Translate this page into:
Mercury-induced cutaneous poisoning with generalised erythema and pruritic blister
Corresponding author: Prof. Gang Wang, Department of Dermatology, Xijing Hospital, Fourth Military Medical University, Shaanxi, China. wanggangxjyy@163.com
-
Received: ,
Accepted: ,
How to cite this article: Sun Z, Shao S, Wang G. Mercury-induced cutaneous poisoning with generalised erythema and pruritic blister. Indian J Dermatol Venereol Leprol 2022;88:831-3.
Sir,
A 73-year-old woman presented with a three-month history of generalised erythema and scattered blisters. These were accompanied by pruritus, oral ulcers, vulval mucosal erosions, swelling of lower limbs, loss of appetite, insomnia and apathy. Three months ago, she was diagnosed with toxic epidermal necrolysis in another hospital and treated with 40 mg of methylprednisolone per day for two weeks. There was partial improvement followed by a rapid flare after withdrawing methylprednisolone. On further questioning, the patient reported that she had been taking compounded pills from a local clinic for chronic urticaria since four months.
Physical examination revealed erythema and pigmentation in a livedoid pattern on the torso, arms and legs [Figure 1a], with clear, flaccid blisters on the chest and abdomen [Figure 1b]. Nikolsky sign was negative. There were erosions on the lips, gingivae and vulva [Figures 1c and d] with swelling of the lower limbs. A skin biopsy demonstrated lichenoid tissue reaction with a subepidermal blister accompanied by a mixed-cell infiltrate in the superficial dermis [Figures 2a and b]. Direct immunofluorescence showed a granular deposit of IgG, IgA and C3 at the dermo-epidermal junction [Figure 3] and indirect immunofluorescence to BP180, BP230, DSG1 and DSG3 was negative. Anti-nuclear antibody was positive (1:320) while other autoimmune antibodies were all negative. Results of other routine laboratory investigations were unremarkable.

- Erythema and brown pigmentation over the torso, arms and legs

- Bullae on the trunk
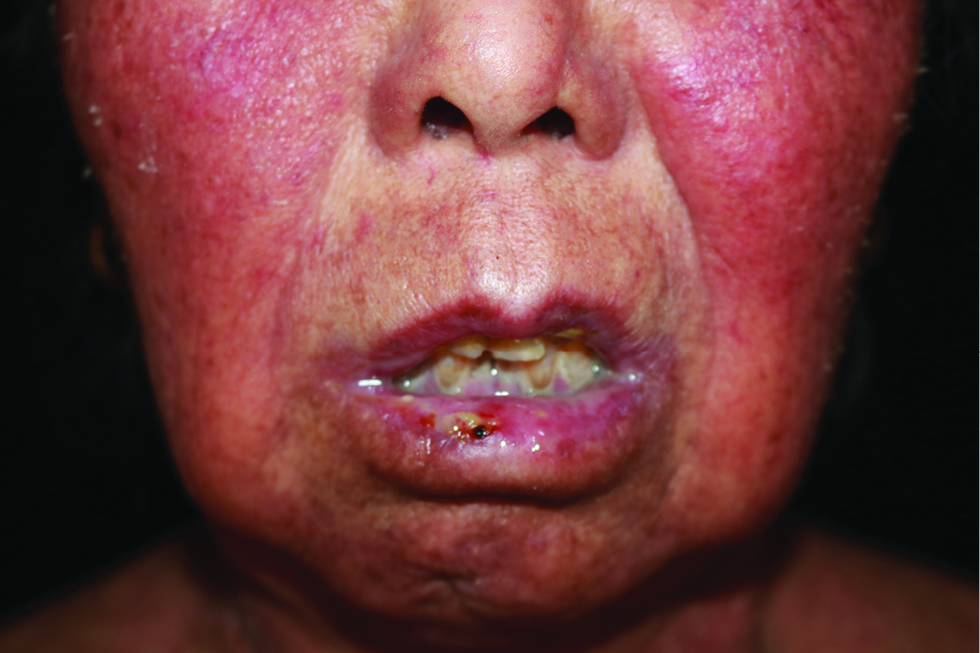
- Erosion and crust on the oral mucosa

