Translate this page into:
Lymphangiomas: Rare presentations in oral cavity and scrotum in pediatric age group
Correspondence Address:
Meghana Madhukar Phiske
Department of Dermatology, OPD 14, 2nd Floor, OPD Building, Topiwala National Medical College and B.Y.L. Nair Ch. Hospital, Mumbai - 400 008, Maharashtra
India
| How to cite this article: Kurude AA, Phiske MM, Kolekar KK, Nayak CS. Lymphangiomas: Rare presentations in oral cavity and scrotum in pediatric age group. Indian J Dermatol Venereol Leprol 2020;86:230 |
Abstract
The incidence of lymphangioma is 1.2 to 2.8/1000 newborns. They present at birth/before 2 years, with predilection for the head and neck (50%–70%). The buccal mucosa is the second most common site reported (14 cases reported) after the anterior two-thirds of tongue. The scrotum is a rare site with less than 50 cases reported (till 2002). Involvement of vital structures, aesthetic, and functional requirements may necessitate treatments such as surgical excision, radiation, cryotherapy, electrocautery, sclerotherapy, embolization, ligation, and laser. Two rare cases – the first being primary, late-onset buccal lymphangioma, with vesicular presentation, and the second being genital lymphangioma involving the right side of scrotum, thigh, and groin with extension to the left groin – are highlighted.
Introduction
Lymphangiomas, first described by Redenbacher in 1828, are benign congenital or hamartomatous malformation of lymphatic vessels, arising from sequestration of lymphatic tissue. Their incidence ranges from 1.2 to 2.8/1000 newborns.[1] Approximately 50% are present at birth and 90% are diagnosed before the age of 2 years. They are most frequently found in the neck (75%) and axillae (15%).[2] The oral cavity is rarely involved, the most common involved site being tongue. The less commonly involved sites include palate, buccal mucosa, gingiva, floor of mouth, and lips.[3]
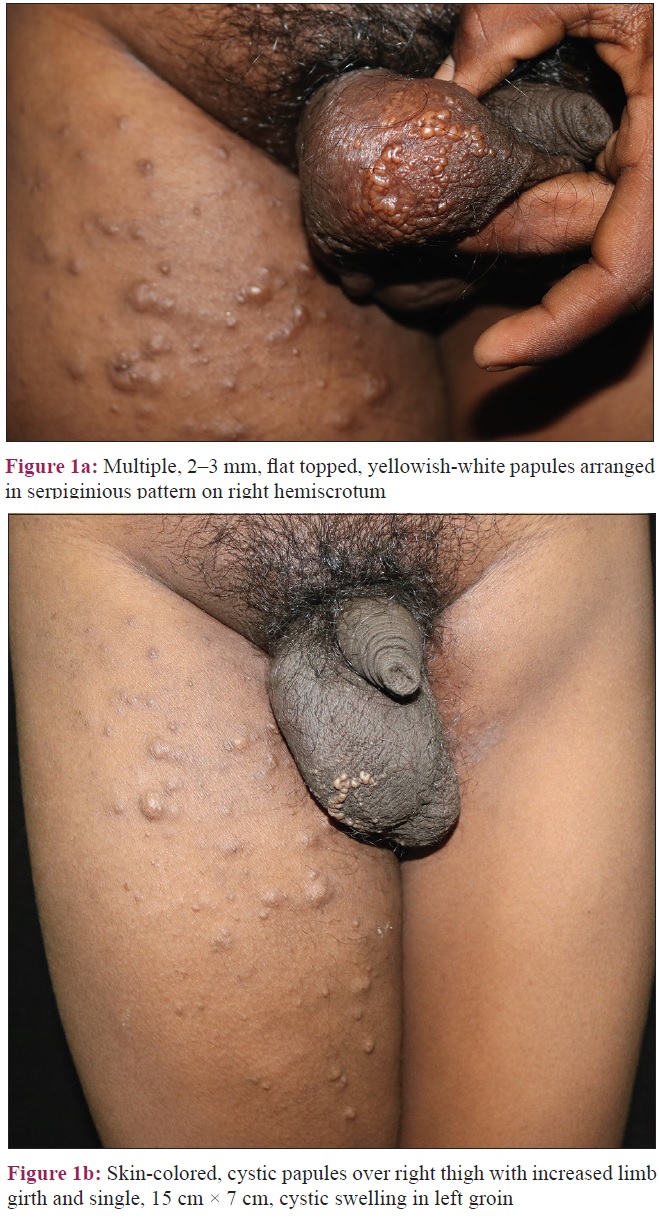
We found 24 cases of lymphangiomas of buccal mucosa reported till date [Table - 1], of which 6 were children as per available data.
