Mixed lymphatic malformation of tongue in a child with excellent response to oral sirolimus
Corresponding author: Dr. Suman Patra, Department of Dermatology, Venereology and Leprology, All India Institute of Medical Sciences, Jodhpur, India. patrohere@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agrawal A, Kaur M, Bains A, Yadav T, Patra S. Mixed lymphatic malformation of tongue in a child with excellent response to oral sirolimus. Indian J Dermatol Venereol Leprol. 2024;90:816-8. doi: 10.25259/IJDVL_1201_2023
Dear Editor,
A 7-year-old boy presented with gradually progressing tongue swelling with multiple asymptomatic, fluid-filled, lesions over the surface since birth. It was associated with restricted tongue mobility, speech disarticulation, and dysphagia for solid foods. There was a history of recurrent tongue swelling with spontaneous resolution within a few days. Multiple episodes (2–3/year) occured which used to resolve in 7–8 days. There was no history of disturbed sleep quality, dyspnea, or bleeding. Examination revealed soft-to-firm macroglossia along with multiple clear and haemorrhagic vesicles distributed over its dorsal and ventral surfaces [Figure 1]. We made a clinical diagnosis of mixed (capillary-lymphatic) malformation of the tongue. Magnetic resonance imaging (MRI) showed infiltrative T2W/STIR hyperintense soft tissue mass with internal blood-fluid level, heterogeneous contrast enhancement in the floor of the mouth, involving the root of the tongue, sublingual and submandibular spaces extending to the intrinsic muscles of the tongue anteriorly with both small and large cystic areas [Figure 2a]. Repeat MRI at 5 months showed overall lesional improvement in the form of the reduced size of the cystic areas [Figure 2b]. As the lesions were unsuitable for surgery, and there was a lack of specific treatment guidelines, we decided to administer oral sirolimus at the dose of 0.8mg/kg/m2/day. Genetic analysis was not done due to financial constraints. The patient was initially started on 0.5 mg twice daily for 1 month and hiked to 0.5mg in the morning and 0.75 mg in the evening for the next 8 months. He was followed up monthly with blood sirolimus levels (with a target level of 5–15 ng/mL) and a complete blood count. The lesions started to respond in the second month with a reduction in the number of surface vesicles [Figure 3a]. We noted around 70–80% clinical improvement reflected by a substantial reduction in the number of lesions and size of the tongue [Figure 3b]. The frequency of recurrent swellings was reduced post-treatment. There was resolution of difficulty in speech and dysphagia as well. He is currently continuing therapy with a plan to continue for a total of 18–24 months or complete subsidence of the lesion, whichever is earlier.

- Diffuse infiltration of the tongue with multiple clear-fluid filled and haemmorhagic vesicles at baseline.
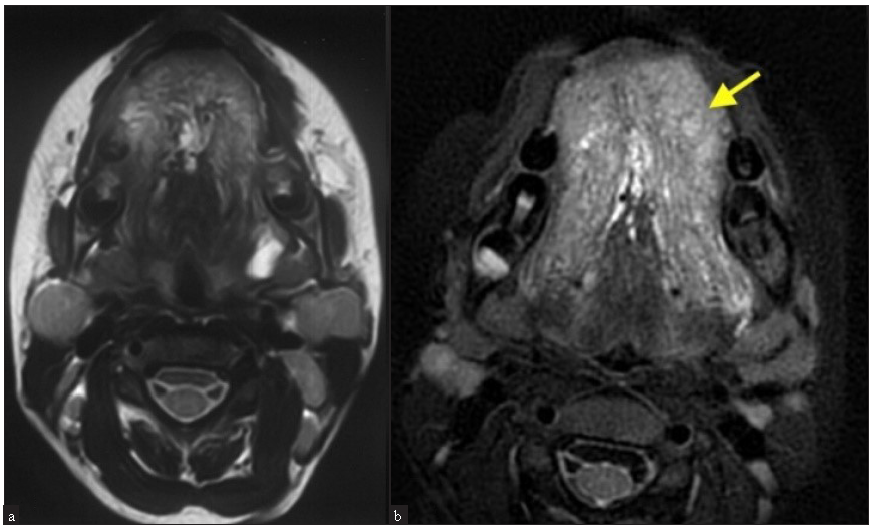
- (a) MRI of the tongue at baseline (Axial view) showing mixed (microcystic and macrocystic) lymphatic malformation in the tongue. (b) At 5 months (Axial view) with a decrease in lesion size (Tongue marked with a yellow arrow).

