Translate this page into:
Misnomers in dermatology: Time to change and update
Correspondence Address:
Manjunath Hulmani
Department of Dermatology, Srinivasa Institute of Medical Science and Research Centre, Mukka, Mangalore - 574 146, Karnataka
India
| How to cite this article: Hulmani M, Kudur M. Misnomers in dermatology: Time to change and update. Indian J Dermatol Venereol Leprol 2013;79:479-491 |
Abstract
Most of the misnomers encountered in dermatology have arisen from lack of understanding of the underlying etiopathogenesis, histopathology and/or concepts. Some misnomers are due to imprecise translations from word of origin, etymological bungles and/or factual errors. It is very important for the residents and practitioners of dermatology to update and change the old misnomers with relevant names to avoid confusion and misunderstanding. In this article, we have listed all the misnomers in dermatology and suggested the appropriate names as indicated.Introduction
The field of dermatology is very rich in descriptive terminologies, but it is very interesting to note that there are lot of misnomers also. Sir William Osler clearly saw the importance of an exact medical lexicon when he wrote, ′′Use guidelines for naming diseases. If our knowledge does not permit to give a name according to the etiology of the disease, the rule should be to pick the one which seems least objectionable, taking priority and usage into account.′′ [1] A misnomer is defined as a word that is used incorrectly or misleadingly. [2] This description is because of frequent use of eponyms and toponyms. An eponym is a person (real or fictitious) from whom something is said to take its name. The term eponym is derived from the Greek words epi, meaning upon, and onyma, meaning name. Thus, eponym means giving a name, while toponym is the name derived from place (geographic eponym) or things. [3] We have tried to compile misnomers in dermatology and alternative terms, where possible, have been suggested.
Misnomers in Dermatological Infections
Tinea
Tinea is a superficial fungal infection of keratinised tissue by dermatophytes. The literal meaning of tinea is larva as Romans mistakenly thought the infection to be due to insects. [4]
Ringworm
The dermatophytic infection is commonly referred to as ringworm, particularly by non-dermatologist physicians and the lay public, which stems from the annular appearance of the lesions. The term is a significant misnomer as no worms are associated with this condition. [5]
Athlete′s foot
It is a misnomer as it does not refer to the physical condition of the foot specific to athletes. It is merely a popular name given to the pedal fungal infection caused by dermatophytes. [5]
Moniliasis
The term monilias is used as a synonym for candidiasis, and it is a misnomer as moniliasis refers to a stage of ascomycetes and has no relationship to the genus Candida. [5]
Tinea versicolor
The term tinea is used for dermatophytic infections. The causative organism for tinea versicolor, Malassezia furfur or M. globosa, is not a dermatophyte, so to call it as tinea versicolor is a misnomer. Pityriasis versicolor is an appropriate terminology for this condition. [5]
Chicken pox
Chicken pox, also known by its Latin name of varicella, is a misnomer. The disease was named after the French term "chichiepois" - which means "chickpea" - from a supposed similarity in size of the seed to the lesions. "Chichiepois" eventually became "chicken pox." [6]
Kaposi sarcoma
Kaposi sarcoma is an infection caused by human herpesvirus-8 (HHV 8) in immunocompromised individuals. Cells infected with HHV 8 produce cytokines, chemokines and growth factors, which cause proliferation of endothelial and spindle cells. There is controversy as to whether these proliferative cells truly represent a malignant neoplasia versus an inflammatory hyperplasia. Therefore, the term sarcoma used in the description of this condition may not be warranted. [7]
Botryomycosis
Botryomycosis is a chronic granulomatous reaction to bacterial infection. In 1884, Revolta named it botryomycosis under the impression that it was caused by a fungus. The word "botryo" is derived from the Greek term "Botrys," meaning "a bunch of grapes." The word mycosis is a misnomer as it is caused by true bacteria and not by fungus. It is also known as actinophytosis, bacterial pseudomycosis and granular bacteriosis. [8]
Malignant pustule of anthrax
Although the primary lesion of anthrax has been called a malignant pustule, the term is a misnomer. The lesion is neither malignant nor purulent, and pustules, if present, represent secondary infection due to streptococci or staphylococci. [5]
Pemphigus neonatorum
It is severe bullous impetigo of the newborn and has nothing to do with pemphigus. [9]
Trichomycosis
It is characterized by concretions along the hair shafts [Figure - 1] that contain the bacterial colonies of Corynebacterium tenuis, easily recognized in gram-stained preparations. [10] The term "trichomycosis" is a misnomer and may now better be called as trichobacteriosis. [11]
 |
| Figure 1: Trichomycosis axilaris, yellow-colored concretions along the hair shaft |
Rocky mountain spotted fever (RMSF)
The term is a misnomer as the condition is relatively rare in the Rocky Mountain States. First noted in the mountains of Montana, RMSF is found most commonly in the Southeast and Central regions of the United States. The greatest numbers of incident cases are reported in North Carolina, Oklahoma, Arkansas, Missouri, Montana, South Dakota and Wyoming. [12]
Pubic lice
Crab lice or Phthirus pubis is also known as pubic lice, which is a misnomer. While the organism is typically found in the pubic area, it may affect any part of the body with secondary hair, including the eyelashes and eyebrows of children. [5]
Misnomers in Tumors and Cysts
Sebaceous cyst
Sebaceous cyst is a misnomer for epidermal or epidermoid cysts. These keratin-containing cysts lined by epidermis are not of sebaceous origin. [13]
Nevus comedonicus
It is a benign hamartoma of the pilosebaceous unit, and is a misnomer as typical comedones are not present. The term follicular keratotic nevus has been proposed. [14]
Seborrheic keratosis
Seborrheic keratoses result from a proliferation of keratinocytes and are not related to sebaceous glands. Therefore, these keratoses should not be termed seborrheic. [15]
Leser-Trelat sign
