Translate this page into:
Miliary pulmonary tuberculosis with tuberculosis verrucosa cutis
2 Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, Puducherry UT, India
Correspondence Address:
Saka VinodKumar
Department of Pulmonary Medicine, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, Puducherry UT
India
| How to cite this article: VinodKumar S, Mathanraj S, Kumar NN, Venugopal J, Basu D. Miliary pulmonary tuberculosis with tuberculosis verrucosa cutis. Indian J Dermatol Venereol Leprol 2014;80:266-267 |
Sir,
Tuberculosis verrucosa cutis is a form of cutaneous tuberculosis occurring in patients with well preserved cell mediated immunity. The presence of miliary tuberculosis in a patient with tuberculosis verrucosa cutis is a rare and unusual combination as they are at two ends of an immunological spectrum.
A 40-year-old male presented to our department with an ulcerated plaque over the plantar aspect of left foot for one year that was associated with swelling, pain and occasional watery discharge [Figure - 1]. He also gave history of low grade fever and cough over two months. No other significant co-morbidities or contact with tuberculosis was present. He denied any previous anti-tubercular therapy.
 |
| Figure 1: TB verrucosa cutis - lesions - pre and post treatment |
Baseline investigations (hemogram, liver and renal function tests) were found to be normal. Cultures from the wound discharge (bacterial, fungal and tubercular) were negative. Chest X-ray revealed bilateral miliary mottling [Figure - 2]. Computed tomography of the chest showed characteristic miliary nodules bilaterally. There were no lesions in the abdominal organs. Ophthalmic examination showed absence of choroid tubercles. Mantoux test was negative. Sputum smear and cultures (on Lowenstein-Jensen medium) were also negative. Flexible fibre-optic bronchoscopy showed inflamed left main stem and lingular bronchus. Acid fast bacilli (AFB) were not seen or grown from bronchial washings and mycobacteria were not detected by PCR. The patient did not consent for trans-bronchial lung biopsy. ELISA for antibodies to HIV and HBsAg (Hepatitis B surface antigen) were found to be negative.
A skin biopsy from the plantar lesion revealed granulomas in the dermis composed of epithelioid cells, Langhans giant cells and lymphocytes in the dermis with marked hyperkeratosis and parakeratosis of the overlying epidermis [Figure - 3]. Based on these findings, a diagnosis of miliary tuberculosis with tuberculosis verrucosa cutis was made. The patient was started on category I anti tubercular therapy given as follows: 2 months of HRZE (H-isoniazid; R-rifampicin; Z-pyrazinamide; E-ethambutol) and 4 months of HR in a daily regimen. At the end of treatment, the foot lesion was completely cleared [Figure - 1] and radiological resolution of miliary shadowing was observed.
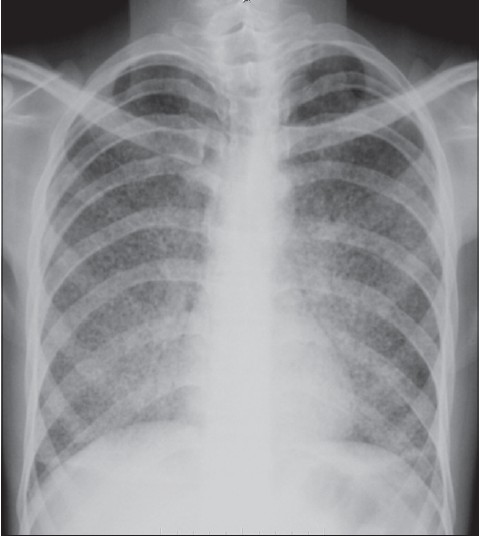 |
| Figure 2: Chest X-ray showing miliary nodules |
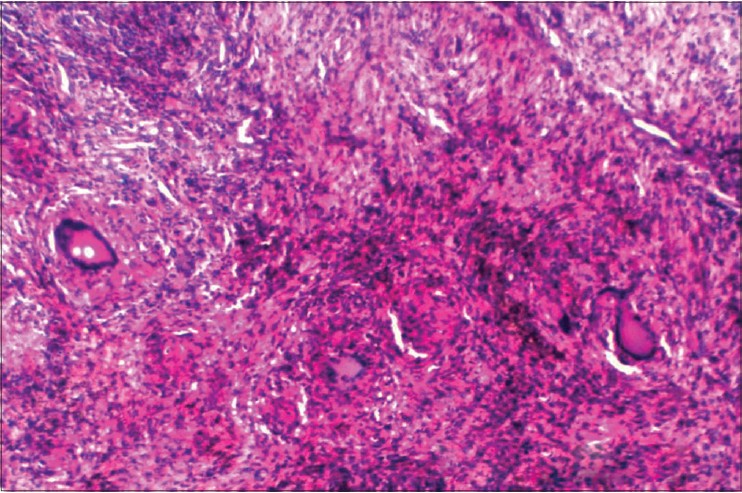 |
| Figure 3: H and E staining shows tubercular granuloma (epitheliod cells, lymphocytes and giant cells seen) |
Tuberculosis verrucsa cutis is also known as warty tuberculosis, prosector′s wart, butcher′s wart, and verrucous tuberculosis. [1] Lesions usually occur on areas exposed to trauma such as hands, fingers and lower extremities. Physicians, pathologists and medical laboratory personnel are usually affected due to handling of sputum and pathologic material. Indian reports indicate that tuberculosis verrucosa cutis occurred most commonly on the lower extremities and buttocks whereas hands were most commonly involved elsewhere. [2]
