Translate this page into:
Melanoma arising from the epidermis overlying an acquired intradermal nevus on the forehead
Correspondence Address:
Noriaki Nakai
Department of Dermatology, Kyoto Prefectural University of Medicine, Graduate School of Medical Science, 465 Kajii-cho, Kawaramachi Hirokoji, Kamigyo-ku, Kyoto 602-8566
Japan
| How to cite this article: Nakai N, Katoh N. Melanoma arising from the epidermis overlying an acquired intradermal nevus on the forehead. Indian J Dermatol Venereol Leprol 2015;81:533-535 |
Sir,
Melanomas can arise from pre-existing nevi or occur de novo. [1] Giant congenital nevi and multiple dysplastic nevi are known risk factors for progression of nevi into melanomas. However, melanoma arising in association with acquired melanocytic nevi has rarely been reported. [2],[3] Herein, we report a case of melanoma arising in association with an acquired intradermal nevus.
A 49-year-old Japanese female visited our department for diagnosis of a black macule. She had noticed gradual development of variegated coloring and asymmetry for 2 years in a lesion which had been on her left forehead for over 10 years. At her first visit, a brownish black 9 × 7 mm macule with a central 3 mm brown nodule was seen on the left forehead [Figure - 1]. Dermoscopic findings of the small nodule showed a perifollicular globular brown pigmentation. The surrounding macule showed a central blue-white veil, atypical pigment network and dots and globules of various sizes and shapes [Figure - 2]. Because the lesion was thought to be a possible melanoma, an excisional biopsy with 2 mm margin was performed for diagnosis. The histopathology of the small nodule showed nests of melanocytes in the epidermal basal layer and round-to-cuboidal cells in the dermis, and maturation of round-to-cuboidal cells in the deeper dermis [Figure - 3]a and b. The histopathology of the macule showed proliferation of spindle-shaped atypical melanocytes with abundant melanin granules in the epidermal basal layer and superficial and mid-dermis [Figure - 3]a and c. The melanocytes, atypical melanocytes and round-to-cuboidal cells were positive for S100 [Figure - 3]d and Melan-A. The melanocytes and atypical melanocytes were positive for HMB-45 [Figure - 3]e and f but the round-to-cuboidal cells were negative [Figure - 3]e and g. We diagnosed this case as melanoma arising in association with an acquired intradermal nevus. The tumor thickness was 1.8 mm. Laboratory tests were within normal limits. Positron emission tomography and computed tomography showed no distant metastasis. Left cervical sentinel lymph node biopsy and wide excision with margins of 5 mm around the remaining scar were performed. The excised tissues did not contain tumor cells. She was classified as stage IB (pT2aN0M0) according to the AJCC/UICC melanoma classification.
 |
| Figure 1: A small brown nodule measuring 3 mm surrounded by a brown-to-black macule measuring 9 × 7 mm on the left forehead |
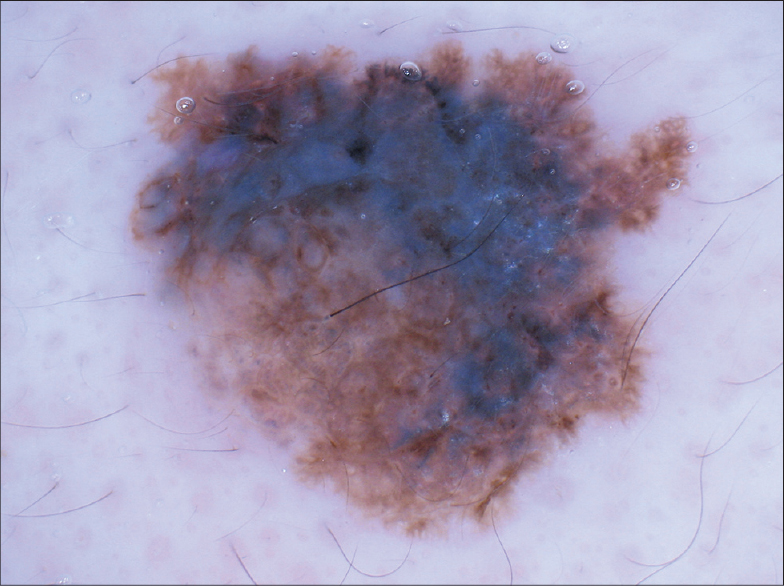 |
| Figure 2: Dermoscopy of the small nodule showed perifollicular globular brown pigmentation. The surrounding macule showed a central blue-white veil, atypical pigment network and dots and globules varying in size and shape |
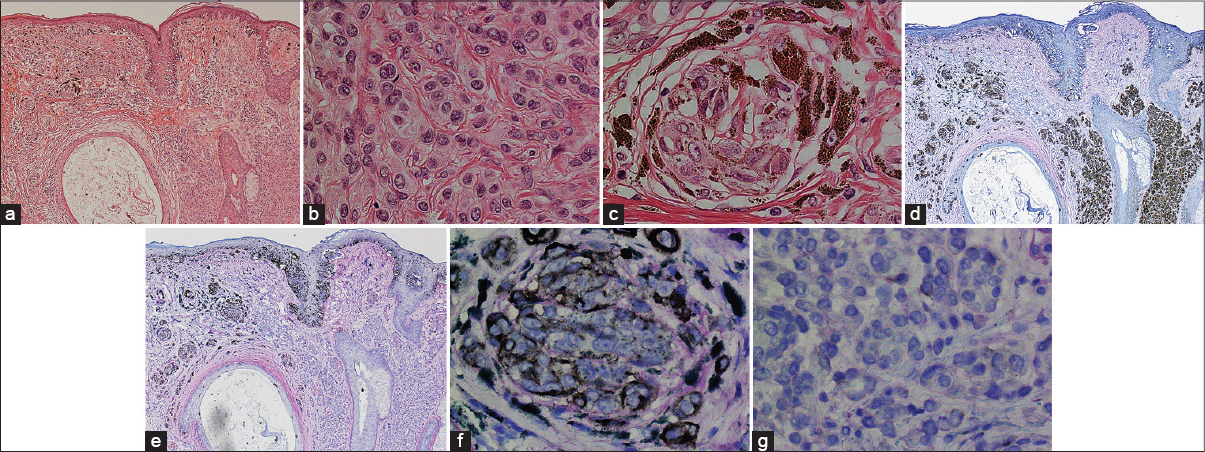 |
