwal P. A prospective study of Lyme arthritis in north India. Indian J Med Res 1999;110:107-9.
[Google Scholar]
|
| 10. |
Praharaj AK, Jetley S, Kalghatgi AT. Seroprevalence of Borrelia burgdorferi in North Eastern India. MJAFI 2008;64:26-8.
[Google Scholar]
|
| 11. |
KR Rajeev. Lyme disease outbreak in WayanadTNN,The Times of India [newspaper on theInternet].March2,2013Availablefrom:( http: // timesofindia.indiatimes.com/city/kozhikode/Lyme-disease-outbreak-in-Wayanad/articleshow/18758675.cms?referral=PM).
[Google Scholar]
|
Fulltext Views
17,080
PDF downloads
2,612





