Translate this page into:
Microinvasive squamous cell carcinoma arising in discoid lupus erythematosus lesions successfully treated with imiquimod 5% cream
2 Department of Otorhinolaryngology, Celal Bayar University, Faculty of Medicine, Manisa, Turkey
3 Department of Pathology, Celal Bayar University, Faculty of Medicine, Manisa, Turkey
Correspondence Address:
Aylin Turel Ermertcan
Department of Dermatology, Celal Bayar �niversitesi Tip Fak�ltesi, Dermatoloji Anabilim Dali, 45010 Manisa
Turkey
| How to cite this article: Ermertcan AT, Gencoglan G, Eskiizmir G, Temiz P. Microinvasive squamous cell carcinoma arising in discoid lupus erythematosus lesions successfully treated with imiquimod 5% cream. Indian J Dermatol Venereol Leprol 2013;79:115-117 |
Sir,
Discoid lupus erythematosus (DLE) is the most common form of cutaneous lupus erythematosus. It is well known that squamous cell carcinoma may develop on long-standing discoid lupus erythematosus lesions. [1]
Alternative therapies, such as photodynamic therapy, interferon, retinoids, 5-fluorouracil and imiquimod can be used effectively either as monotherapies or as adjuvants to the surgical modalities for the treatment of nonmelanoma skin cancers. [2]
A-46-year old white female patient presented with nonhealing wounds on her lip and around ears with a history of nine months. The lesion on the left preauricular region had been excised three months ago and was diagnosed as microinvasive squamous cell carcinoma (SCC) histopathologically. Recurrence occurred in the same region immediately just one month later. The lesion on the lip had enlarged progressively.
Dermatological examination revealed erythematous, scaly infiltrated plaques on the left preauricular region, right infraauricular region and right lower lip with the sizes of 2 × 1.5 cm, 1 × 1 cm and 2.5 × 1.5 cm, respectively [Figure - 1]. Two punch biopsies were performed from the recurred lesion on the left preauricular region and from the lesion on the right infraauricular region of the patient. On histopathological examination, epidermal basal vacuolization, plugged follicles, perifollicular inflammation, solar elastosis and invasive squamous cell islands were observed [Figure - 2]. With clinical and histopathological findings, the patient was diagnosed as microinvasive SCC arising in DLE. Physical and laboratory examinations revealed no signs of systemic involvement for both SCC and systemic lupus erythematosus (SLE). We did not detect any lymphatic involvement on the examination of regional lymph nodes. Autoimmunity markers for SLE were found to be negative.
 |
| Figure 1: (a-c) Erythematous, scaly infiltrated plaques on the locations of left preauricular region, right infraauricular region and right lower lip, respectively (before treatment) |
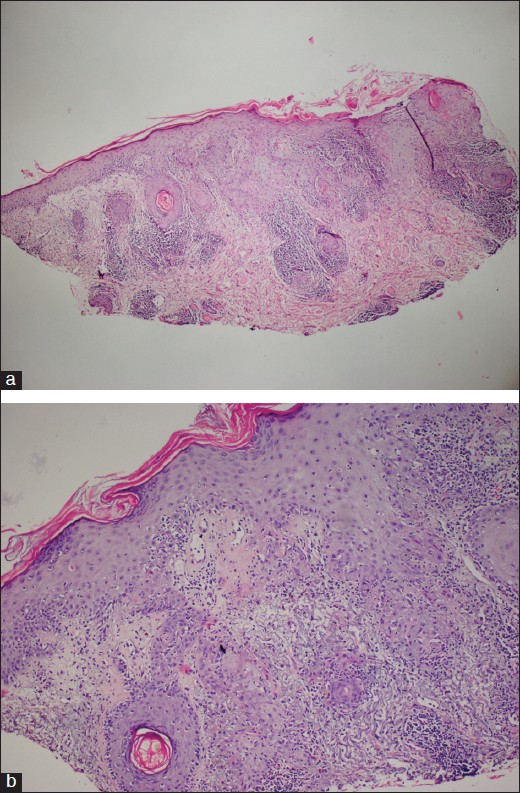 |
| Figure 2: (a) Plugged follicles, perifollicular inflammation, solar elastosis and invasive squamous cell islands in dermis (Hematoxylin-eosin, × 40). (b) Epidermal basal vacuolization, perifollicular inflammation and invasive squamous cell islands (Hematoxylin-eosin, × 100) |
Since the patient′s lesions were multiple and recurrence of the lesion on the left preauricular region was observed after excision, we selected imiquimod 5% cream as the treatment agent. Complete healing was observed within two weeks′ topical imiquimod therapy that was applied five days per week [Figure - 3]. We did not observe any side effects except minimal burning and irritation due to imiquimod. We prescribed an appropriate sunscreen and gave advices about sun protection behaviors to the patient. There was no recurrence or new lesion development during one year′s-follow up.
 |
| Figure 3: (a-c) Clinical appearance of the patient after topical imiquimod therapy |
DLE is a disease characterized by well-defined, erythematous, scaly patches, which tend to heal with atrophy and scarring. The lesions are commonly seen in sun-exposed areas, especially on the face. [3]
SCC is a rare, but well-recognized, long-term complication of chronic DLE. Duration between the initiation of DLE lesion and appearance of SCC may vary in a wide range, from 1 to 41 years. [1] This time was very short, approximately six months, in our patient.
