Translate this page into:
Management of Darier disease: A review of the literature and update
Corresponding author: Dr. Roger N. Haber, Department of Dermatology, Saint George Hospital University Medical Center, Beirut, Lebanon. rnhaber@stgeorgehospital.org
-
Received: ,
Accepted: ,
How to cite this article: Haber RN, Dib NG. Management of Darier disease: A review of the literature and update. Indian J Dermatol Venereol Leprol 2021;87:14-21.
Abstract
Darier disease (DD) is a rare type of inherited keratinizing disorder with no definitive therapeutic approach. The objective of this study is to provide a detailed literature review of all the available treatment modalities of Darier disease, including those that are both surgical and non surgical, to compare their efficacies and to propose a novel therapeutic approach. A complete search of the literature for all articles describing the different treatments of Darier disease, with no restrictions on patients’ ages, gender or nationalities, was performed with the use of PubMed. A total of 68 articles were included in the study: 3 prospective studies, 44 case reports/case series and 21 letters/correspondences/clinical images. The treatments described were topical, oral or physical. Retinoids (isotretinoin, tazarotene and adapalene) and fluorouracil were the two most effective topical treatments. Oral retinoids were the most effective oral therapy and were prescribed in the cases of generalized Darier disease. For localized and resistant skin lesions, physical therapies including surgical excision, dermabrasion and CO2 laser ablation were the first line choices. Limitations of this article include the inability to verify the accuracy of the published data, the relatively small sample size, the absence of randomized controlled clinical trials and possible unidentified confounding factors in various studies. In every therapeutic approach to Darier disease, consideration of patient comorbidities, disease distribution, severity and treatment accessibility is essential. Large and randomized clinical trials are necessary for the comparison of the efficacy and the safety of all the treatments of Darier disease and settling a consensus for management.
Keywords
Darier
laser
surgery
systemic
topical
treatment
Introduction
Darier disease (DD), first reported by Darier1 and White2 in 1889, is an autosomal dominant skin disorder caused by a genetic mutation of the ATP2A2 gene on chromosome 12.3 It is clinically characterized by multiple firm, greasy and hyperkeratotic papules that coalesce into plaques, mostly affecting seborrheic regions. Nail involvement is also observed.4 Characteristic histological features include acantholysis with suprabasal separation, focal dyskeratosis of the keratinocytes and overlying epidermal orthokeratosis.
To date, there is no consensus on the treatment of Darier disease, and current treatment methods range from simple medical and non invasive treatments to invasive surgical interventions.
The aim of this study is providing a complete review of all of the available data on the efficacy and safety of these treatments and to suggest a therapeutic algorithm for Darier disease.
Methods
On October 2019, an extensive review of the English and French published literature using the PubMed databases was conducted using the following key words:
(Darier OR Darier-White OR keratosis follicularis) AND (treatment OR topical OR systemic OR retinoids OR cyclosporine OR doxycycline OR laser OR photodynamic therapy PDT OR surgery OR gene therapy). The references of included articles were manually screened for additional pertinent articles. Studies were selected based on titles and abstracts and were then obtained and read in full.
The studies that were included were published from November 1987 to date. Unavailable articles were not included unless the abstract was available. Articles that were written in any other language apart from English or French were excluded. The authors agreed upon the final selection of the included studies as shown in Figure 1; any disagreement was solved by discussion. The descriptive data for each included study was recorded as follows: (i) first author and year of publication; (ii) study design; (iii) type of treatment and dose; (iv) treatment duration; (v) number of patients; (vi) mean age of patients; (vii) gender; (viii) failed treatments; (ix) outcome; (x) side effects; (xi) relapse. Every article had specific clinical definitions for remission and relapse of the disease after treatment with the use of various adjectives. In this article, remission was defined as the reduction or disappearance of the signs and symptoms of the disease; relapse was defined as the subsequent return of symptoms after a period of improvement. No chronologic constraints were set to define remission or relapse due to the chronicity of this disease and the fact that none of the treatments had the intention to cure.
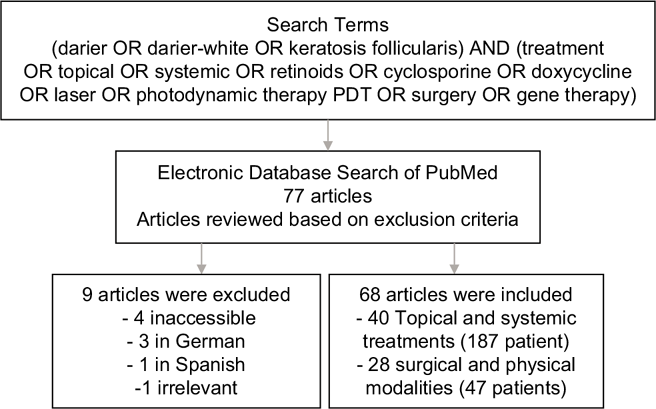
- Stepwise approach for article inclusion
Results
The initial search yielded a total of 77 articles. Of those, 9 records were excluded after title and abstract revision and 68 articles were included: 3 prospective studies, 44 case reports/case series and 21 letters/correspondences/clinical images, thus rendering the quality of evidence suboptimal. In total, 187 patients received oral and topical treatments and 42 patients were treated with physical therapies. Treatments were either single-agent or multi-agent regimens. The stepwise approach for study selection is summarized in Figure 1. Table 1 displays the different treatment characteristics including: number of treated patients, percentage of efficacy and tolerability. Treatment was reported as effective when the primary authors of the articles clearly stated a significant clinical improvement. An inconclusive result was evaluated by the main authors (RH and ND) by reviewing the pictures and/or the clinical description in the texts and a final conclusion was drawn.
