Translate this page into:
Lymphangioma circumscriptum-like presentation of breast carcinoma
2 Department of Pathology, Kocaeli University Medical Faculty, Kocaeli, Turkey
3 Department of General Surgery, Kocaeli University Medical Faculty, Kocaeli, Turkey
Correspondence Address:
Evren Odyakmaz Demirsoy
Department of Dermatology, Kocaeli University Medical Faculty, Kocaeli
Turkey
| How to cite this article: Bayramg�rler D, Demirsoy EO, Doğan N, Yıldız K, Utkan Z. Lymphangioma circumscriptum-like presentation of breast carcinoma. Indian J Dermatol Venereol Leprol 2012;78:121 |
Sir,
The most common cause of cutaneous metastases (CM) in women is breast carcinoma. CM of breast carcinoma usually manifests as nodules, while carcinoma erysipeloides, carcinoma en cuirasse, telangiectatic carcinoma, alopecia neoplastica, malignant melanoma-like metastases and subungual metastases are other commonly reported types. Besides these well-known presentations, CM can mimic many benign skin lesions. [1] CM are usually seen in patients with advanced diseases, but can rarely be the presenting lesion. [2] In the latter cases or in cases of uncommon presentations, diagnoses of CM may be difficult. We present a case with lymphangioma circumscriptum-like telangiectatic carcinoma, which is a rare form of CM.
A 39-year-old woman presented to us with a 6-month history of enlarging erythema and blisters on her left axilla. Dermatological examination revealed multiple slightly erythematous flesh-colored papules having vesicular image on her left axilla [Figure - 1]a. Skin biopsy from papules was consistent with adenocarcinoma metastases with involvement of the dermal lymphatic and capillaries by tumor cells [Figure - 1]b and c. Physical examination was unremarkable except ipsilateral axillar lymphadenopathy, which had also been realized by the patient for the last 6 months. She consulted the General Surgery Department, where a mass in her left breast was noticed and fine-needle aspiration biopsy from her breast mass and lymph node excision were performed by a surgeon. She was diagnosed as breast carcinoma (stage IV) after her histopathologic and radiologic investigations. She was treated with chemotherapy (docetaxele and anthracycline) and radiation therapy. All skin lesions disappeared during treatment. One month after the radiation therapy had been stopped, she presented with vesicular lesions on her left shoulder. An infiltrated erythematous, warm, tender plaque with well-defined margins affecting her mastectomy area and spreading to her left shoulder was detected. There were also coalescent hemorrhagic vesicules on the shoulder area without typical zosteriform distribution [Figure - 2]. Biopsy specimens from both plaque and vesicular lesions supported carcinoma metastases and the patient was referred to the Medical Oncology Department. Abdominal computed tomography scan showed metastatic nodular lesions in the liver. She died while she was treated with chemotherapy.
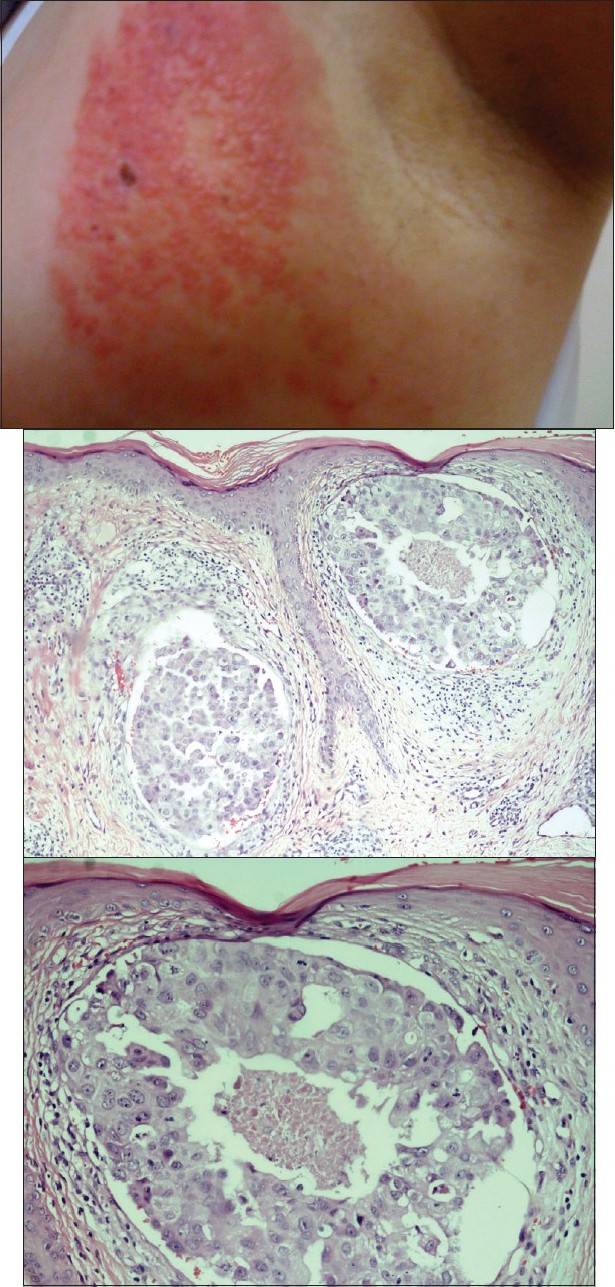 |