The exact etiology of the development of SCC in chronic DLE has not been clearly elucidated. The reason why only very small minorities of patients with DLE develop SCC is also unknown. Ultraviolet light exposure probably plays a significant role, compounded by the decrease in protective melanin in chronic DLE with hypopigmentation as well as in fair-skinned individuals. Genetic predisposition, severity of DLE and human papillomavirus infection of discoid lesions may be other possible factors for the development of SCC. [4] Our patient had fair skin and she had no other confounding factor.
Treatment of DLE presents a challenge to clinicians because lesions usually show recurrence after treatment. Antimalarials, corticosteroids (topical, intralesional, and/or systemic), dapsone, retinoids, methotrexate and azathioprine are treatment options for DLE. Topical tacrolimus, thalidomide, clofazimine, cryotherapy and laser are the other reported therapeutic choices. [5] We found only two cases of DLE succesfully treated with topical imiquimod in the literature. [3],[5] Gül et al reported a 44-year-old male patient with the diagnosis of generalized DLE. They applied imiquimod cream 5% to his lesions once a day three times a week and they observed regression of the lesions after 20 applications. [5] Gerdsen et al presented a 56-year-old female patient with DLE of the scalp. Their patient was unresponsive to topical steroids, hydroxychloroquine, methotrexate, azathioprine, mycophenolate mofetil and dapsone. They applied imiquimod 5% cream topically once daily in two cycles over three weeks. They observed a marked improvement on the follow-ups and no recurrence was defined after a period of more than one year. [3]
Imiquimod, a heterocyclic imidazoquinoline amide, is an immune response modifying drug that has potent antiviral and antitumor activity. [6] It has been used effectively in the treatment of nonmelanoma skin cancers. [2] Because of its ability to rapidly and potently stimulate both innate and adaptive arms of the immune system, imiquimod has been demonstrated to be useful in the treatment of a number of conditions beyond the FDA-approved indications. DLE has been reported as one of the off-label indications of imiquimod. [6]
In the literature search, we observed that SCC that developed on DLE lesions was mostly treated by surgical excision. However, our patient had multiple lesions and the lesion on the left preauricular region had recurred after excision. Therefore, also taking better cosmetic results into account, we preferred imiquimod 5% cream as an alternative treatment
To our knowledge this is the first case reporting the efficacy of topical imiquimod in the treatment of SCC that arised on DLE lesions.
| 1. |
Dhingra M, Bhalla M, Thami GP, Mittal P. Metastasizing squamous cell carcinoma arising from chronic discoid lupus erythematosus plaque of recent oncet. Indian J Dermatol Venereol Leprol 2011;77:626.
[Google Scholar]
|
| 2. |
Terushkin V, Braga JC, Dusza SW, Scope A, Busam K, Marghoob AA, et al. Agreement on the clinical diagnosis and management of cutaneous squamous neoplasms. Dermatol Surg 2010;36:1514-20.
[Google Scholar]
|
| 3. |
Gerdsen R, Wenzel J, Uerlich M, Bieber T, Petrow W. Successful treatment of chronic discoid lupus erythematosus of the scalp with imiquimod. Dermatology 2002;205:416-8.
[Google Scholar]
|
| 4. |
Ee HL, Ng PPL, Tan SH, Goh CL. Squamous cell carcinoma developing in two Chinese patients with chronic discoid lupus erythematosus: The need for continued surveillance. Clin Exp Dermatol 2006;31:542-4.
[Google Scholar]
|
| 5. |
Gül U, Gönül M, Cakmak SK, Kiliç A, Demiriz M. A case of generalized discoid lupus erythematosus: Successful treatment with imiquimod cream 5%. Adv Ther 2006;23:787-92.
[Google Scholar]
|
| 6. |
Ganjian S, Ourian AJ, Shamtoub G, Wu JJ, Murase JE. Off-label indications for imiquimod. Dermatol Online J 2009;15:4.
[Google Scholar]
|
Fulltext Views
2,765
PDF downloads
1,602