| Treatment | Number of patients | Percentage of patients who improved, n (%) | Side effects |
|---|---|---|---|
| Topical isotretinoin | 19 | 8 (42) | Mild to severe burning/erythema/irritation |
| Diclofenac sodium 3% | 3 | 3 (100) | Irritation |
| Diclofenac sodium 1% | 1 | 1 (100) | - |
| Tazarotene | 4 | 4 (100) | Dryness, irritation |
| Adapalene | 3 | 3 (100) | None |
| 5-FU | 11 | 11 (100) | None |
| Tacalcitol | 1 | 1 (100) | - |
| Tacrolimus | 1 | 1 (100) | - |
| Alitretinoin | 7 | 7 (100) | Mild dryness of eyes, moderate reversible hair loss, headache, aseptic cellulitis, enlarging pyogenic granuloma, erosions, fever, mild dyslipidemia |
| Alitretinoin + 5-FU | 1 | 1 (100) | - |
| Cyclosporine | 4 | 3 (75) | None |
| Doxycycline | 2 | 2 (100) | None |
| Etretinate | 1 | 1 (100) | Stomatitis |
| Microgynon | 1 | 1 (100) | Weight gain |
| Fatty acids | 16 | 13 (80) | - |
| Cetirizine | 1 | 0 (0) | - |
| Magnesium chloride | 1 | 1 (100) | Unpleasant taste |
| Naltrexone | 6 | 2 (33) | - |
| Isotretinoin | 104 | 99 (95) | Dry skin and mucosa |
| Botulinum toxin | 3 | 3 (100) | None |
| CO2 laser ablation with dermabrasion | 2 | 2 (100) | - |
| CO2 laser ablation | 7 | 7 (100) | Irritation, edema, crusting |
| Erbium YAG | 3 | 3 (100) | Hypopigmentation |
| PDL | 8 | 6 (75) | HSV superinfection |
| FPDL | 1 | 1 (100) | Purpura, mild crusting |
| Electron beam radiation therapy | 1 | 1 (100) | Dermatitis, desquamation |
| Photon beam radiation therapy | 3 | 3 (100) | Severe ulceration upon re-irradiation |
| Electro surgery | 2 | 2 (100) | Serous drainage |
| PDT with topical 5-ALA 20% | 7 | 5 (71) | Erythema, exudation, discomfort, pruritus, pain |
| PDT with MAL (methylaminolevulinate) | 1 | 1 (100) | Mild self-limiting inflammatory response |
| Focal multimodality radiation therapy (electron beam, IMRT, brachytherapy) | 1 | 1 (100) | Severe complications requiring hospitalization |
| Surgery | 6 | 6 (100) | Dehiscence of wound, necrosis |
n: Number of patients, 5-FU: Fluorouracil, CO2: Carbon dioxide, PDL: Pulsed dye laser, Erbium YAG: Erbium-doped yttrium aluminium garnet laser, PDL: Pulsed dye laser, FPDL: Flashlamp-pumped pulsed-dye laser, PDT: Photodynamic therapy, ALA: Aminolevulinic acid, MAL: Methylaminolevulinate, IMRT: Intensity modulated radiation therapy, HSV: Herpes simplex virus
Discussion
At present, there are no proven curative treatments for Darier disease; the majority of cases are treated symptomatically to improve pruritus and irritation. Use of emollients, soap substitutes and cotton clothing are recommended. Sunblock is advocated for patients with a history of photo aggravation. Avoiding exacerbating factors such as high temperature, high humidity, UV rays and mechanical irritation is also essential. Lithium carbonate has also been reported to exacerbate Darier disease.5,6 Special care should be taken to avoid bacterial (mainly with Staphylococcus and Streptococcus species), viral (mainly herpes simplex virus) and trichophytic infections. Spontaneous improvement is observed in approximately one third of patients.6
Topical treatments
Topical retinoids
Topical isotretinoin had been used in a total of 19 patients.7-11 In 16 patients with a mean age of 43 (half of which were males), a formulation of 0.05% applied twice daily for 3 months was used. Of those, 6 (35%) patients showed complete resolution of symptoms with only 1 patient experiencing a relapse following a month of treatment discontinuation. Erythema, burning and irritation were reported by 11 (75%) patients.