- Erosion and crust in vulva
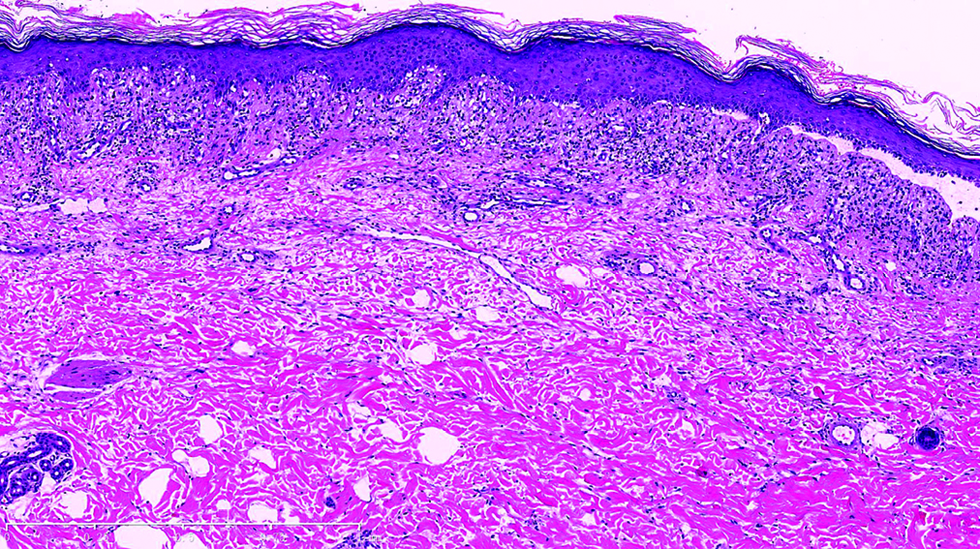
- Under low power view, lichenoid tissue reaction, subepidermal blister and a mixed dermal superficial infiltration was noted
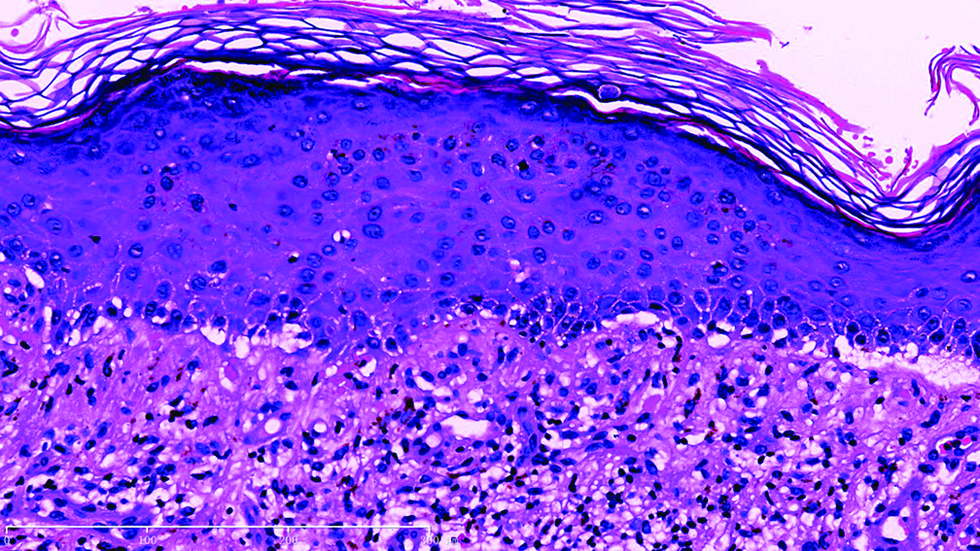
- Under high power view, liquefaction degeneration in basal membrane with a predominant lymphoid infiltration was obeserved in the epidermal-dermal junction and superficial dermis
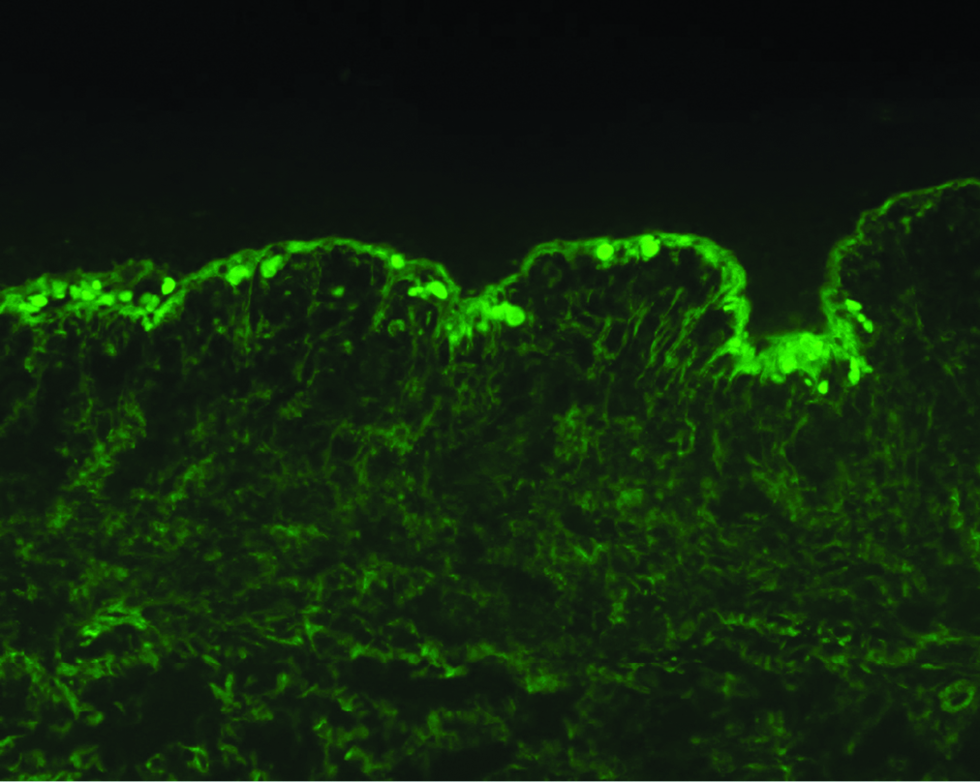
- Direct immunofluorescence analysis of lesional skin showing strong granular deposition of IgG antibodies at the dermal-epidermal junction
Patient showed poor response to oral methylprednisolone administered with a diagnosis of suspected lichenoid eruption. The real etiology remained hidden until we found occasional mercury beads within her homemade pill [Figure 4]. Urine mercury concentration was 62 μg/L (normal range <10 μg/L) which confirmed mercury toxicity. Methylprednisolone was discontinued and patient was administered 3 intramuscular injections of 2,3-dimercaptopropane sulfonate (5 mg/kg) to chelate the mercury.1 She was told to stop taking the homemade pills which led to normalization of the concentration of mercury in urine. At the two-month follow-up, the bullae and ulcers had nearly resolved with post-inflammatory hyperpigmentation.

- Indigenous prescription pills with mercury beads
Mercury poisoning, can present with multi-organ systemic involvement such as neural, renal, gastrointestinal and skin. Mercury in all forms is toxic to the body and clinical manifestations may vary depending on the type of mercury, mode of administration, dose, and duration.2 Nowadays, it is uncommon to see patients having exposure to mercury, however, some prescriptions from indigenous systems of medicine may contain mercury in compounded pills to utilize its historical role in treating many cutaneous diseases such as syphilis, psoriasis, urticaria, and melasma.3,4 Due to its uncommon presentation in the current era mercury poisoning may be often misdiagnosed, leading to delayed treatment and significant morbidity.