The eponym has been wrongly credited to two European surgeons, Edmund Leser and Ulysse Trelat. While they apparently observed cherry angiomatosis in patients with cancer, it was Hollander who first linked internal cancer with seborrheic-keratoses [Figure - 2] in 1900. [5],[16]
 |
| Figure 2: Leser Trelat sign, eruption of seborrheic keratosis over the back |
Eruptive syringoma
Eruptive syringoma may represent a hyperplastic response of the eccrine duct to an inflammatory reaction rather than a true adnexal neoplasm. The term "syringomatous dermatitis" has been proposed for such cases. [17]
Trichoadenoma (trichoadenoma of Nikolowski)
The term trichoadenoma is a misnomer as there are no adenomas of strictly follicular lineage; the hair follicle is not a structure that exhibits glandular differentiation. [18]
Adult colloid milium
These are asymptomatic, shiny, smooth, firm papules 1-10 mm in diameter, involving chronically sun-damaged skin of adults. Microscopically, the papules show severe elastosis involving most of the papillary dermis. This is a distinct clinical form of severe solar elastosis, and the term papular-elastosis has been suggested. [19]
Myxoid cyst
Digital myxoid cysts occur over the distal phalanx of the finger [Figure - 3] or rarely the toe, appearing as solitary, shiny, tense, opalescent papules. There are currently two variations of these cysts. The first arises in the proximal nail fold and is a form of focal mucinosis. The other arises in proximity to the distal interphalangeal joint as a result of an extension of the joint lining due to osteoarthritis and thus resembles a ganglion cyst. Many of the former types of cyst do not exhibit a lining histologically and, therefore, may be more appropriately termed pseudocysts. [20]
 |
| Figure 3: Myxoid cyst over the distal phalanx |
Infantile myofibromatosis
Despite being considered a rare condition, infantile myofibromatosis is the most common fibrous tumor in infancy. The solitary form (myofibromas) may affect the skin, subcutaneous cellular tissue, muscle or bone. In the multi-centered form (myofibromatosis), there may also be visceral lesions. [21] The name infantile myofibromatosis is a misnomer because the most common form of this disorder is solitary, not multicentric as the name implies. [20]
Palisaded encapsulated neuromas
These are small, solitary, asymptomatic papules occurring predominantly on the face in middle age, and are characterised histologically by proliferation of Schwann cells and axons in the dermis. The term is a misnomer as no real palisading nor encapsulation are observed. Renaming the lesion "solitary circumscribed neuroma" has been proposed. [22]
Actinic keratosis (AK)
The term AK is a misnomer as it fails to reflect the malignant nature of this lesion. From the cytological and from the molecular biological point of view, AKs demonstrate features of malignancy from their inception. Both AK and invasive squamous cell carcinoma (SCC) contain atypical keratinocytes with loss of polarity, nuclear pleomorphism, disordered maturation and increased number of mitotic figures. [23] Unfortunately, this questionable misnomer "actinic keratosis" has become ingrained in our medical literature and, till now, attempts to rename this lesion to accurately reflect its biologic behavior have failed. But, regardless of what it is called, AK (actinic keratosis) must be clearly recognized as what it is - incipient SCC. [24]
Fibroepithelioma of Pinkus (FEP)
FEP was first described as pre-malignant fibroepithelial tumor of the skin by Herman Pinkus in 1953. [25] Although FEP is currently accepted as a variant of basal cell carcinoma (BCC), its classification still remains controversial. FEP may also be categorized as a variant of trichoblastoma, a benign counterpart of BCC. [26] Therefore, fibroepithelioma is not an accurate term for this disease.
Mycosis fungoides
The term came into use in 1806 by Jean Louis Marc Alibert, a French dermatologist, when he described a severe disorder in which large necrotic tumors resembling mushrooms presented on a patient′s skin. The term is a misnomer; the condition is a cutaneous T-cell lymphoma and there is no association with fungus. [5]
Subungual melanoma
Subungual melanoma is a variant of acral lentiginous melanoma. The term is a misnomer as it is often loosely used to connote true subungual melanomas, ungual melanomas and periungual melanomas. A more accurate nomenclature, melanoma of the nail apparatus, should be used. [27]
Acne and Acneiform Eruptions
Nodulocystic or cystic acne
Historically, the term nodulocystic or cystic acne [Figure - 4] has been extensively used, and yet is a misnomer. Not lined by an epithelium, "acne cysts" are not true cysts, and are more appropriately described as nodules or pseudocysts. [5]
 |
| Figure 4: Nodulocystic acne |
Hidradenitis suppurativa (synonyms: Verneuil disease, acne inversa)
The French physician, Verneuil, in 1854 related the inflammation to the sweat glands and, in 1865, coined the term "hidrosadénitephlegmoneuse," the French term for hidradenitis suppurativa. Without performing histological studies, Verneuil viewed the entity he reported as a disorder of the sweat glands based merely on the characteristic distribution of the apocrine glands and the anatomical coincidence with the disease process. [28] The central pathogenetic event is not a suppurative inflammation of the apocrine glands but an occlusion of the hair follicles. It is acne inversa because, in contrast to acne vulgaris, the disease involves ectopic (intertriginous) locations and not the regions classically affected by acne vulgaris. Therefore, the term "hidradenitis suppurativa" should be abandoned for acne inversa. [29]
Acne keloidalis
Acne keloidalis, also known as folliculitis nuchae, is a form of chronic scarring folliculitis characterized by fibrotic papules and nodules of the nape of the neck and the occiput. The term acne keloidalis given by Bazin in 1872 is a misnomer as it differs pathogenically from acne vulgaris and true keloids are not formed. [30],[31]
Chloracne
The chloracne lesions are not "acne" because there is no sebaceous gland hypertrophy, but, rather, the disappearance of sebaceous glands and presence of epidermal cysts. It has been proposed to call these dioxin-induced cysts as "Metabolizing Acquired Dioxin-Induced Skin Hamartomas" (MADISH). [32]
Acne rosacea