Formulations of 0.1% isotretinoin were used by 3 patients for 1 to 3 months, with complete resolution of symptoms in 1 patient. All 3 patients complained of experiencing either erythema or burning.
Tazarotene is thought to be more specific to the retinoid receptor compared to 13-cis-retinoic acid and is associated with fewer side effects.12-14 A total of 4 women with a mean age of 45 years used Tazarotene 0.05% and 0.1% daily with complete resolution of their symptoms. Dryness and irritation were still reported by 1 patient, and another had relapse on the forehead and the back after 1 year.
Adapalene gel, a synthetic retinoid, was used in a total of 3 patients at a concentration of 0.1% daily for 2 months; all showed marked improvement with no side effects.15-17
Fluorouracil (5-FU)
DNA synthesis is inhibited by fluorouracil, a drug that was shown to be effective in treating Darier disease with a good safety profile. A total of 11 patients (eight females, three males) have been reported to use topical 5-FU at dosages of 1%, 5% or 20% for severe and resistant-to-therapy Darier disease. All patients showed marked improvement and resolution after 2 weeks of treatment but relapsed after treatment cessation. No patients experienced side effects.18-22
Diclofenac sodium
Diclofenac sodium 3% was used twice a day in 3 patients for 3 to 8 months with marked improvement and near resolution of all the lesions.23,24 Among these, 1 patient complained of irritation and had recurrence of lesions 3 months after stopping the treatment.
Diclofenac sodium 1% was used twice a day in 1 patient for 1 month with marked flattening of the lesions except at the soles.25
Tacalcitol
Tacalcitol was used in a 39-year-old female with substantial improvement and no relapse after 5 months.26
Tacrolimus
Tacrolimus 0.1% was used twice a day in a 22-year-old female with remission after 8 weeks and no relapse for up to 1 year after the treatment.27
Topical steroids
Even though topical steroids are widely used in the treatment of Darier disease, no trials to date were found to support their use and efficacy. They have mostly been used in association with retinoids to reduce irritation. Similarly, a combination of steroids and antibiotics may be justified based on the risk of bacterial super-infections in some patients as seen in clinical practice.
Oral treatments
Oral retinoids
Burge et al. were the first to use oral etretinate in 1981, at a dose of 0.5–1.0 mg/kg in 18 patients with Darier disease, 17 of which improved.28 Adverse effects were dose-related; they included dryness of mucosal surfaces, soreness, nosebleeds, thinning of the skin and increase of pruritus. Of these patients, 6 (33%) interrupted treatment 3 years later due to side effects.29
Localized Darier disease of the scalp was treated successfully with oral etretinate at 40 mg/day in 1 case report.30 However, the patient developed stomatitis and was obliged to stop the treatment with subsequent relapse of his lesions. Oral etretinate was then reintroduced at a lower dose (20 mg/day) with adequate control of the disease.
Efficacy of acitretin in Darier disease was assessed in 1 case series where 4 out of the 5 patients improved, using starting doses of 35 mg daily for the first 3 months then adjusting the dose according to the response.31 In another article, acitretin was used to treat 13 patients with a dose starting at 30 mg per day for 16 weeks.32 All subjects showed improvement; adverse effects included itching in 5 patients and diffuse alopecia in 2.
A double-blind study of 26 patients compared the efficacy of acitretin and etretinate in the treatment of Darier disease and found no significant difference between the two drugs.33
Isotretinoin has also been used in the treatment of this disease for many years.34,35
In a large, multicentre, open study published in 1982, isotretinoin was used in 104 patients.36 It was found to be very effective with 73 (70%) patients showing clinical improvement after 1 to 4 weeks according to both patients and the physicians.36 The starting dose that was used was 0.5 mg/kg and the maintenance dose was adjusted according to symptoms. Some patients were maintained on alternate day or alternate week regimens, but long-term remission was not achieved. Out of the 104 participants, 5 had no improvement. Bhat et al. used oral isotretinoin at a dose of 20 and 40 mg/day along with a steroid taper for 2 patients with diffuse Darier disease with nail involvement with marked improvement.37
Alitretinoin (9-cis retinoic acid) was used for a total of 7 patients with rather generalized Darier disease, all of which showed marked improvement of symptoms at a dose of 30 mg/day over a period of at least 1 month; 6 of them, however, relapsed.38-42 Alitretinoin at 30 mg/day was also used in association with 5-FU on a daily basis in a 43-year-old male who achieved complete remission after 4 months.43 The disease relapsed when the dose was decreased to 20 mg/day, so the patient continued taking 30 mg/day of alitretinoin. Follow up after three and a half years showed no relapse.
