Translate this page into:
Monkeypox disease in India: Unusual clinical presentation
Corresponding author: Dr. Bijaylaxmi Sahoo, Department of Dermatology, Maulana Azad Medical College, New Delhi, India. blsahooacad@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sahoo B, Kumar S, Monalisa K, Solanki B, Relhan V. Monkeypox disease in India: Unusual clinical presentation. Indian J Dermatol Venereol Leprol. 2024;90:345-8. doi: 10.25259/IJDVL_765_2022
Dear Editor,
Herein, we report a case series of monkeypox (MP) disease from India. The data is presented from an MP-designated tertiary care hospital in North India, from July 2022 to October 2022.
Out of the 12 confirmed cases of MP, 5 (42%) were males and 7 (58%) were females. The median age at presentation was 28 years. In all cases, patients reported having a single sexual partner, except for one patient who had two partners, and one denied any sexual contact. Six (50%) of these patients had a history of travelling to Nigeria within the past 6 months.
Majority of the lesions observed were umbilicated papulo-pustular and crusted ulcers, predominantly located on the genitalia in every patient [Figures 1–5]. Involvement of the palms and soles were noted in 9/12 (75%) patients. In all, number of lesion count exceeded 50. Oral erosion with pharyngitis and genital erosions were present in 10 (83%) patients each, while significant lymph node enlargement was observed in 7 (58%) patients. One patient was HIV positive, while all tested negative for venereal disease reserach laboratory (VDRL), HBsAg and anti-HCV antibodies. The patients’ details are summarised in Table 1.

- Multiple, well-defined, round-to-oval umbilicated lesions with brownish-black thick crusting present over the base of penis, arranged singly and in groups.

- Multiple well-defined erosions present over the base of penis with erythematous base and marginal re-epithelization.

- Multiple discrete to coalescent ulcers present over the scrotum and inner aspect of bilateral thighs with erythematous base and marginal hyperpigmentation.

- Few scattered umbilicated papules present over the chest and abdomen.

- Multiple skin-coloured, umbilicated papules and vesiculopustular lesions present over the forehead.

- Few erythematous papules present over the palm and soles.

- Multiple skin-coloured umbilicated papules present over the oral mucosa with overlying greyish slough.
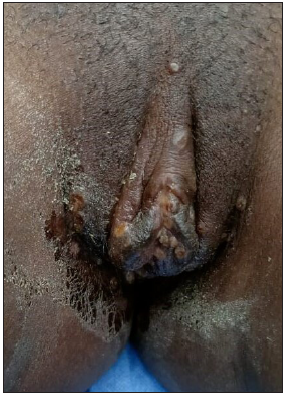
- Multiple umbilicated papules and erosions present over the clitoris, labia majora and minora.