The term "acne rosacea" appeared in Bateman′s writings, who made it a clinical form of acne. This confusion lasted throughout the 19th century. It was not until Hebra in Austria and Darier in France that the differential diagnosis was clearly made between acne and rosacea. The term rosacea designates facial telangiectasia, whether or not it is associated with characteristic redness. [33]
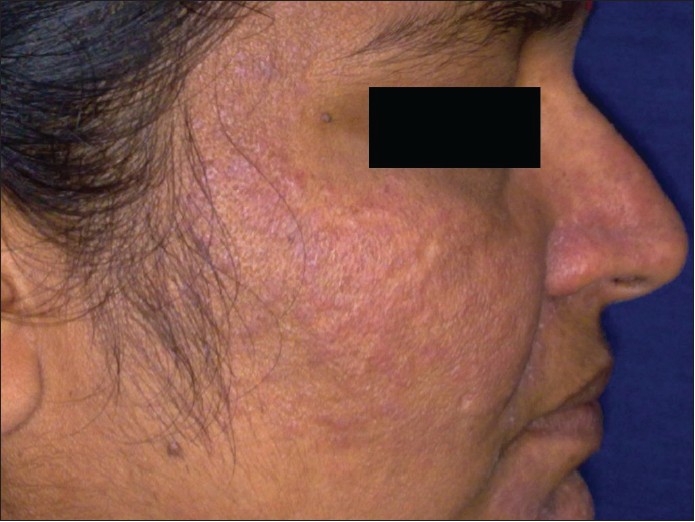
Lupus miliaris disseminatus faciei (LMDF)
LMDF is not a tuberculid because mycobacteria cannot be grown from the lesions, tuberculin test is negative and it does not respond to antitubercular treatment. [34] LMDF is an entity distinct from either skin tuberculosis or granulomatous-type rosacea. However, its name is confusing, and the name "Facial Idiopathic Granulomas with Regressive Evolution ( Figure)" has been proposed. [35]
LMDF is also called acne agminata or acnitis, which is again a misnomer as the condition is not related to acne. [36]
Hair Disorders
Hot comb alopecia
Hot comb alopecia is a term used to denote a distinctive form of scarring alopecia primarily seen in black women. The name is thought to be misleading as hot comb use was found to be an unlikely cause of alopecia in many reported cases. The term follicular degeneration syndrome is proposed for this scarring alopecia. It remains unclear whether the use of any of a variety of hair care products and techniques plays a role in the pathogenesis of this condition. [37]
Congenital triangular alopecia
Congenital triangular alopecia, also called temporal triangular alopecia, appear to develop during the first few years of life, and the designation "congenital" is a misnomer. The appearance of alopecia can be best explained as a focal zone of hair miniaturization leading to vellus hair formation. [38]
Kinky hair disease
The kinky, rather unruly hair of pili torti, a physical sign only, may exist alone in classic or late-onset pili torti, or it may occur with other signs, and point to a variety of conditions, Menkes syndrome being one of them. Others are Bjornstad syndrome, pseudomonilethrix, Bazex syndrome, Crandall syndrome, hypohydrotic ectodermal dysplasia and trichothiodystrophy. [39] Therefore, to call Menkes syndrome as Kinky hair disease is a misnomer.
Pilonidal sinus
Hodge in 1880 coined the name "pilonidal" from the Latin words pilus, which means hair, and nidus, which means nest. [40] Pilonidal disease consists of a spectrum of entities ranging from asymptomatic hair containing cysts and sinuses to a large abscess. However, the name is a misnomer because not all pilonidal cysts involve hair. Usually found in the sacrococcygeal region. However, they may also occasionally occur in the axilla, groin, interdigital web, umbilicus, nose, intermammary areas, suprapubic area, clitoris, prepuce, penis, occiput or on the feet. [41]
Genodermatoses
Phakomatosis
The term phakomatosis is derived from the Greek phakos, meaning "lentil" or "lens-shaped," and it refers to patchy, circumscribed dermatologic lesions that are the hallmark of this group of disorders. In addition to the dermatologic features, these syndromes have hamartomatous involvement of multiple tissues, especially the central nervous system and the eye. Neurocutaneous syndrome is a preferred term. [42]
Adenoma sebaceum
"Adenoma sebaceum of Pringle" (ASP) [Figure - 5] seen in Tuberous sclerosis is a misnomer. The tumor is not an adenoma and is not derived from sebaceous glands. The lesion is characterized by dermal fibrosis and associated vascular proliferation and dilatation. Changes in contiguous sebaceous glands and other adnexal structures are merely secondary. Thus, "angiofibroma" would be a more appropriate name. The histologic changes suggest that it is a hamartoma rather than a true neoplasm. [43]
 |
| Figure 5: Adenoma sebaceum, multiple angiofibromas over the face |
Keratosis follicularis
Keratosis follicularis (Darier′s disease) is characterized by keratotic papules predominately affecting the seborrheic regions such as the upper trunk and the head and neck areas [Figure - 6]. The term is a misnomer as the lesions are not limited to the hair follicles. [44]
 |
| Figure 6: Darier's disease showing keratotic papules over the face |
Follicular atrophoderma (Bazex-Dupre΄-Christol syndrome) This is an X-linked dominant condition characterised by the development of BCCs on the face, hypohidrosis, hypotrichosis and follicular atrophoderma. The latter refers to ice-pick marks or patulous follicles on the extremities. The term is a misnomer as no evidence of atrophy of the epidermis, hair or dermis has been reported, and the elastic fibers are normal. On histopathology, hair follicles appear abnormally wide, and are surrounded by an inflammatory cell infiltrate. [5]
Focal dermal hypoplasia (Goltz syndrome)
This rare mesoectodermal disorder is characterised by linear depressed lesions in conjunction with fat nodules, dysmelanosis, wart-like excrescences and variable bone, eye, tooth, hair and nail abnormalities. [45]
The term is a misnomer because, here, the defect not only involves the dermis but also the epidermis, the subcutis and even the underlying bones in combinations, and was first reported by Libermann in 1935. Goltz coined the term "Focal dermal hypoplasia" for the rare genodermatosis on the basis of histologically apparent areas of connective tissue hypoplasia. [46]
Keratitis, ichthyosis and deafness (KID) syndrome
The KID acronym does not accurately define this entity as the disorder is not an ichthyosis, because scaling is not the main cutaneous feature and not all patients have keratitis early in the course. This syndrome should be included under the general heading of congenital ectodermal defects as a keratodermatous ectodermal dysplasia. [47]
Macrocephaly-cutis marmorata telangiectatica congenita syndrome (M-CMTC)
Reticulated or confluent port-wine stains and persistent capillary malformations of the central face, rather than CMTC, are the most characteristic cutaneous vascular anomalies seen in so-called M-CMTC syndrome. The name macrocephaly-capillary malformations more accurately reflect the features of this syndrome. [48]
Misnomers in Eczema
Dyshidrosis and dyshidrotic eczema
The dyshidrotic vesicle is an intraepidermal, spongiotic lesion. The intraepidermal part of the eccrine sweat duct (acrosyringium) is not altered even by spongiosis. As the acrosyringium does not take part in formation of a dyshidrotic vesicle, the term "dyshidrosis" has to be regarded as a misnomer. Dyshidrosis is nothing but spongiotic dermatitis modified by the distinctive characteristics of palmar and plantar skin. [49]