We found less than 65 cases of primary genital lymphangiomas till date, of which 12 cases had scrotal and thigh/inguinal involvement [Table - 2].
Involvement of vital structures or aesthetic/functional requirements may necessitate treatment. 4 Two rare cases, one of bilateral buccal lymphangioma and the other, a lymphangioma involving scrotum, groin, and thigh with bony involvement, are reported. The cases presented to the skin OPD, TNMC, and B.Y.L. Nair Ch. Hospital, Mumbai.
Case Reports
Case 1
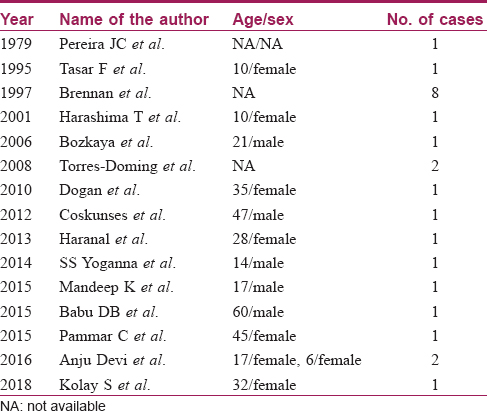
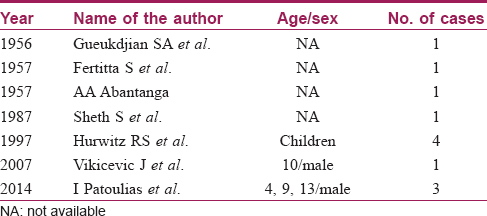
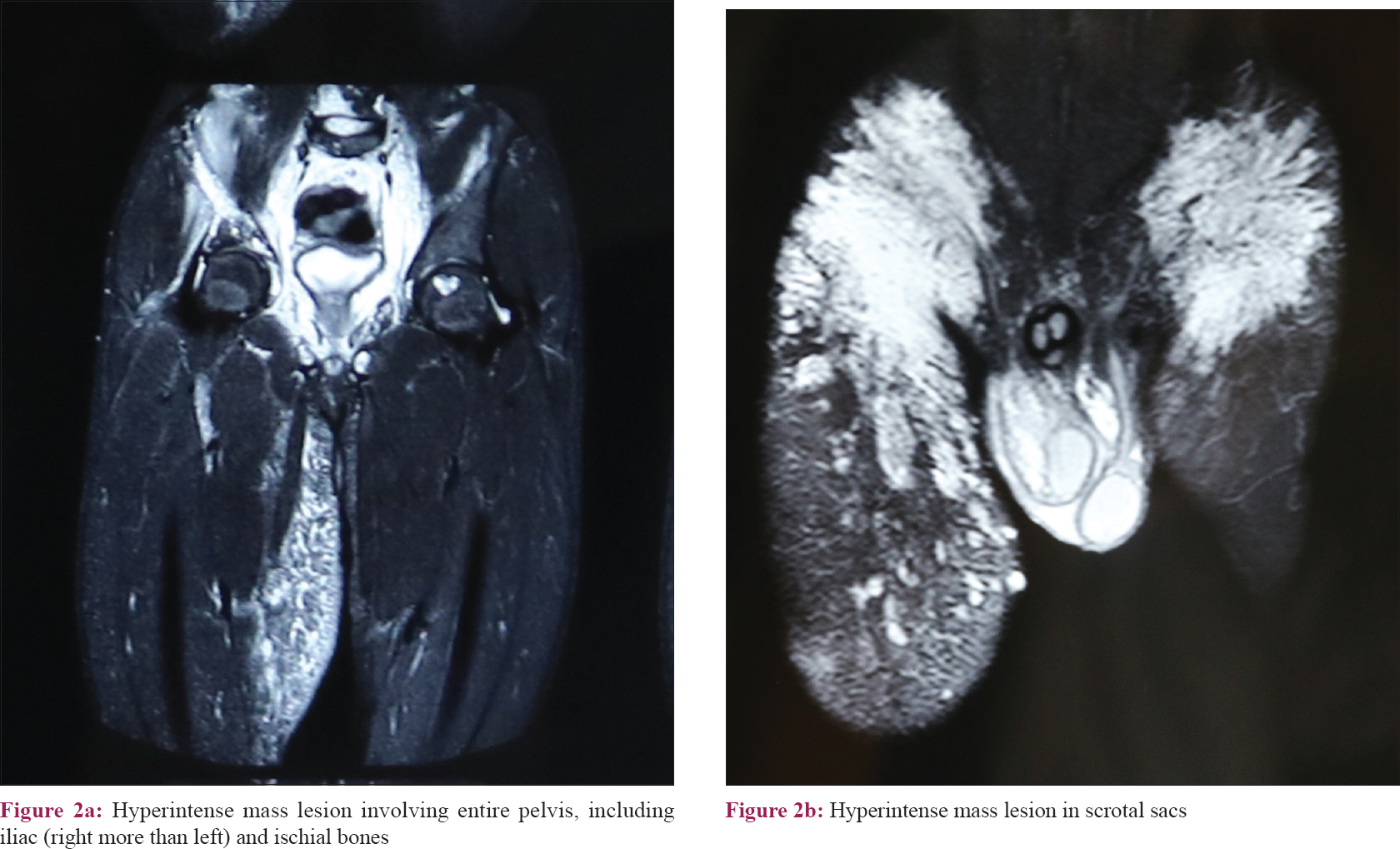
A 15-year-old boy presented with asymptomatic raised lesions over the right side of scrotum and the right thigh since 4 years, with history of discharge from the scrotal lesions. Cutaneous examination revealed multiple, 2–3 mm, flat topped, yellowish-white papules with smooth surface, arranged in serpiginous pattern on the right hemiscrotum along with scrotal edema [Figure - 1]a. Multiple, discrete, skin-colored, soft, cystic papules, 3–7 mm were seen over the right upper thigh. At 51 cm, the midthigh girth of the right lower limb was much greater than the midthigh girth of the left lower limb, which was 44 cm. The left groin showed a single large, 15 × 7 cm cystic swelling [Figure - 1]b. Testicular examination was normal. Ultrasonography of the right inguinoscrotal region showed a large thick-walled hyperechoeic collection with internal echoes and septation within the right hemiscrotum. The right scrotal wall appeared thickened with evidence of edema. Subcutaneous edema was noted over both the right and left inguinal regions (left more than right). Magnetic resonance imaging (MRI) of the scrotum and local parts revealed diffuse multicompartmental T2 hyperintense infiltrative mass lesion with mild postcontrast enhancement involving the pelvis, ileum, ischial bones, subcutaneous and intermuscular planes, anterior (medial and lateral) aspect of bilateral thigh, and both scrotal sacs consistent with clinical diagnosis of cystic lymphangiomas [Figure - 2]a and [Figure - 2]b. Histopathologic examination from the lesions over the thigh and scrotum showed numerous collapsed, irregular dilated lymph channels with flattened endothelial cells suggestive of lymphangioma [Figure - 3]. Plastic surgeons opined that surgical treatment would be considered if the lesions become symptomatic.