Cyclosporine
Cyclosporine 3 mg/kg/day was found to be helpful in treating 2 middle-aged male patients with widespread eczematized Darier disease.44,45 Relapse after stopping the treatment for 3 months was noted in 1 of these patients who had found almost complete resolution of his disease after 10 weeks of treatment.45 Another report showed that cyclosporine 6 mg/kg/day for 8 weeks lead to complete resolution in a patient and to minimal improvement in another.46
Doxycycline
Commonly used for treatment of acne, doxycycline 100 mg/day was recently used in the treatment of Darier disease and was found to have positive outcome in 2 female patients without any reported side effects.47,48
Microgynon
Microgynon, a combined oral contraceptive pill (ethinylestradiol 50 μg, levonorgestrel 125μ g) was used in the treatment of 1 female patient with reduction of itching and improvement in skin fragility over 2 years.49 The main side effect observed was mild weight gain. Clinical improvement persisted despite stopping the medication for 1 week every 3 weeks.
Epsy et al. also administered oral contraceptive pills for 5 women with premenstrual exacerbation of disease symptoms, and the lesions almost completely resolved in 4.50 This suggests a hormonal influence in the pathogenesis of this disease.51
Fatty acids
In a study of 14 patients with Darier disease, 13 patients responded to fatty acid supplementation; 6 of those patients who complained of sunlight sensitivity showed better sunlight tolerance during treatment.52 The rationale of using fatty acids as a treatment can be related to the clinical similarities between essential fatty-acid deficiency and Darier disease. Reduced levels of delta 6-desaturated metabolites of linoleic and alpha-linoleic acids have also been observed in these patients.
Cetirizine
Cetirizine, a second generation H1 antihistamine, was used in a case report of a 55-year-old woman with a vesiculobullous variant of Darier disease.53 She was given cetirizine 10 mg daily that was increased to 40 mg daily over the period of 4 weeks. The patient had marked improvement of burning sensation, however, the lesions persisted.
Magnesium chloride
Magnesium chloride was used in an 11-year-old boy suffering from Darier disease with lesions scattered over the neck, abdomen and inguinal folds with more severe involvement of the scalp.54 With the administration of 1 month of oral magnesium chloride at a dosage of 300 mg daily, he had marked improvement in most of the areas except the scalp. No relapse was observed 1 month after stopping the treatment.
Naltrexone
Boehmer et al. used naltrexone to treat 6 patients with Darier disease after it was shown to be effective in patients with Hailey–Hailey disease and based on the similarities in pathophysiology of the 2 diseases.55-58 Naltrexone was used off-label at a dose of 5 mg with 200 mg of magnesium supplementation. Patients were followed up every 4 weeks for 12 weeks. Those with severe disease had worsening of symptoms after an initial improvement. The 2 patients with mild and moderate disease showed almost complete remission and flattening of the lesions after 12 weeks of treatment. To note, 1 of these 2 patients was also taking oral acitretin.
Physical approaches
Dermabrasion
Skin dermabrasion reaching down to the papillary dermis was used to treat 12 patients with Darier disease; 75% of the treated skin remained disease free 2 1/2later.59,60 Dermabrasion in conjunction with deep dermal excision was also successful in 1 patient.61
Electrosurgical excision
Electrosurgical excision was used in 2 patients who had etretinate resistant disease with good results.62
Surgical excision
In 1985, deep surgical treatment for refractory and hypertrophic Darier disease lesions over the areola of a 50-year-old man was performed with local anesthesia and debridement extending down to the level of the superficial dermis; re-epithelialization occurred 4 weeks later and the procedure was successful.63 Surgical treatment has also been used in conjunction with systemic retinoids with variable results.64 A 25-year-old male patient with perianal involvement showed favorable outcomes with surgery alone and no relapse was noted after 6 months; the patient had wound dehiscence prior to complete healing.65 A similar case of a 22-year-old male patient suffering from perianal lesions was successfully managed with surgical excision; no follow up was mentioned.66
Reduction mammoplasty was similarly used in a 46-year-old female patient with Darier’s disease involving the breast area, with near complete remission of the lesions.67
Darier’s disease involving the nail is very difficult to treat; 2 patients were treated with nail avulsion yielding good results.68,69
Botulinum toxin
Botulinum toxin administered every 6 months showed good results in 3 middle-aged patients with Darier disease at the intertriginous areas.70-72 No side effects were noted. In 1 patient, 100 units of BTX-A (BOTOX, Allergan) were diluted in 4 mL of 0.9% NS; 50 units were used to treat the left submammary area with 2.5 units (0.1 mL) injected 2 cm apart using a 30 G needle.70 In the second patient, 40 units were used in each inguinal fold and 20 units in the anal fold, with injections 2 cm apart using a 30 G needle.71 For the third patient, 200 units were injected in the intergluteal folds 1 cm apart with 2.5 units at each site.72
CO2laser ablation
Carbon dioxide laser ablation was used after surgery in 2 cases with good outcome.73,74 It was also successful in the treatment of 7 patients with chronic and resistant Darier disease.75-79 Mild erythema and edema were reported, and recurrence rates were minimal.
Erbium laser
With the use of erbium-doped yttrium aluminium garnet laser (Er: YAG laser), 2 patients with diffuse pruritic lesions in the upper body showed complete resolution.80 No hypo pigmentation was noted after treatment and no relapse was seen after 2 years of follow up. Another patient was treated with a 1,550 nm erbium doped fiber laser resulting in 75% improvement.81 Side effects included pain, erythema and mild edema.