Seborrheic dermatitis
Malassezia yeasts have been associated with seborrheic dermatitis. Abnormal or inflammatory immune system reactions to these yeasts may be related to the development of seborrheic dermatitis. [50] Seborrhea plays no part in the pathogenesis of the rash in most patients with seborrheic dermatitis, and the term "Dermatitis of the sebaceous areas" [Figure - 7] would be more accurate. [51]
 |
| Figure 7: Seborrheic dermatitis |
Blistering Disorders
Herpes gestationis
The disease was originally named on the basis of the morphological herpetiform features of the blisters, but is not related to any active or prior herpes virus infection, and Pemphigoid gestationis is a better term for this condition. [4]
Impetigo herpetiformis
In 1872, Hebra described impetigo herpetiformis as a pustular eruption with serious constitutional symptoms affecting women in pregnancy or in the puerperium. [52] Impetigo herpetiformis is a dermatosis of pregnancy with a misleading name given that the condition is now generally considered to be a rare form of pustular psoriasis during pregnancy. [4]
Transient acantholytic dermatosis (TAD)
TAD is a non-familial, non-immune-mediated acantholytic skin disorder that manifests as pruritic, discrete, edematous papules and/or a vesiculopapular rash, and is more commonly referred to as Grover disease, after Dr Ralph Grover, who first reported the condition in 1970. Grover disease may be the more appropriate terminology, because it is most likely a condition/syndrome caused by various etiologies resulting in the same clinical manifestations. In addition, the term TAD is misleading, considering Grover disease can, in fact, be persistent and show morphologies other than acantholysis. [53]
Diseases of Vessels and Vasculitis
Stasis ulcer
Leg ulcerations secondary to chronic venous insufficiency have been termed "stasis ulcers." This is based on an original idea proposed by Homans in 1917. However, since then, data has been generated suggesting that, in fact, "stasis" does not occur. Schwartzberg and Kirsner reviewed the information that has accumulated, refuting the concept of stasis, and suggest that the term "stasis ulcer" is a misnomer, and should be abandoned. [54]
Pyogenic granuloma
The word pyogenic granuloma or granuloma pyogenicum was introduced by Hartzell in 1904. [55] It is an inflammatory hyperplasia seen over the skin [Figure - 8] or oral mucosa. This term is a misnomer because the lesion is unrelated to infection and, in reality, arises in response to various stimuli such as low-grade local irritation, traumatic injury or hormonal factors and, histologically, it does not show granuloma either. [56] The term reactive hemangioma has been proposed as a more appropriate terminology. [57]
 |
| Figure 8: Pyogenic granuloma over the lip |
Pyoderma gangrenosum (PG)
Brunsting, Goeckerman and O′Leary in 1930 named it as PG in the belief that streptococcal infection was a significant component leading to secondary cutaneous gangrene. [58] Although the pathogenesis is not well understood, it is of an autoimmune etiology and not an infectious one. [59] Hence, the term pyoderma gangrenosum is a misnomer.
Sinusoidal hemangioma
Sinusoidal hemangioma is a misnomer as the lesion is a vascular malformation rather than a neoplasm. It is made of dilated interconnecting ("sinusoidal"), thin-walled channels with a single-layered lining endothelium and a lobular architecture. [60]
Verrucous hemangioma
Verrucous hemangioma refers to a rare hyperkeratotic congenital vascular malformation of the superficial and deep dermis. The term is a misnomer as the lesion is not a hemangioma (neoplasm) but a malformation, and it could be called as verrucous lymphovascular malformation. [61],[62]
Hobnail hemangioma (HH)
HH is currently classified as a benign vascular tumor. Immunostaining with the endothelial marker Wilms tumor 1 (WT1) helps distinguish between vascular neoplasms and malformations, being positive in the former and negative in the latter. On the basis of the WT1 negativity, it has been shown that HH is better considered as a lymphatic malformation rather than a lymphatic neoplasm. [63]
Lymphangiosarcoma
Lymphangiosarcoma is a misnomer as this malignancy arises from the blood vessels rather than the lymphatics. Hemangiosarcoma is a more appropriate term. [5]
Connective Tissue Diseases
Collagen disorders or collagen vascular disorders
Given that collagen is the most abundant protein within the connective tissue, connective tissue disorders are occasionally referred to as "collagen disorders." The term is a misnomer as connective tissue also contains other elements, such as elastin and glycoproteins. These diseases affect many structures in addition to vascular structures. At present, the idiom collagen disorders should be restricted to inherited conditions that affect the synthesis or expression of collagen, such as Ehlers-Danlos syndrome and osteogenesis imperfecta. [5]
Lupus anticoagulants (LA)
It is a double misnomer. LA were originally described in patients with systemic lupus erythematosus (SLE) and clinical bleeding. Following the original description, they were associated with numerous clinical conditions, and it was soon appreciated that there was not an increased risk of hemorrhage. Hence, the name is a misnomer, which has resisted attempts at modification. [64] The term was initially coined by Feinstein and Rappaport because of the anticoagulant activity observed in vitro, but is regarded as a misnomer as procoagulant activity occurs in vivo and most patients do not have lupus. [65]
Pigmentary Disorders
Chloasma
The term "chloasma" (from the Greek word "chloazein" meaning "to be green") is often used to describe melasma developing during pregnancy; however, as the pigmentation never appears to be green, the term "melasma" (from the Greek word "melas" meaning black) should be preferred. [66]
Nevus depigmentosus
It is a misnomer as the areas of leukoderma are hypomelanotic and not amelanotic. [5]
Other Dermatological Misnomers
Psoriasis
The name psoriasis derives from the Greek "psora," which means to itch. Still, this is a bit of a misnomer, as itch is not always a feature of the condition.