 |
| Figure 1: |
 |
| Figure 2: |
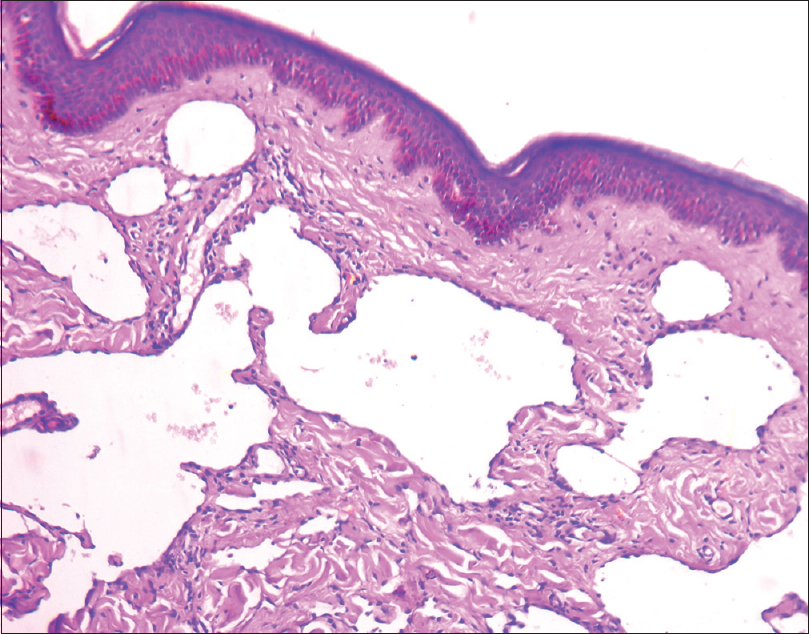 |
| Figure 3: Biopsy (H and E, ×100) – numerous collapsed, irregular dilated channels in the upper dermis with flattened endothelial cells |
Case 2
A 10-year-old boy presented for evaluation of asymptomatic lesions on the right buccal mucosa with swelling of cheek and lips on the right side since 1 year. The lesions had gradually increased to the present size, with gradual involvement of left buccal mucosa also. He had difficulty in mastication. Cutaneous examination revealed multiple, soft, flesh-colored, 2–3 mm papules extending in a linear fashion from the inner aspect of the right lower lip to the buccal mucosa, with discrete papules adjacent to the linear lesions [Figure - 4]a and [Figure - 4]b. Few similar papules were seen on the left buccal mucosa. There was associated edema of the right cheek and right side of upper and lower lip. Biopsy was consistent with lymphangioma. Ultrasound showed multiple, unilocular, sub centimeter sized, noncommunicating cystic spaces in the submucosal and intramuscular planes in the right cheek, with few similar spaces also seen on the left submucosal plane. MRI lymphangiography showed abnormal T2 hyperintense lesions involving bilateral buccal mucosa with minimal postcontrast enhancement without any bony involvement. One USG-guided sclerotherapy treatment using injection polidocanol (40% dilution) was done by the radiology department with marked reduction in lesions, clinically and radiologically, at the end of 6 months [Figure - 5].
 |
| Figure 4: |
 |
| Figure 5: Postsclerotherapy (end of 6 months) using polidoconol with marked reduction in right buccal mucosa lesions |
Discussion
Buccal lymphangiomas with different presentations have been reported in children. Cases reported by Yoganna et al. and Kaur et al. in 2014 and 2015 had congenital and acquired unilateral buccal lymphangioma presenting as diffuse swelling with overlying translucent papules,[5],[6] with similar lesions on the right commissural region of the lip.[6] Devi et al. in 2016 reported two unilateral cases, one with palatal extension.[3] Our case was primary, late onset, with vesicles over both cheeks, extending on the inner aspect of the right side of the lower lip, but with unilateral cheek swelling.
Of the 30 cases of genital lymphangiomas, most had scrotal lymphangiomas; few had inguinoscrotal and penoscrotal presentation. Vikicevic et al. reported similar presentation like ours, but with the additional feature of cryptorchidism.[7] Sheth et al. reported a cystic hygroma involving the soft tissue of thigh, scrotum, and pelvis on ultrasonogram.[8] Similar areas of involvement were seen in our case, with the additional finding of pelvic bone involvement. Our case had late onset and predominant involvement of the right side of scrotum, thigh, and groin with extension to the left groin, leading to limb girth discrepancy, with additional evidence of pelvic bone involvement on MRI with contrast.
Morphological classification of lymphangiomas includes macrocystic, microcystic, and mixed variants.