Pulsed dye laser
Schmitt et al. used 595 nm pulse dye laser (PDL) with satisfactory results in 2 patients suffering from Darier disease.82 Cannarozzo et al. also used the 595 nm PDL to treat 8 patients, 4 of which had excellent results.83 The rest had moderate improvement. To note, 2 patients had superimposed HSV infection following the treatment. Half of the patients reported no recurrence and half had relapse of their disease 18 months after treatment.
Flashlamp-pumped pulsed-dye laser
Roos et al. successfully used FPDL in a 42-year-old female with submammary Darier disease with marked improvement.84
Radiation therapy
Patients undergoing radiation therapy for cancer treatment were found to have unexpected improvement in their symptoms of Darier disease.85,86 Kittridge et al. used electron beam radiation therapy in a patient that resulted in a good outcome but was complicated with severe dermatitis requiring ICU admission.87 Follow up in 18 months showed no relapse.
Photon beam therapy, known to have deeper penetration than electron beam radiation therapy, was used in 3 patients with recalcitrant disease and thickened hyperkeratotic lesions.88 Significant and sustained improvement was observed in these patients after the first session; one of them suffered from ulcerations at the site of treatment after re-irradiation. Focal multimodality radiation therapy was used in a 36-year-old female patient.89 She had excellent persistent response with electron beam therapy to the lower abdomen and neck along with moderate improvement with intensity modulated radiation therapy (IMRT) to the pelvis, abdomen and inframammary folds. The reappearance of pelvic lesions occurred 18 months later, so the patient underwent re-irradiation with electron beam to the vulva along with brachytherapy to the buttocks to limit internal organ radiation. The patient had sustained remission 1 month later.
To note, caution must be taken knowing the increased risk of malignancy and ulceration from radiation therapy.
Photodynamic therapy
Photodynamic therapy using topical 5-amino laevulinic acid (5-ALA) 20% was used in a case series of 6 patients with Darier disease: 2 (33%) had excellent results and 1 (16%) had no clinical improvement.90 Side effects included erythema, exudation, and pain. Westeinde et al. used PDT with topical 5-ALA with no improvement.91 Photodynamic therapy with methylaminolevulinate (MAL) was also used in 1 patient with complete resolution and remission for up to 27 months.92
Limitations
Limitations of this article include inability to verify accuracy of the published data, small overall sample size, absence of randomized controlled clinical trials and possible unidentified confounding factors in various studies.
Conclusion
Till now, there is no consensus on the treatment of Darier disease and most data are limited to case series and case reports. Moreover, no single treatment has demonstrated a clear superiority. Figure 2 suggests a possible therapeutic treatment algorithm for local or disseminated disease.
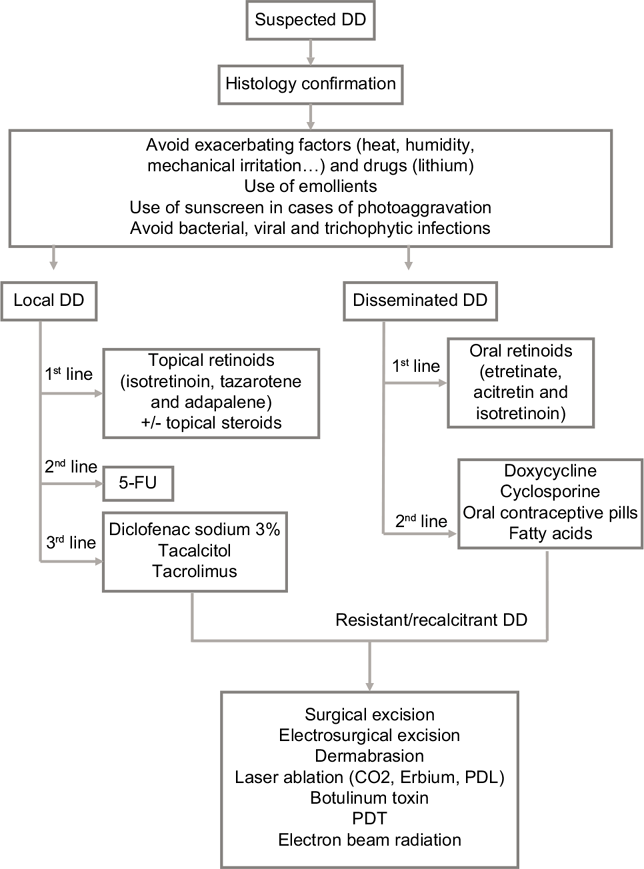
- Treatment algorithm for DD. DD: Darier disease, 5-FU: Fluorouracil, CO2: Carbon dioxide, PDL: Pulsed dye laser, PDT: Photodynamic therapy
The two most effective topical treatments are retinoids (isotretinoin, tazarotene and adapalene) and 5-FU, the latter showing 100% resolution rate but high relapse rates. Oral retinoids remain the mainstay of oral therapy in case of generalized Darier disease. Physical therapies including surgical excision, dermabrasion or CO2 laser ablation can be considered for localized and resistant skin lesions with favorable outcome and variable side effects as shown in Figure 2. The consideration of patient comorbidities, disease distribution, clinician experience and treatment accessibility are mandatory in every therapeutic approach of Darier disease.