Auspitz sign
The eponymously credited sign was not first discovered by Heinrich Auspitz. Both Devergie jeune and Hebra observed this clinical sign earlier. [67]
Tinea amiantacea
Tinea amiantacea represents a particular reaction pattern of the scalp to various inflammatory scalp diseases [Figure - 9]. The most frequent skin diseases associated are psoriasis and seborrheic dermatitis. Staphylococci on the scalp could participate in the pathogenesis. [68] It is a misnomer to term this disease tinea because it is typically not associated with a dermatophytic infection. Pityriasis amiantacea will be a better term. [20]
 |
| Figure 9: Tinea amiantacea |
Erythema toxicum neonatorum
Erythema toxicum neonatorum, or toxic erythema of the newborn, is an uncommon, self-limiting, benign dermatosis of unknown etiology affecting both sexes equally. [69] It is a misnomer as there will not be any toxic features in the neonate.
Porokeratosis
Porokeratosis is a misnomer. While the cornoid lamellae occasionally correspond to ostia of eccrine glands or hair-follicles, this finding is fortuitous as the peripheral border of the lesions moves centrifugally and is not permanently bound to the epidermal adnexae. [70]
Pretibial myxedema
Although the condition is most often confined to the pretibial area, it may occur anywhere on the skin, including the thighs, shoulders, hands and face. Furthermore, myxedema refers to "mucus edema," while true pathology lies in hyaluronic acid deposition in the dermis and subcutis of the skin lesions. Thyroid dermopathy is perhaps a more appropriate term for this condition. [71]
Sarcoidosis
From Boeck′s fallacious idea that this disease represented a connective tissue neoplasm or sarcoma, we inherit the term "sarcoid" (Greek: sarx = flesh). [72]
Lupus pernio
A cutaneous manifestation that is characteristic of sarcoidosis, the term lupus pernio is a misnomer because the condition is not associated with lupus and has no association with pernio. [20]
Leprosy
The Hebrew word used in the Bible to denote the unclean condition was ts-araath, a word that is of religious significance, implying the stigma of punishment by God. The disease we know as leprosy (Hansen′s disease) was known to the Greeks as elephantiasis because of the bodily deformities, and the term lepra was used by them for a scaly skin condition. The Bible translators faced with the problem of finding a Greek translation of the Hebrew ts-araath and chose the word lepra. [73],[74]
When the Hebrew text of the Old Testament was translated into Greek about 250 BC, ts-ara ′ath was rendered as lepra, a generic term applied to skin lesions, which, by transliteration, reached the English versions as leprosy. [75] Therefore, the word leprosy is a misnomer.
Knuckle pads
Knuckle pads occur from benign thickening of the skin, principally the epidermis. Despite the name, knuckle pads most commonly overlie the proximal interphalangeal joints and not over the knuckles or the metacarpophalangeal joints. [76]
Piezogenic pedal papules
Piezogenic pedal papules were first described by Shelley and Rawnsley in 1968. This term is somewhat of a misnomer as piezogenic means "producing pressure," when, in fact, these lesions are produced by pressure. [77]
Juvenile xanthogranuloma
It is predominantly a disease of infancy or early childhood, although adults may also be affected. The term juvenile makes it a misnomer. [78]
Granuloma annulare
It is a misnomer as it is neither a granuloma in conventional meaning nor necessarily annular. The revised terminology is necrobiotic papulosis. [57]
Papular urticaria
This term is a misnomer as it is not a variant of urticaria as the name suggests and lesions can also present as vesicles.
Urticaria pigmentosa
It is a misnomer as the lesions are not true urticaria, are only lightly pigmented and more telangiectatic.
Siliconoma
The term siliconoma, coined in 1964 to describe silicone granulomas, is a misnomer as silicone itself cannot become a tumor (-oma) nor can the cells that phagocytize silicone multiply in a tumorous fashion. [79]
Microdermabrasion
Microdermabrasion is a misnomer as the technique does not cause injury to the dermis, but rather acts at the level of the epidermis. [5]
Chemosurgery
Chemosurgery is a term occasionally applied to Mohs micrographic surgery, which, when used today, is a misnomer. When Dr. Frederick Mohs initially introduced the procedure, zinc chloride chemical paste was applied to the tumor and the surrounding skin for fixation.
Since 1974, however, the procedure has involved excising the tumor with special repeated histologic examination without the use of in vivo chemical fixation. [80]
Misnomers in Dermatopathology
Acanthosis nigricans
Acanthosis nigricans is a well-defined clinical entity, yet is at least a partial misnomer. Histopathologically, despite the term "acanthosis," the actual amount of acanthosis, or thickening of the stratum spinosum, is variable and typically mild. [81]
Horn cysts
These intraepidermal whorls of invaginated keratin found in seborrheic keratoses are not true cysts because each connects to the skin surface via a prominent ostium. Horn pseudocysts have been proposed as a more appropriate term. [5]
Pautrier′s microabscess
Pautrier′s microabscess is a collection of atypical lymphocytes found within the epidermis of lesions of cutaneous T-cell lymphoma. The term is a misnomer as an abscess characteristically refers to a collection of neutrophils or, alternatively, to a cavity formed by liquefactive necrosis within a solid tissue. [5]
Darier was the first person to describe it, and Pautrier himself expressed surprise that he was given credit for Darier′s contribution and had acknowledged that it should have been termed Darier′s epidermal nest instead. [82]
Scleredema adultorum of Buschke
Scleredema adultorum of Buschke is a misnomer as relatively high proportion of cases occur in children, and histopathological examination reveals neither sclerosis nor edema, but rather a thickened dermis with mucopolysaccharide deposition between collagen bundles. [83],[84]
Granuloma faciale
Granuloma faciale is a misnomer because its histologic appearance does not demonstrate granulomatous inflammation [85] and, also, this condition is reported to occur on extra-facial areas of the body, such as trunk and extremities. [86]
Borst Jadassohn phenomenon
Borst and Jadassohn had described quite different biological phenomena, and that the term "Borst-Jadassohn intraepidermal epithelioma" therefore should be discarded. Borst was describing a squamous cell carcinoma of the lip that secondarily invaded the epidermis and that the Jadassohn lesion has a mixed etiology and that intraepidermal BCC seldom occurs. The Jadassohn phenomenon was most often associated with benign lesions such as seborrheic keratosis (especially if irritated by infection or trauma) or entirely intraepidermal sweat gland tumors (hidroacanthoma simplex of Smith and Coburn). [87],[88]
Extracellular cholesterosis of erythema elevatum diutinum (EED)
EED is a rare disease of unknown origin that belongs to the spectrum of leukocytoclastic vasculitis. Chronic lesions of EED contain lipid deposits, for which the term extracellular cholesterosis has been coined. Electron microscopic examination revealed a heavy, exclusively intracellular lipid deposition that consisted of lipid droplets, myelin figures and rare cholesterol clefts within histiocytes and also within epidermal keratinocytes, mast cells, pericytes and lymphocytes. These findings are in keeping with the results of previous ultrastructural studies, and suggest that the term extracellular cholesterosis is a misnomer; intracellular lipidosis would more accurately describe the lipid deposition. [89]
Lupus erythematosus (LE) cell
LE cells, if present in large numbers, are highly suggestive of SLE, but it is also seen in other chronic inflammatory autoimmune diseases like chronic discoid LE, systemic sclerosis and rheumatoid arthritis. [88]
To conclude, we are all aware of the deficiencies of these terminologies and labelling of the diseases, syndromes and signs. They were introduced when we had limited knowledge about the pathophysiology, etiology, histopathology and other cellular receptor marker studies. These terminologies have served their purpose, and they still remind us about the history and what has gone into it to earn this name. Renaming these misnomers is a continuous process that has to proceed along with advances made in dermatology.