- 20–25% decrease in lesions after 2 months of oral sirolimus.
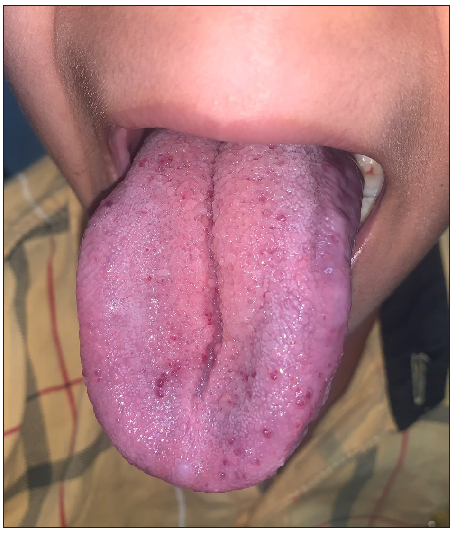
- 70–80% decrease in lesions after 9 months of oral sirolimus.
Lymphatic malformations (LM) are slow-flow congenital vascular anomalies.1 Around 48% of lesions involve the head and neck. LMs in the neck can cause dysphagia and be life-threatening due to airway obstruction in cases of laryngo-bronchial microcystic LMs or circumferential subglottic LMs.2 Current treatment options include medical therapy such as sildenafil, and propranolol along with surgical excision, sclerotherapy, radiofrequency ablation, and ablative lasers. Sclerotherapy is most commonly used in macrocystic malformations and is effective in almost 73–97% of cases. Skin necrosis, hematoma formation, infection, and scarring are the usual complications. Surgical excision, another option for macrocystic disease, is more extensive, and microcystic LMs are difficult to be excised completely and have a higher recurrence risk. Surface ablative measures like radiofrequency and carbon dioxide laser only provide symptomatic relief. Deeper lesions require local or regional anaesthesia and can result in scarring.3 Propranolol lacks efficacy in such malformations. Sildenafil showed better response in macrocystic LMs as compared to microcystic ones.4
Current understanding of pathogenesis implicates abnormal activation of the phosphatidylinositol-3΄-kinase (PI3K)/AKT/mTOR pathway in the development of LMs.5 Sirolimus, an inhibitor of mammalian target of rapamycin (mTOR) has recently gained attention for the treatment of vascular malformations and tumours. It is effective in lymphatic malformations of the head and neck. Response is usually partial and earlier initiation of therapy is associated with better results. There are fewer reports of predominantly microcystic lesions of the tongue. The usual treatment duration for sirolimus ranges from 6 months to 4 years and hyperlipidaemia, neutropenia, and infections are common adverse events reported.2 Our patient did not receive cotrimoxazole prophylaxis. In a systematic review by Wiegand et al, 43.8% of patients were administered sulfamethoxazole-trimethoprim for prevention of Pneumocystis pneumonia infection prophylactically. However, only one patient reported the occurrence of bacterial pneumonia, but its causative organism was not listed.6 Relapse has been reported after discontinuation of sirolimus, and in a series of 56 patients with complex LMs recurrence rate was found to be around 8%.7 We did not experience any adverse events in our case.
To our best knowledge, this is the first such report described by a patient of Indian ethnicity. This report adds to the growing literature on the efficacy of sirolimus in the management of head and neck LM in paediatric population.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Contribution of the ISSVA 2014/2018 Classification. Ann Pathol. 2015;41:58-70.
- [CrossRef] [PubMed] [Google Scholar]
- Refractory head and neck lymphatic malformation in infants treated with sirolimus: A case series. Front Oncol. 2021;11:616702.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Management of head and neck lymphatic malformations. Facial PlastSurg. 2012;28:596-602.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of oral sildenafil in treatment of pediatric head and neck lymphatic malformations. Acta Otolaryngol. 2017;137:674-8.
- [CrossRef] [PubMed] [Google Scholar]
- Genetics of lymphatic anomalies. J Clin Invest. 2014;124:898-904.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Efficacy of sirolimus in children with lymphatic malformations of the head and neck. Eur Arch Otorhinolaryngol. 2022;279:3801-10.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effectiveness of sirolimus in the treatment of complex lymphatic malformations: Single center report of 56 cases. J Pediatr Surg. 2020;55:2454-8.
- [CrossRef] [PubMed] [Google Scholar]