The differential diagnosis for this case included bullous pemphigoid,5 bullous drug eruption, bullous lupus erythematosus, paraneoplastic pemphigus, and other immunobullous diseases. Negative BP180 and BP230 antibodies, and a granular deposit of IgG, IgA and C3 in dermal-epidermal junction did not meet the diagnostic criteria of bullous pemphigoid. We speculated that a granular deposit of IgG, IgA, C3 and ANA might be caused by mercury-induced immunoreaction. No necrotic keratinocytes were found on histology which is inconsistent with toxic epidermal necrosis. Bullous fixed drug eruption was not supported by the clinical picture. Although ANA showed positivity, other autoimmune antibodies of the ANA profile were all negative, making a diagnosis of bullous lupus erythematosus unlikely. Considering that the patient also had depression and irritability, we suspected heavy metal poisoning caused by homemade pills.Blood or urine testing of increased mercury concentrations establishes the diagnosis of mercury poisoning. The psychiatric symptoms and allotriogeustia may help with the diagnosis, as mercury poisoning also causes neuropsychiatric clinical manifestations. Therefore, a thorough enquiry about medication history or food intake and careful clinical observation are of great importance in making a diagnosis of mercury toxicity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- The toxicology of mercury–“Current exposures and clinical manifestations. New Engl J Med. 2003;349:1731-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous mercury granuloma following accidental occupational exposure. Indian J Dermatol Venereol Leprol. 2015;81:57-9.
- [CrossRef] [PubMed] [Google Scholar]
- History of the treatment of psoriasis. J Am Acad Dermatol. 1992;27:640-5.
- [CrossRef] [PubMed] [Google Scholar]
- Mercury toxicity and treatment: A review of the literature. J Environ Public Health. 2012;2012:460508.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of blood and urinary mercury in pemphigus vulgaris and pemphigus foliaceus patients and its comparison with control group. Indian J Dermatol Venereol Leprol. 2015;81:225.
- [CrossRef] [PubMed] [Google Scholar]