| 1. |
Osler W. Anemiasplenica. Trans Assoc Am Phys 1902;17:429-61.
[Google Scholar]
|
| 2. |
Garner BA. Garner's Modern American Usage. 3 rd ed. New York: Oxford University Press; 2009 p. 542.
rd ed. New York: Oxford University Press; 2009 p. 542.'>[Google Scholar]
|
| 3. |
Musray JA, Bradley H, Craigie WA, Onions CT, editors. The Oxford English Dictionary. Vol. 3. Oxford: Clarendon Press; 1961. p. 250.
[Google Scholar]
|
| 4. |
Kanwar AJ, De D. superficial fungal infections. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3rd ed. Mumbai: Bhalani Publishing House; 2008. p. 252-97.
[Google Scholar]
|
| 5. |
Barankin B, Freiman A. Misnomers in Dermatology. J Cutan Med Surg 2005;9:284-8.
[Google Scholar]
|
| 6. |
Chen TM, George S, Woodruff CA, Hsu S. Clinical manifestations of varicella-zoster virus infection. Dermatol Clin 2002;20:267-82.
[Google Scholar]
|
| 7. |
Schwartz RA. Kaposi's sarcoma: Advances and perspectives. J Am Acad Dermatol 1996;34:804-14.
[Google Scholar]
|
| 8. |
Hacker P. Botryomycosis. Int J Dermatol 1983;22:455-8.
[Google Scholar]
|
| 9. |
Singh G, Kaur V, Singh S. Bacterial infections. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3rd ed. Mumbai: Bhalani Publishing House; 2008. p. 223-51.
[Google Scholar]
|
| 10. |
Coyle MB, Lipsky BA. Coryneform bacteria in infectious diseases: Clinical and laboratory aspects. Clin Microbiol Rev 1990;3:227-46.
[Google Scholar]
|
| 11. |
Blaise G, Nikkels AF, Hermanns-Lê T, Nikkels-Tassoudji N, Piérard GE. Corynebacterium-associated skin infections. Int J Dermatol 2008;47:884-90.
[Google Scholar]
|
| 12. |
Treadwell TA, Holman RC, Clarke MJ, Krebs JW, Paddock CD, Childs JE. Rocky Mountain spotted fever in the United States, 1993-1996. Am J Trop Med Hyg 2000;63:21-6.
[Google Scholar]
|
| 13. |
Parkash S, Chandrasekaran V. Sebaceous cyst-a misnomer. J Indian Med Assoc 1982;79:29-31.
[Google Scholar]
|
| 14. |
Lefkowitz A, Schwartz RA, Lambert WC. Nevus comedonicus. Dermatology 1999;199:204-7.
[Google Scholar]
|
| 15. |
Hafner C, Hartmann A, Real FX, Hofstaedter F, Landthaler M,Vogt T. Spectrum of FGFR3 Mutations in Multiple Intraindividual Seborrheic Keratoses. J Invest Dermatol 2007;127:1883-5.
[Google Scholar]
|
| 16. |
Hollander EV. Beitrage zur Fruhdiagnose des Darmcarcinomas (Hereditatsverhaltnisse und Hautveranderungen. Deutsche Medicinische Wochenschrift 1900;26:483-5.
[Google Scholar]
|
| 17. |
Guitart J, Rosenbaum MM, Requena L. 'Eruptive syringoma': A misnomer for a reactive eccrine gland ductal proliferation? J Cutan Pathol 2003;30:202-5.
[Google Scholar]
|
| 18. |
McCalmont T. Adnexal Neoplasms. In: Bolognia J, Jorizzo J, Rapini R, editors. Dermatology. 1 st ed. Amsterdam: Mosby Elsevier. 2003. p. 1733-55.
[Google Scholar]
|
| 19. |
Kwittken J. Papular elastosis. Cutis 2000;66:81-3.
[Google Scholar]
|
| 20. |
Nosrati N, Harting MS, Yang DJ, Shen YA, Maender JL, Jogi RP, et al. Dermatology misnomers. Dermatol Online J 2008;14:22.
[Google Scholar]
|
| 21. |
Weinberger CH, Dinulos JG, Perry AE. An enlarging tender nodule on the finger of a 4-year-old boy: An unusual presentation of infantile myofibromatosis. J Am Acad Dermatol 2007;57:30-2.
[Google Scholar]
|
| 22. |
Dakin MC, Leppard B, Theaker JM. The palisaded, encapsulated neuroma (solitary circumscribed neuroma). Histopathology 1992;20:405-10.
[Google Scholar]
|
| 23. |
Ackerman AB, Mones JM. Solar (actinic) keratosis is squamous cell carcinoma. Br J Dermatol 2006;155:9-22.
[Google Scholar]
|
| 24. |
Oppel T, Korting HC. Actinic keratosis: The key event in the evolution from photoaged skin to squamous cell carcinoma. Skin Pharmacol Physiol 2004;17:67-76.
[Google Scholar]
|
| 25. |
Pinkus H. Premalignant fibroepithelial tumors of skin. AMA Arch Derm Syphilol 1953;67:598-615.
[Google Scholar]
|
| 26. |
Su MW, Fromer E, Fung MA. Fibroepithelioma of pinkus. Dermatol Online J 2006;12:2.