| Figure 1: (a)Erythematous flesh-colored papules having vesicular image on left axilla Figure 1b: Tumor thrombosis into lymph vessels in papillary dermis and necrosis in the thrombus (H and E, ×100) Figure 1c: Tumor cells typical for breast carcinoma with pale basophilic cytoplasm, enlarged pleomorphic nuclei and prominent nucleoli (H and E, ×200) |
 |
| Figure 2: Hemorrhagic vesicles on the left shoulder |
Telangiectatic carcinoma is a rarely seen manifestation of CM from breast carcinoma, characterized by purpuric nodules/papules/plaques, [1] or erythematous patch with prominent telangiectasias, or lymphangioma circumscriptum-like pseudovesicles. [3],[4] Traditionally, CM have often been regarded as a sign of advanced and disseminated disease. Recently, Hu et al. showed that there are differences in survival for CM arising from different internal malignancies, with breast cancer patients having a relatively better prognosis compared with other cancers. They suggested that discovery of CM in breast cancer did not necessarily indicate widely disseminated disease. [5] In our case, cutaneous lymphangioma circumscriptum-like pseudovesicles on the left axillary region were the presenting symptom leading to the diagnosis of breast cancer. The skin lesions improved after chemotherapy and radiation therapy, but recurrence of similar vesicular lesions was noted on the left shoulder 1 month after radiation therapy had been stopped. There was no evidence of visceral metastases at the time of diagnosis, but concomitant liver metastases had been found with recurrent cutaneous lesions.
Telangiectatic carcinoma should be differentiated from cutaneous lymphangioma circumscriptum, Stewart-Treves syndrome an zosteriform CM. Zosteriform CM present as nodular, papulovesicular or vesiculobullous lesions, but these lesions are typically distributed along one or more dermatomes. [1] In our case, the lesions never showed a zosteriform distribution.
Histopathologically, it has been mostly proposed that malignant cells are present predominantly in dermal capillaries, although spread of tumor cells via lymphatics is also reported. [4] In our case, both dermal capillaries and lymphatic vessels were invaded by tumor cells.
| 1. |
De Giorgi V, Grazzini M, Alfaioli B, Savarese I, Corciova SA, Guerriero G, et al. Cutaneous manifestations of breast carcinoma. Dermatol Ther 2010;23:581-9.
[Google Scholar]
|
| 2. |
Vano-Galvan S, Moreno-Martin P, Salguero I, Jaen P. Cutaneous metastases of breast carcinoma: A case report. Cases J 2009;2:71.
[Google Scholar]
|
| 3. |
Lin JH, Lee JY, Chao SC, Tsao CJ. Telangiectatic metastatic breast carcinoma preceded by en cuirasse metastatic breast carcinoma. Br J Dermatol 2004;151:523-4.
[Google Scholar]
|
| 4. |
Marneros AG, Blanco F, Husain S, Silvers DN, Grossman ME. Classification of cutaneous intravascular breast cancer metastases based on immunolabeling for blood and lymph vessels. J Am Acad Dermatol 2009;60:633-8.
[Google Scholar]
|
| 5. |
Hu SC, Chen GS, Lu YW, Wu CS, Lan CC. Cutaneous metastases from different internal malignancies: A clinical and prognostic appraisal. J Eur Acad Dermatol Venereol 2008;22:735-40.
[Google Scholar]
|
Fulltext Views
2,413
PDF downloads
3,157