| Figure 3: (a) The histopathology of the small nodule showed nests of melanocytes in the epidermal basal layer and round-to-cuboidal cells with maturation in the dermis. The histopathology of the macule showed proliferation of spindle-shaped atypical melanocytes in the epidermal basal layer and superficial and middle dermis (left side, melanoma; right side, nevus; hematoxylin– eosin (H and E) staining, original magnification ×40). (b) Higher magnification of the round-to-cuboidal cells (H and E staining, original magnification ×400). (c) Higher magnification of the atypical melanocytes (H and E staining, original magnification ×400). (d) The melanocytes, atypical melanocytes and round-to-cuboidal cells were positive for S100 (left side, melanoma; right side, nevus; original magnification ×40). (e) The melanocytes and atypical melanocytes were positive for HMB-45, but the round-to-cuboidal cells were negative for HMB-45 (left side, melanoma; right side, nevus; original magnification ×40). (f) Higher magnification of the atypical melanocytes (HMB-45 staining, original magnification ×400). (g) Higher magnification of the round-to-cuboidal cells (HMB-45 staining, original magnification ×400) |
In a study of 1606 patients with cutaneous melanoma, 421 (26.2%) melanomas were histologically associated with nevi, amongst which 240 (57.0%) melanomas were associated with nondysplastic nevi. [1] Betti et al. also reported that 247 (28.2%) of 873 cutaneous melanomas were associated with melanocytic nevi. [4] However, there were no reports of the frequency of melanoma associated with only common acquired melanocytic nevus. Giant congenital melanocytic nevus and dysplastic nevus are variants of melanocytic nevus and they are known risk factors for the development of melanoma. [1],[5] Therefore, melanoma arising from an acquired intradermal nevus, as seen in the present case, was considered rare.
In the present case, dermo-epidermal junctional nests of atypical melanocytes were seen, and the intradermal nevus and nests of atypical melanocytes were clearly separated. A dermoscopic examination of the periphery of the intradermal nevus also showed a blue-white veil, as well as dots and globules varying in size and shape. Based on these findings, we surmised that the melanoma might have arisen from the epithelium overlying the intradermal nevus and extended through the epidermis and into the dermis.
| 1. |
Bevona C, Goggins W, Quinn T, Fullerton J, Tsao H. Cutaneous melanomas associated with nevi. Arch Dermatol 2003;139:1620-4.
[Google Scholar]
|
| 2. |
Okun MR, Di Mattia A, Thompson J, Pearson SH. Malignant melanoma developing from intradermal nevi. Arch Dermatol 1974;110:599-601.
[Google Scholar]
|
| 3. |
Benisch B, Peison B, Kannerstein M, Spivack J. Malignant melanoma originating from intradermal nevi. A clinicopathologic entity. Arch Dermatol 1980;116:696-8.
[Google Scholar]
|
| 4. |
Betti R, Santambrogio R, Cerri A, Vergani R, Moneghini L, Menni S. Observational study on the mitotic rate and other prognostic factors in cutaneous primary melanoma arising from naevi and from melanoma de novo. J Eur Acad Dermatol Venereol 2014;28:1738-41.
[Google Scholar]
|
| 5. |
Watt AJ, Kotsis SV, Chung KC. Risk of melanoma arising in large congenital melanocytic nevi: A systematic review. Plast Reconstr Surg 2004;113:1968-74.
[Google Scholar]
|
Fulltext Views
3,915
PDF downloads
1,353