[Google Scholar]
|
| 27. |
Saida T. Heterogeneity of the site of origin of malignant melanoma in ungual areas: Subungual malignant melanoma may be a misnomer. Br J Dermatol 1992;126:529.
[Google Scholar]
|
| 28. |
Verneuil A. Études sur les tumeurs de la peau; de quelques maladies des glandes sudoripares. Arch Gén Méd 1854;5:447-68.
[Google Scholar]
|
| 29. |
Sellheyer K, Krahl D. ''Hidradenitissuppurativa'' is acne inversa! An appeal to (finally) abandon a misnomer. Int J Dermatol 2005;44:535-40.
[Google Scholar]
|
| 30. |
Ogunbiyi A, George A. Acne keloidalis in females: Case report and review of literature. J Natl Med Assoc 2005;97:736-8.
[Google Scholar]
|
| 31. |
Kelly AP. Pseudofolliculitis barbae and acne keloidalis nuchae. Dermatol Clin 2003;21:645-53.
[Google Scholar]
|
| 32. |
Saurat JH, Sorg O. Chloracne, a misnomer and its implications. Dermatology 2010;221:23-6.
[Google Scholar]
|
| 33. |
Cribier B. The red face:art, history and medical representations. Ann Dermatol Venereol 2011;138:172-8.
[Google Scholar]
|
| 34. |
Simon N. Ist der lupus miliaris disseminates tuberculoser Aetiologie? Hautarzt 1975;26:625-30.
[Google Scholar]
|
| 35. |
Van de Scheur MR, van der Waal RI, Starink TM. Lupus miliaris disseminates faciei: A distinctive rosacea-like syndrome and not a granulomatous form of rosacea. Dermatology 2003;206:120-3.
[Google Scholar]
|
| 36. |
O'Driscoll T, Morgan G. Acne agminata of the eyelid. Proc R Soc Med 1974;67:869-70.
[Google Scholar]
|
| 37. |
Sperling LC, Sau P. The follicular degeneration syndrome in black patients. 'Hot comb alopecia_ revisited and revised. Arch Dermatol 1992;128:68-74.
[Google Scholar]
|
| 38. |
Trakimas C, Sperling LC, Skelton HG 3rd, Smith KJ, Buker JL. Clinical and histologic findings in temporal triangular alopecia. J Am Acad Dermatol 1994;31:205-9.
[Google Scholar]
|
| 39. |
Powell J, Ferguson DJ, Dawber RP. Is kinky-hair disease a misnomer for Menkes syndrome? Arch Dermatol 2001;137:92-3.
[Google Scholar]
|
| 40. |
Chintapatla S, Safarani N, Kumar S. Sacrococcygeal pilonidal sinus: Historical review, pathological insight and surgical options. Tech Coloproctol 2003;7:3-8.
[Google Scholar]
|
| 41. |
Al-Jaberi TM. Excision and simple primary closure of chronic pilonidal sinus. Euro J Surg 2001;167:133-5.
[Google Scholar]
|
| 42. |
Diaz JH. Perioperative management of children with congenital phakomatoses. Paediatr Anaesth 2000;10:121-8.
[Google Scholar]
|
| 43. |
Sanchez NP, Wick MR, Perry HO. Adenoma sebaceum of Pringle: A clinicopathologic review, with a discussion of related pathologic entities. J Cutan Pathol 1981;8:395-403.
[Google Scholar]
|
| 44. |
Grandbois J. Darier's disease. Can Med Assoc J 1952;67:152-3.
[Google Scholar]
|
| 45. |
Gangopadhyay KA. Focal dermal hypoplasia syndrome. Indian J Dermatol Venereol Leprol 1999;65:281-2.
[Google Scholar]
|
| 46. |
Goltz RW, Peterson WC, Gorlin RJ, Ravits HG. Focal dermal hypoplasia. Arch Dermatol 1962;86:708-17
[Google Scholar]
|
| 47. |
Caceres-Rios H, Tamayo-Sanchez L, Duran-Mckinster C, de la Luz Orozco M, Ruiz-Maldonado R. Keratitis, ichthyosis, and deafness (KID syndrome): Review of the literature and proposal of a new terminology. Pediatr Dermatol 1996;13:105-13.
[Google Scholar]
|
| 48. |
Wright DR, Frieden IJ, Orlow SJ, Shin HT, Chamlin S, Schaffer JV, et al. The misnomer "macrocephaly-cutis marmorata telangiectatica congenital syndrome": Report of 12 new cases and support for revising the name to macrocephaly-capillary malformations. Arch Dermatol 2009;145:287-93.
[Google Scholar]
|
| 49. |
Kutzner H, Wurzel RM, Wolff HH. Are acrosyringia involved in the pathogenesis of "dyshidrosis"? Am J Dermatopathol 1986;8:109-16.
[Google Scholar]
|
| 50. |
Gupta AK, Bluhm R, Cooper EA, Summerbell RC, Batra R. Seborrheic dermatitis. Dermatol Clin 2003;21:401-12.
[Google Scholar]
|
| 51. |
Burton JL, Pye RJ. Seborrhoea is not a feature of seborrhoeic dermatitis. Br Med J 1983;286:1169-70.
[Google Scholar]
|
| 52. |
Feiwel M, Ferriman D. Impetigo herpetiformis. ProcR Soc Med 1957;50:392-4.
[Google Scholar]
|
| 53. |
Weaver J, Bergfeld WF. Grover disease (transient acantholytic dermatosis). Arch Pathol Lab Med 2009;133:1490-4.
[Google Scholar]
|
| 54. |
Schwartzberg JB, Kirsner RS. Stasis in venous ulcers: A misnomer that should be abandoned. Dermatol Surg 2000;26:683-4.
[Google Scholar]
|
| 55. |
Hartzell MB. Granuloma pyogenicum. J Cutan Dis Syph 1904;22:520-5.
[Google Scholar]
|
| 56. |
Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: A review. J Oral Sci 2006 48:167-75.
[Google Scholar]
|
| 57. |
Malak JA, Kibbi AG. Revised terminology in dermatology: A call for the new millennium. Arch Dermatol 2001;137:93-4.
[Google Scholar]
|
| 58. |
Brunsting LA, Goecker WH, O'Leary PA. Pyoderma (ecthyma) gangrenosum: Clinical and experimental observations in five cases occurring in adults. Arch Dermatol 1930;22:655-80.
