Translate this page into:
Malignant melanoma with metastasis to the male breast
Correspondence Address:
Seung-Ki Kim
Department of Surgery, CHA Bundang Medical Center,CHA University, 59 Yatap-ro Bundang-gu Seongnam-si Gyeonggi-do
Korea
| How to cite this article: Kang BS, Kim SK. Malignant melanoma with metastasis to the male breast . Indian J Dermatol Venereol Leprol 2014;80:566-568 |
Sir,
Although primary breast cancer is the most common malignancy in women worldwide, metastasis to the breast from other sites is rare, accounting for 0.5-2% of all breast malignancies. [1] The source of metastasis is mainly contralateral breast cancer and extramammary tumors, including lymphoma, lung cancer, and malignant melanoma. [2] Approximately 20% of malignant melanomas result in metastasis, with the most common metastatic sites being the liver, lung, and brain. [3] Breast metastasis from malignant melanoma is uncommon and most case reports involve female patients. We report a case of metastatic malignant melanoma in the breast of a male patient.
A 62-year-old man was referred to the breast clinic from the dermatology department with a recently detected palpable left breast mass and soreness. He had a history of a posterior auricular cutaneous malignant melanoma that was excised 8 years previously. On physical examination, a 4 × 2 cm firm mass was palpable in the upper outer quadrant of the left breast. The overlying skin showed thickening without pigmentation [Figure - 1]a. Mammography showed bilateral nodular gynecomastia and a well-defined lobulated hyperdense mass in the upper outer quadrant of the left breast [Figure - 1]b. Ultrasonography revealed a 4.5 × 2.5 × 1.1 cm lobulated, complex echoic mass with a thick echogenic halo in the surrounding parenchyma [Figure - 1]c. Fine-needle aspiration cytology showed a few atypical cells in a necrotic background. Considering the history of malignant melanoma, immunohistochemical staining was performed for markers such as HMB-45, Melan-A, and S-100, which were focally positive. Surgical excision was planned because the results were highly suspicious for, although not diagnostic of, metastatic melanoma. There was no evidence of any other metastatic lesion on abdomen-pelvic, and chest computed tomography and a whole body positron emission tomography. Partial mastectomy and sentinel lymph node biopsy using indigo carmine were performed. A dye-tinged single lymph node was dissected and submitted for frozen section analysis and was subsequently deemed to be free of tumor. The haematoxylin and eosin (H and E) staining of the excised tissue showed pleomorphic tumor cells with abundant cytoplasm, large vesicular nuclei, prominent nucleoli and frequent mitoses [Figure - 2]a. The immuno-histochemical staining results for S-100, HMB-45, and Melan A were positive, confirming the diagnosis of metastatic melanoma [Figure - 2]b-d.
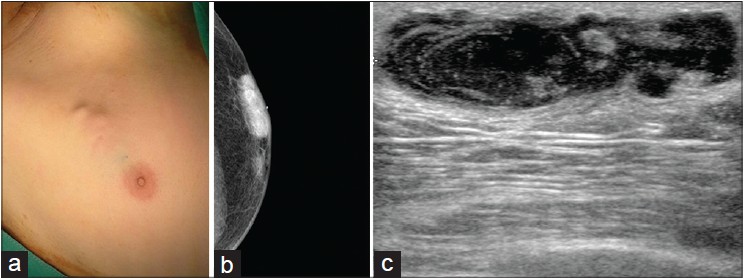 |
| Figure 1: (a) Approximately 4 x 2 cm firm mass at the left upper outer breast with no apparent skin pigmentation. (b) Bilateral gynecomastia and well-defined, lobulated hyperdense mass on mammography. (c) Approximately 4.5 x 2.5 x 1.1 cm oval, complex echoic mass with thick echogenic halo in the surrounding parenchyma on breast ultrasonography |
 |
| Figure 2: (a) Pleomorphic tumor cells with abundant cytoplasm, large vesicular nuclei, prominent nucleoli and frequent mitosis. H and E (×400), (b) Strongly positive immunohistochemical staining of neoplastic cells with S-100 (×100), (c) Strongly positive immunohistochemical staining of neoplastic cells with HMB-45 (×100), (d) Strongly positive immunohistochemical staining of neoplastic cells with Melan-A (×100) |
Breast metastases from extramammary malignancies are uncommon, and when they do arise, the main primary lesions are lymphoma, lung cancer, and malignant melanoma. Most such cases are reported in females; reports in males are very rare. The role of estrogen in the development and progression of melanoma is still controversial, but epidemiologic evidence is accumulating. [2],[3],[5] There is no identified predisposing factor for metastasis to the breast from extra-mammary tumors. [1] However, in the case of men with a history of prostatic cancer, estrogen therapy could be a predisposing factor. [4] Most earlier reports of melanoma metastatic to the breast were in premenopausal women with an average age at metastasis of 38-40 years. Metastatic melanoma to the breast frequently occurs in the upper outer quadrant of the breast as a single lesion. [3],[4] This may be explained, in part, by the good vascularity and abundant glandular tissue of younger patients, particularly in the upper outer area of the breast. The rarity of metastatic melanoma to the breast in men might be a result of the comparatively scant glandular tissue in the male breast. In young patients, the tumor may be difficult to differentiate from fibroadenoma on mammography and ultrasonography as it is seen as a well-marginated, round mass. Fine-needle aspiration cytology or core biopsy should be performed to confirm the diagnosis but a pathological diagnosis can also be difficult because of histological variability. A definitive diagnosis is possible by immunohistochemical staining for melanocytic markers. S-100 is the most sensitive diagnostic marker for melanoma, and immunohistochemical staining should be performed for this marker along with one or more other markers such as Melan-A, tyrosinase, or HMB-45.
The standard treatment for metastatic malignant melanoma to the breast is wide local excision with clear resection margins. A sentinel lymph node biopsy of the axilla may be considered but has no proven therapeutic value and a minor risk of morbidity. After local excision, systemic chemotherapy should be administered as an adjuvant treatment. Breast metastasis from malignant melanoma does not usually occur as an isolated lesion and presents in conjunction with disseminated disease, including metastases to the lung, liver, or brain. [5] In our case, we could not find any other metastasis at the time of diagnosis. Prognosis of breast metastasis from malignant melanoma has been reported as being poor. [1]
In conclusion, metastatic melanoma to the breast is rare, especially in men. For accurate diagnosis and treatment, clinical suspicion is essential. When a breast lump is detected in a patient with previously diagnosed malignant melanoma, metastatic melanoma must be included in the differential diagnosis.
| 1. |
Loffeld A, Marsden JR. Management of melanoma metastasis to the breast: Case series and review of the literature. Br J Dermatol 2005;152:1206-10.
[Google Scholar]
|
| 2. |
Satoru T, Nayuko S, Hiroya F, Yuko T, Lpsei K, Mitsuhiko I, et al. A case of solitary breast metastasis from malignant melanoma of the nasal cavity. Oncol Lett 2012;4:889-92.
[Google Scholar]
|
| 3. |
James M. Bilateral breast masses as initial presentation of widely metastatic melanoma. J Surg Oncol 1999;72:175-7.
[Google Scholar]
|
| 4. |
Toombs B, Kalisher L. Metastatic disease to the breast: Clinical, pathologic, and radiologic features. Am J Roentgenol 1977;129:673-6.
[Google Scholar]
|
| 5. |
Larisa R, Wiliam AR, Karl L, Rene G. Metastatic melanoma in the breast: A report of 27 cases. J Surg Oncol 2006;94:101-4.
[Google Scholar]
|
Fulltext Views
3,955
PDF downloads
2,034