Large and randomized clinical trials are necessary to compare the efficacy and the safety of all treatments of Darier disease to reach a more adequate consensus for management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A case of keratosis (Ichthyosis) follicularis. Archives of Dermatol. 1983;119:72.
- [CrossRef] [Google Scholar]
- Mutations in ATP2A2, encoding a Ca2+pump, cause Darier disease. Nat Genet. 1999;21:271-7.
- [CrossRef] [PubMed] [Google Scholar]
- Exacerbation of Darier's disease by lithium carbonate. J Am Acad Dermatol. 1990;23:926-8.
- [CrossRef] [Google Scholar]
- Darier's disease, Treatment with topical vitamin A acid. Arch Dermatol. 1968;98:396-9.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of unilateral Darier's disease with topical isotretinoin. Clin Exp Dermatol. 1999;24:425-7.
- [CrossRef] [PubMed] [Google Scholar]
- Topical isotretinoin in Darier's disease. Br J Dermatol. 1995;133:924-8.
- [CrossRef] [PubMed] [Google Scholar]
- Topical treatment of ichthyoses and Darier's disease with 13-cis-retinoic acid. A clinical and immunohistochemical study. Arch Dermatol Res. 1993;285:221-6.
- [CrossRef] [PubMed] [Google Scholar]
- Topical treatment with 13-cis-retinoic acid improves Darier's disease and induces the expression of a unique keratin pattern. Dermatologica. 1991;182:178-83.
- [CrossRef] [PubMed] [Google Scholar]
- Tazarotene gel for Darier's disease. J Am Acad Dermatol. 1998;38:1001-2.
- [CrossRef] [Google Scholar]
- The treatment of Darier's disease with topical tazarotene. Br J Dermatol. 1999;141:603-4.
- [CrossRef] [PubMed] [Google Scholar]
- Short-contact therapy with topical tazarotene in Darier disease. Actas Dermosifiliogr. 2012;103:255-6.
- [CrossRef] [Google Scholar]
- Successful treatment of Darier's disease with adapalene gel. Pediatr Dermatol. 2011;28:197-8.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of linear Darier's disease with topical adapalene. J Eur Acad Dermatol Venereol. 2009;23:237-8.
- [CrossRef] [PubMed] [Google Scholar]
- Effective treatment of localized Darier's disease with adapalene 0.1% gel. Cutis. 1999;63:227-30.
- [Google Scholar]
- Efficacy and risks of topical 5-fluorouracil in Darier's disease. Ann Dermatol Venereol. 2010;137:455-9.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of Darier disease with topical 5-fluorouracil. Br J Dermatol. 2006;154:1210-2.
- [CrossRef] [PubMed] [Google Scholar]
- Improvement of Darier's disease on treatment with topical 5-fluorouracil. Ann Dermatol Venereol. 2006;133:366-8.
- [CrossRef] [Google Scholar]
- Topical 5-fluorouracil in the treatment of Darier's disease. Br J Dermatol. 1995;133:463-6.
- [CrossRef] [PubMed] [Google Scholar]
- Topical 5-fluorouracil in Darier disease. Br J Dermatol. 2008;158:1393-6.
- [CrossRef] [PubMed] [Google Scholar]
- Improvement of Darier disease with diclofenac sodium 3% gel. J Am Acad Dermatol. 2014;70:e89-90.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of Darier's disease with diclofenac sodium 3% gel. Dermatol Ther. 2017;30:3.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment with diclofenac sodium 1% gel of a case of suspected Darier disease. Clin Exp Dermatol. 2019;44:447-9.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of combination therapy with tacalcitol lotion associated with sunscreen for localized Darier's disease. J Dermatol. 2010;37:718-21.
- [CrossRef] [PubMed] [Google Scholar]
- A case of Darier's disease successfully treated with topical tacrolimus. J Eur Acad Dermatol Venereol. 2006;20:84-7.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of an aromatic retinoid, Tigason (etretinate), in the treatment of Darier's disease. Br J Dermatol. 1981;104:675-9.
- [CrossRef] [PubMed] [Google Scholar]
- The use of Tigason (etretinate) in Darier's disease, Retinoid Therapy. Br J Dermatol Springer 1984:61-2.
- [CrossRef] [Google Scholar]
- Localized Darier's disease of the scalp: Successful treatment with oral etretinate. Dermatology. 2004;208:83-4.
- [CrossRef] [PubMed] [Google Scholar]
- Acitretin monotherapy in Darier's disease. Br J Dermatol. 1989;121:375-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and ultrastructural effects of acitretin in Darier's disease. Acta Derm Venereol. 1988;68:492-8.