[Google Scholar]
|
| 59. |
Hasselmann DO, Bens G, Tilgen W, Reichrath J. Pyodermagangrenosum: Clinical presentation and outcome in 18 cases and review of the literature. J Dtsch Dermatol Ges 2007;5:560-4.
[Google Scholar]
|
| 60. |
Enjolras O, Wassef M, Brocheriou-Spelle I, Josset P, Tran Ba Huy P, Merland JJ. Sinusoidal hemangioma. Ann Dermatol Venereol 1998;125:575-80.
[Google Scholar]
|
| 61. |
Requena L, Sangueza OP. Cutaneous vascular anomalies. Part I. Hamartomas, malformations, and dilation of preexisting vessels. J Am Acad Dermatol 1997;37:523-49.
[Google Scholar]
|
| 62. |
Brown A, Warren S, Losken HW, Morrell DS. Verrucous lymphovascular malformation versus verrucous hemangioma: controversial nomenclature. Cutis 2008;81:390-6.
[Google Scholar]
|
| 63. |
Trindade F, Kutzner H, Tellechea Ó, Requena L, Colmenero I. Hobnail hemangioma reclassified as superficial lymphatic malformation: A study of 52 cases. J Am Acad Dermatol 2012;66:112-5.
[Google Scholar]
|
| 64. |
Triplett DA, Brandt JT. Lupus anticoagulants: Misnomer, paradox,riddle, epiphenomenon. Hematol Pathol 1988;2:121-43.
[Google Scholar]
|
| 65. |
Gibson GE, Su WP, Pittelkow MR. Antiphospholipid syndrome and the skin. J Am Acad Dermatol 1997;36:970-82.
[Google Scholar]
|
| 66. |
Bandyopadhyay D. Topical treatment of melasma. Indian J Dermatol 2009;54:303-9.
[Google Scholar]
|
| 67. |
Holubar K, Fatoviæ-Ferenciæ S. Papillary tip bleeding or the Auspitz phenomenon: A hero wrongly credited and a misnomer resolved. J Am Acad Dermatol 2003;48:263-4.
[Google Scholar]
|
| 68. |
Abdel-Hamid IA, Agha SA, Moustafa YM, El-Labban AM. Pityriasis amiantacea: A clinical and etiopathologic study of 85 patients. Int J Dermatol 2003;42:260-4.
[Google Scholar]
|
| 69. |
Mahajan VK, Sharma NL. Erythema toxicum neonatorum. Indian Pediatr 2010;47:793.
[Google Scholar]
|
| 70. |
Kanitakis J, Euvrard S, Faure M, Claudy A. Porokeratosis and immunosuppression. Eur J Dermatol 1998;8:459-65.
[Google Scholar]
|
| 71. |
Fatourechi V, Pajouhi M, Fransway AF. Dermopathy of Graves disease (pretibial myxedema). Review of 150 cases. Medicine (Baltimore) 1994;73:1-7.
[Google Scholar]
|
| 72. |
Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med 2007;357:2153-65.
[Google Scholar]
|
| 73. |
Lendrum FC. The name Leprosy. Am J Trop Med Hyg 1952;1:999-1008.
[Google Scholar]
|
| 74. |
Cule J. Biblical ills and remedies. J R Soc Med 1987;80:534-5.
[Google Scholar]
|
| 75. |
Davies ML, Davies TA. Biblical ills and remedies. J R Soc Med 1987;80:534-5.
[Google Scholar]
|
| 76. |
Paller AS, Hebert AA. Knuckle pads in children. Am J Dis Child 1986;140:915-7.
[Google Scholar]
|
| 77. |
Maari C, Powell J. Atrophies of Connective Tissue. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2nd ed. Amsterdam : Mosby Elsevier. 2008. p 1505-14.
[Google Scholar]
|
| 78. |
Saad N, Skowron F, Dalle S, Forestier JY, Balme B, Thomas L. Multiple adult xanthogranuloma: Case report and literature review. Dermatology 2006;212:73-6.
[Google Scholar]
|
| 79. |
Duffy DM. The Silicone conundrum: A battle of anecdotes. Dermatol Surg. 2002;28:590-4
[Google Scholar]
|
| 80. |
Mohs FE. Mohs micrographic surgery. A historical perspective. Dermatol Clin 1989;7:609-11.
[Google Scholar]
|
| 81. |
Rogers DL. Acanthosisnigricans. Semin Dermatol 1991;10:160-3.
[Google Scholar]
|
| 82. |
Omura GA. Darier, Pautrier, and the "microabscesses" of mycosis fungoides. J Am Acad Dermatol 2002;46:320-1.
[Google Scholar]
|
| 83. |
Greenberg LM, Geepert C, Worthen HG, Good RA. SCLEREDEMA "ADULTORUM" IN CHILDREN. Report of three cases with histochemical study and review of world literature. Paediatrics 1963;32:1044-54.
[Google Scholar]
|
| 84. |
Singal A, Gandhi V, Bhattacharya SN, Khanna G, Baruah MC. Scleredema adultorum of buschke associated with non-scarring alopecia of scalp. Indian J Dermatol Venereol Leprol 1999;65:38-9.
[Google Scholar]
|
| 85. |
Ortonne N, Wechsler J, Bagot M, Grosshans E, Cribier B. Granuloma faciale: A clinic opathologic study of 66 patients. J Am Acad Dermatol 2005;53:1002-9.
[Google Scholar]
|
| 86. |
Crowson AN, Mihm MC Jr, Magro CM. Cutaneous vasculitis: A review. J Cutan Pathol 2003;30:161-73.
[Google Scholar]
|
| 87. |
Mitchell RE. Squamous cell carcinoma developing in the Jadassohn phenomenon: A case report. Australas J Dermatol 1975;16:79-82.
[Google Scholar]
|
| 88. |
Madke B, Doshi B, Pande S, Khopkar U. Phenomena in dermatology. Indian J Dermatol Venereol Leprol 2011;77:264-75.
[Google Scholar]
|
| 89. |
Kanitakis J, Cozzani E, Lyonnet S, Thivolet J. Ultrastructural study of chronic lesions of erythema elevatum diutinum:"extracellular cholesterosis" is a misnomer. J Am Acad Dermatol 1993;29:363-7.
[Google Scholar]
|
Fulltext Views
12,022
PDF downloads
3,652