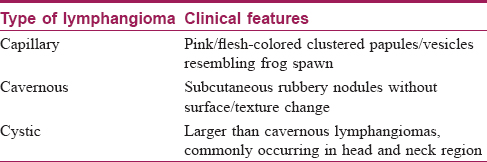
They can be categorized into capillary, cavernous, and cystic lymphangioma, the clinical features being mentioned in [Table - 3].[6]
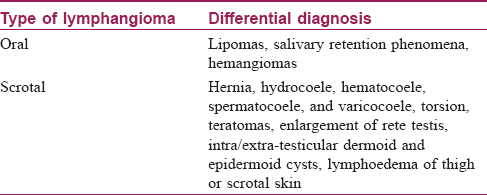
[Table - 4] includes differential diagnosis of oral and scrotal lymphangiomas.[2],[5]
Biopsy confirms diagnosis, ultrasonography detects cystic nature and fluid component, and helps in planning the surgical approach in scrotal lymphangiomas. Angiography rules out vascular lesions and computed tomography/MRI detects extension to adjacent structures.[2]
Treatment includes surgical excision, radiation, cryotherapy, electrocautery, sclerotherapy, embolisation, ligation, lasers, and observation.[9]
For recurrent, residual, unresectable/surgically challenging lesions, sclerotherapy with 25% dextrose, hypertonic saline, bleomycin, and picibanil (OK-432) is recommended.[4] Sclerotherapy leads to total regression of lesions, as endothelial lining of lymphangiomas is vulnerable to chemical irritants. Polidocanol (hydroxypolyathoxydodecan) is a liquid surfactant that acts as an endothelial irritant inducing thrombosis and fibrosis around the vascular space into which it is injected. Jain achieved a volume reduction of 96%–100% in three patients with lymphangiomas with polidocanol.[10]
Conclusion
Awareness of occurrence of lymphangiomas at rare sites like oral cavity/scrotum is important to avoid misdiagnosis and for initiation of appropriate treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Grasso DL, Pelizzo G, Zocconi E, Schleef J. Lymphangiomas of the head and neck in children. Acta Otorhinolaryngol Ital 2008;28:17-20.
[Google Scholar]
|
| 2. |
Patoulias I, Prodromou K, Feidantsis T, Kallergis I, Koutsoumis G. Cystic lymphangioma of the inguinal and scrotal regions in childhood – Report of three cases. Hippokratia 2014;18:88-91.
[Google Scholar]
|
| 3. |
Devi A, Narwal A, Yadav AB, Singh V, Gupta A. Classical cases of lymphangioma – As multiple vesicular eruptions. J Clin Diagn Res 2016;10:ZD22-3.
[Google Scholar]
|
| 4. |
Dogan N, Durmaz CE, Sencimen M, Ucok O, Okcu KM, Gunhan O, et al. The treatment of recurrent lymphangioma in the oral buccal mucosa by cryosurgery: A case report. OHDMBSC 2010;9:7-10.
[Google Scholar]
|
| 5. |
Yoganna SS, Rajendra Prasad RG, Sekar B. Oral lymphangioma of the buccal mucosa a rare case report. J Pharm Bioallied Sci 2014;6:S188-91.
[Google Scholar]
|
| 6. |
Kaur M, Gombra V, Subramanyam RV, Hasan S. Lymphangioma of the buccal mucosa-A case report and review of literature. J Oral Med Oral Surg Oral Pathol Oral Radiol 2015;1:123-5.
[Google Scholar]
|
| 7. |
Vikicevic J, Milobratovic D, Vukadinovic V, Golubovic Z, Krstic Z. Lymphangioma scroti. Pediatr Dermatol 2007;24:654-6.
[Google Scholar]
|
| 8. |
Sheth S, Nussbaum AR, Hutchins GM, Sanders RC. Cystic hygromas in children: Sonographic-pathologic correlation. Radiology 1987;162:821-4.
[Google Scholar]
|
| 9. |
Haroon S, Hasan SH. Lymphangioma circumscriptum in the scrotum: A case report. J Med Case Rep 2012;6:233.
[Google Scholar]
|
| 10. |
Wiegand S, Eivazi B, Zimmermann AP, Sesterhenn AM, Werner JA. Sclerotherapy of lymphangiomas of the head and neck. Head Neck 2011;33:1649-55.
[Google Scholar]
|
Fulltext Views
5,645
PDF downloads
3,549