- [Google Scholar]
- A double-blind comparison of acitretin and etretinate in the treatment of Darier's disease. Acta Derm Venereol. 1992;72:150-2.
- [Google Scholar]
- Evaluation of 13-cis retinoic acid in lamellar ichthyosis, pityriasis rubra pilaris and Darier's disease. Cutis. 1980;25:380-1, 385
- [Google Scholar]
- Treatment of Darier's disease, lamellar ichthyosis, pityriasis rubra pilaris, cystic acne, and basal cell carcinoma with oral 13-cis-retinoic acid. Dermatologica. 1978;157(Suppl 1):11-2.
- [CrossRef] [PubMed] [Google Scholar]
- Isotretinoin treatment of Darier's disease. J Am Acad Dermatol. 1982;6:721-6.
- [CrossRef] [Google Scholar]
- Darier-White disease in siblings responding to isotretinoin. Indian Dermatol Online J. 2010;1:18-20.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of oral alitretinoin for the treatment of Darier disease: A case report. J Am Acad Dermatol. 2014;71:e46-8.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of Darier disease with oral alitretinoin. Clin Exp Dermatol. 2013;38:523-5.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment with oral alitretinoin in women of childbearing potential with Darier's disease. Br J Dermatol. 2013;169:709-10.
- [CrossRef] [PubMed] [Google Scholar]
- Alitretinoin and Darier disease: All that glisters is not gold. J Am Acad Dermatol. 2015;72:363-4.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of refractory Darier disease with alitretinoin with a follow up of over a year: A case report. Dermatol Ther. 2016;29:222-3.
- [CrossRef] [PubMed] [Google Scholar]
- Combination of alitretinoin and topical 5-fluorouracil in Darier disease. JAAD Case Rep. 2019;5:75-7.
- [CrossRef] [PubMed] [Google Scholar]
- Darier's disease: Severe eczematization successfully treated with cyclosporin. Br J Dermatol. 1994;131:713-6.
- [CrossRef] [PubMed] [Google Scholar]
- Darier-White syndrome and cyclosporin. Dermatology. 1995;190:174-5.
- [CrossRef] [PubMed] [Google Scholar]
- Oral cyclosporine in the treatment of inflammatory and noninflammatory dermatoses. A clinical and immunopathologic analysis. Arch Dermatol. 1990;126:339-500.
- [CrossRef] [PubMed] [Google Scholar]
- Extensive darier disease successfully treated with doxycycline monotherapy. Case Rep Dermatol. 2015;7:311-5.
- [CrossRef] [PubMed] [Google Scholar]
- A case of segmental Darier disease treated with doxycycline monotherapy. Dermatol Online J. 2018;24
- [Google Scholar]
- Oral contraceptives in the treatment of Darier-White disease-a case report and review of the literature. Clin Exp Dermatol. 1996;21:442-4.
- [CrossRef] [PubMed] [Google Scholar]
- Darier's disease: Epidemiology, pathophysiology, and management. Am J Clin Dermatol. 2003;4:97-105.
- [CrossRef] [PubMed] [Google Scholar]
- Essential fatty acids in the treatment of Darier's disease. J Dermatol Treat. 1998;9:97-101.
- [CrossRef] [Google Scholar]
- Vesiculobullous Darier Disease Symptomatically Responsive to Cetirizine. J Drugs Dermatol. 2019;18:213-4.
- [Google Scholar]
- Treatment of Darier's disease with oral magnesium: A case report. SAGE Open Med Case Rep. 2018;6:1-2.
- [CrossRef] [PubMed] [Google Scholar]
- Variable response to low-dose naltrexone in patients with Darier disease: A case series. J Eur Acad Dermatol Venereol. 2019;33:950-3.
- [CrossRef] [PubMed] [Google Scholar]
- Naltrexone for the Treatment of Darier and Hailey-Hailey Diseases. J Cutan Med Surg. 2019;23:453-4.
- [CrossRef] [PubMed] [Google Scholar]
- The uses of naltrexone in dermatologic conditions. J Am Acad Dermatol. 2019;80:1746-52.
- [CrossRef] [PubMed] [Google Scholar]
- Variable Response to Naltrexone in Patients With Hailey-Hailey Disease. JAMA Dermatol. 2018;154:362-3.
- [CrossRef] [PubMed] [Google Scholar]
- Dermabrasion of Hailey-Hailey disease and Darier's disease. J Am Acad Dermatol. 1992;27:136.
- [CrossRef] [Google Scholar]
- Cornifying Darier disease-a unique variant, II. Surgical treatment. Arch Dermatol. 1976;112:504-6.
- [CrossRef] [PubMed] [Google Scholar]
- Electrosurgical treatment of etretinate-resistant Darier's disease. J Dermatol Surg Oncol. 1989;15:1277-80.
- [CrossRef] [PubMed] [Google Scholar]
- The surgical treatment of hypertrophic Darier's disease. J Dermatol Surg Oncol. 1985;11:420-3.