Warty tuberculosis is usually solitary but multiple lesions may occur. The lesion typically starts with a painless, dusky red, firm, indurated nodule or papule that expands peripherally and is surrounded by inflammation. Spontaneous central resolution with areas of atrophy surrounded by a verrucous keratotic surface or an annular plaque with a warty advancing border is seen. Occasionally pus and keratinous material may be expressed from fissures in the warty areas. Lymphadenopathy is usually absent and if seen, indicates secondary infection. [3]
Histopathology shows pseudoepitheliomatous hyperplasia with marked hyperkeratosis, acanthosis, dense inflammatory infiltrates with epitheliod cells and giant cells in the mid-dermis. Typical tuberculosis granulomas with characteristic caseation are not common. [3] Tuberculosis verrucosa cutis is a paucibacillary disease demonstrating very few bacilli. Mantoux reaction is markedly positive.
Diagnosis is usually confirmed by typical clinical appearance, histopathological pattern, and a positive response to anti-tubercular treatment. The differential diagnoses include blastomycosis, chromomycosis, fixed sporotrichosis, lesions caused by non-tubercular mycobacteria, lupus vulgaris, and tertiary syphilis.
Kumar et al. in their study observed that cutaneous TB was associated with tuberculosis in other organs in 22% of patients. Organs commonly affected were lungs followed by bone, abdomen and CNS. The association of tuberculosis verrucosa cutis with pulmonary tuberculosis was rare in their study. [4]
Our patient had both tuberculosis verrucosa cutis and miliary tuberculosis which is a very rare association. The presence of miliary tuberculosis in our patient was identified on routine screening for pulmonary tuberculosis. Conversely, cutaneous involvement is a very rare and unusual presentation in miliary tuberculosis. [5] Whether military tuberculosis preceded the skin lesion or followed it is difficult to determine.
Tuberculosis verrucosa cutis can result both from inoculation and from endogenous spread. [4] The foot lesion can be explained by inoculation of mycobacteria while walking barefoot. Endogenous spread as a part of hemato-lymphatic dissemination to the skin in a patient with miliary tuberculosis is a rarer possibility. Sehgal et al. [3] reported a case of disseminated tuberculosis with tuberculosis verrucosa cutis and pulmonary involvement in an immunocompetent patient, similar to our case. Padmavathy et al. also reported miliary tuberculosis in a patient with tuberculosis verrucosa cutis and explained it as part of the varied immunological response to infection. [6]
| 1. |
Pomeranz MK, Orbuch P, Shupack J, Brand R. Mycobacteria and skin. In: Rom WM, Garay S, editors. Tuberculosis. Vol. 51.1 st ed. London: Little Brown Co.;1996. p. 657-74.
[Google Scholar]
|
| 2. |
Aliaðaoðlu C, Atasoy M, Güleç AÝ,Özdemir Þ, Erdem T, Engin RÝ. Tuberculosis verrucosa cutis. Eur J Gen Med 2009;6:268-73.
[Google Scholar]
|
| 3. |
Sehgal VN, Sehgal R, Bajaj P, Sriviastava G, Bhattacharya S. Tuberculosis verrucosa cutis (TBVC). J Eur Acad Dermatol Venereol 2000;14:319-21.
[Google Scholar]
|
| 4. |
Kumar B, Muralidhar S.Cutaneous tuberculosis: A twenty-year prospective study. Int J Tuberc Lung dis 1999;3:494-500.
[Google Scholar]
|
| 5. |
del Giudice P, Bernard E, Perrin C, Bernardin G, Fouché R, Boissy C, et al. Unusual cutaneous manifestations of miliarytuberculosis. Clin Infect Dis 2000;30:201-4.
[Google Scholar]
|
| 6. |
Padmavathy L, Lakshmana Rao L, Ethirajan N, Ramakrishna Rao M, Subrahmanyan EN, Manohar U.Tuberculousverrucosa cutis (TBVC)- foot with military tuberculosis. Indian J Tuberc 2007;54:145-8.
[Google Scholar]
|
Fulltext Views
3,226
PDF downloads
1,687