- [CrossRef] [PubMed] [Google Scholar]
- Combined retinoid plus surgical treatment of hypertrophic Darier's disease. J Europ Acad Dermatol Venereol. 2006;2:242-4.
- [CrossRef] [Google Scholar]
- The surgical treatment of hypertrophic intertriginous Darier's disease. J Plast Reconstr Aesthet Surg. 2009;62:e442-6.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical excision for non-familial hypertrophic Darier's disease. ANZ J Surg. 2018;88:E77-8.
- [CrossRef] [PubMed] [Google Scholar]
- Darier disease: Sustained improvement following reduction mammaplasty. Cutis. 2003;72:124-6.
- [Google Scholar]
- Darier's disease, an unusual problem and solution. J Hand Surg Br. 2004;29:293-5.
- [CrossRef] [PubMed] [Google Scholar]
- An effective surgical treatment for nail thickening in Darier's disease. J Eur Acad Dermatol Venereol. 2005;19:689-91.
- [CrossRef] [PubMed] [Google Scholar]
- Letter: Botulinum toxin type A: An alternative symptomatic management of Darier's disease. Dermatol Surg. 2007;33:882-3.
- [CrossRef] [PubMed] [Google Scholar]
- Botulinum toxin type A for the preventive treatment of intertrigo in a patient with Darier's disease and inguinal hyperhidrosis. Dermatol Surg. 2008;34:1733-7.
- [CrossRef] [PubMed] [Google Scholar]
- Vegetating darier disease treated with botulinum toxin. JAMA Dermatol. 2018;154:106-8.
- [CrossRef] [PubMed] [Google Scholar]
- Carbon dioxide laser ablation and adjunctive destruction for Darier-White disease (keratosis follicularis) Dermatol Surg. 2008;34:1431-4.
- [CrossRef] [PubMed] [Google Scholar]
- Condyloma-like Darier's disease of the inguinal region: Resolution after surgical excision and CO2 laser ablation. J Dtsch Dermatol Ges. 2015;13:1180-4.
- [CrossRef] [PubMed] [Google Scholar]
- Carbon dioxide laser vaporization of recalcitrant symptomatic plaques of Hailey-Hailey disease and Darier's disease. J Am Acad Dermatol. 1990;23:893-7.
- [CrossRef] [Google Scholar]
- Darier-White disease treated with fractional CO2 laser in two cases. Dermatol Ther. 2015;28:254-7.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of segmental keratosis follicularis (Darier disease) using ablative fractional laser resurfacing. Dermatol Surg. 2015;41:516-8.
- [CrossRef] [PubMed] [Google Scholar]
- Extensive recalcitrant Darier disease successfully treated with laser ablation. Br J Dermatol. 2010;162:227-9.
- [CrossRef] [PubMed] [Google Scholar]
- Significant alleviation of Darier's disease with fractional CO2 laser. J Cosmet Laser Ther. 2015;17:77-9.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of erbium: YAG laser ablation in Darier disease and Hailey-Hailey disease. Arch Dermatol. 1999;135:423-7.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of Darier's disease using a 1,550-nm erbium-doped fiber laser. Dermatol Surg. 2010;36:142-6.
- [CrossRef] [PubMed] [Google Scholar]
- Segmental Darier disease: Treatment with pulsed dye laser. Hautarzt. 2009;60:995-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dye laser treatment for darier disease: Results of a case series. Photomed Laser Surg. 2016;34:305-7.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of Darier disease with the flashlamp-pumped pulsed-dye laser. Arch Dermatol. 2008;144:1073-5.
- [CrossRef] [PubMed] [Google Scholar]
- Exacerbation, then clearance, of mutation-proven Darier's disease of the skin after radiotherapy for bronchial carcinoma: A case of radiation-induced epidermal differentiation? Radiat Res. 2001;156:724-30.
- [CrossRef] [Google Scholar]
- Efficacy of the Radiotherapy on Darier's Disease: An Indirect Evidence. Case Rep Dermatol Med. 2013;2013:1-4.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of recalcitrant Darier's disease with electron beam therapy. Dermatol Ther. 2010;23:302-4.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term improvement of recalcitrant Darier disease with photon and electron beam radiation therapy. JAAD Case Rep. 2018;4:1062-4.
- [CrossRef] [PubMed] [Google Scholar]
- Focal multimodality radiation therapy: A promising treatment for recalcitrant Darier disease. Dermatol Ther. 2018;31:e12641.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of Darier's disease with photodynamic therapy. Br J Dermatol. 2003;149:606-10.
- [CrossRef] [PubMed] [Google Scholar]
- Photodynamic therapy in a patient with Darier's disease. J Eur Acad Dermatol Venereol. 2006;20:870-2.
- [Google Scholar]
- Clinical improvement in Darier's disease with photodynamic therapy. Australas J Dermatol. 2010;51:32-5.
- [CrossRef] [PubMed] [Google Scholar]