- Multiple umbilicated papules present over the back and right arm.
| Case | Age & Sex | Onset site/lesion count | Nationality | Sexual behaviour/partners/marital status | Last sexual contact | H/o international travel/months | Constitutional features | Lesions type | Mucosa | Palm and sole | Lymphadenopathy | HIV/VDRL/Hep B,C |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Confirmed cases | ||||||||||||
| 1 | 34 M | Genitalia ≈30 | Indian | Heterosexual (single regular partner)/married | 15 days back, protected | No | Fever, lethargy, low mood | VP, erosions, crusting, umbilication, ulcers | – | + | – | NR |
| 2 | 34 M | Genitalia ≈20 | Nigerian | Heterosexual (single regular partner)/unmarried | 1 month back, unprotected | No | Lethargy, difficulty in swallowing, low mood | VP, erosions, thick crusted ulcers | Oral erosion+ & pharyngitis, genital erosion+ | + | B/L submental, retro-auricular LNs | NR |
| 3 | 35 M | Genitalia ≈20 | Nigerian | Heterosexual (single regular partner)/unmarried | 1 month back, unprotected | No | Fever, lethargy. | VP, erosions, crusted ulcers | _ | + | B/L submandibular, inguinal | NR |
| 4 | 31 F | Genitalia ≈20 | Nigerian | Heterosexual (single regular partner)/unmarried | 1 year back | 5 months back to Nigeria | Fever, lethargy, difficulty in swallowing | VP, erosions, crusted ulcers, umbilication | Oral erosion, Genital erosion+ | + | B/L Inguinal | NR |
| 5 | 22 F | Foot ≈20 | Nigerian | Heterosexual (2 sexual partners)/unmarried | 4 days back | 35 days back to Nigeria | Fever, difficulty in swallowing | VP, erosions, crusting, umbilication | Oral erosion, genital erosion+ | + | - | NR |
| 6 | 25 F | Genitalia ≈20 | Nigerian | Heterosexual (single regular partner)/unmarried | 1 month back, protected | 1 month back to Nigeria | Fever, difficulty in swallowing | VP, erosions, crusted ulcers | genital erosion+ | - | - | NR |
| 7 | 24 F | Genitalia ≈20 | Nigerian | Heterosexual (single regular partner)/unmarried | 1 weekback, protected | 4 month back to Nigeria | Fever, difficulty in swallowing | VP, erosions, crusted ulcers | genital erosion+ | - | B/L inguinal LN | HIV + |
| 8 | 24 M | Hand ≈20 | Nigerian | Heterosexual (single regular partner)/unmarried | 1 weekback, unprotected | 3 month back to Nigeria | Fever, difficulty in swallowing | VP, erosions, crusted ulcers | Whitish papule over tonsils | + | Left inguinal LN | NR |
| 9 | 24 M | Hand ≈20 | Nigerian | Heterosexual (single regular partner)/unmarried | 1 month back protected | - | Fever, difficulty in swallowing | VP, erosions, crusted ulcers | genital erosion+ | + | - | NR |
| 10 | 30 F | Genitalia ≈20 | Nigerian | Denied | - | 4 month back to Nigeria | Difficulty in swallowing | VP, erosions, crusted ulcers | genital erosion+ | - | - | NR |
| 11 | 30 F | Genitalia ≈20 | Nigerian | Heterosexual (single regular partner)/unmarried | 1 month back, protected | - | - | VP, erosions, crusted ulcers | genital erosion+ | + | Left axillary LN | NR |
| 12 | 22 F | Genitalia ≈20 | Nigerian | Heterosexual (single regular partner)/unmarried | 1 weekback, protected | 7 month back to Nigeria | Fever, difficulty in swallowing | VP, erosions, crusted ulcers | genital erosion+ | + | B/L submandibular, inguinal | NR |
VP: Vesicopustules, LN: Lymphnodes, NR: non-reactive, B/L: Bilateral
MP is a rare disease caused by the monkeypox virus, genus orthopoxviridae. While the disease is endemic in Africa, in May 2022, it began spreading to non-African regions. In countries like India, where the MP disease was not reported earlier, the current outbreak is more likely linked to international travel to the affected areas.1 On 23 July 2022, the World Health Organization (WHO) declared MP “a public health emergency of international concern.”2 Currently, more than 100 countries have reported outbreaks of this disease.
India was the first country in southeast Asia to report MP in an adult male who had a history of travel to the Middle East. The patient had close contact with an MP-positive individual in the United Arab Emirates (UAE).3 About 10 days later, Delhi reported its first case (Case 1), and this patient had no recent history of international travel.4 While government health officials did not officially confirm community transmission of the disease in India at that time, it raised concerns about the possibility of local spread.
The disease primarily affects the adult population and begins with a prodrome of fever, lymphadenopathy, headache, malaise, chills, rigour, sore throat or cough. Skin manifestations typically appear within 1–3 days after the onset of fever, and these symptoms can persist for a duration of 2–4 weeks. The lesions usually start as macules on the face and then gradually spread centrifugally to the palm and soles. Scabs typically persist for around a week before falling off spontaneously. Upon healing, they may result in either hyperpigmented or hypopigmented atrophic or hypertrophic scars, occasionally leading to patchy alopecia, contracture, or deformities.5
Contrary to the classic centrifugal spread of rash in MP, we observed predominant clustering of lesions in the genital area. A similar finding was also observed by Thornhill et al.5, where sexual route was the most common mode of transmission of the disease in 95% of their cases. Noticeably, 97% of those patients were homosexual, 1% was heterosexual and 2% were bisexual.5 Another study detected MP DNA in the seminal fluid of 29 of 32 cases, although it remains unclear whether the DNA was capable of replication and further transmission.6 According to the United Kingdom Health Security Agency, sexual abstinence during the disease period and condom usage for 12 weeks after the scabs have fallen, are recommended precautions.7 In the present study, the patients denied any homosexual contact or history of contact with any suspected MP cases. However, it is important to note that the possibility of transmission through sexual contact cannot be entirely ruled out.
The patients were admitted for the purpose of isolation, confirmation of diagnosis and monitoring. All patients showed improvement with conservative treatment. Upon discharge, they were advised to use condoms for a duration of 8–12 weeks and scheduled for follow-up in the sexually transmitted infection (STI) clinic.
To conclude, the clustering of umbilicated crusted lesions over the genital area is an atypical presentation of MP disease. This raises a clinical suspicion of sexual route of transmission in the present case series, although patients denied homosexual contact, or contact with other confirmed cases of MP. In addition, the possible neurotropic nature of these viruses or their affinity for the genital region needs to be researched.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Recently spreading human monkeypox virus infection and its transmission during COVID-19 pandemic period: A travelers’ prospective. Travel Med Infect Dis. 2022;49:102398.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- WHO declared monkeypox a public-health emergency of international concern: A case for prevention rationale. Int J Surg Lond Engl. 2022;105:106850.
- [Google Scholar]
- Monkeypox in South-East Asia: Is an alarming bell for this region? Int J Surg Lond Engl. 2022;106:106917.
- [Google Scholar]
- Monkeypox: Current situation in India: An old virus, a new menace? Indian J Community Med Off Publ Indian Assoc Prev Soc Med. 2022;47:628-30.
- [Google Scholar]
- Monkeypox virus infection in humans across 16 countries. N Engl J Med. 2022;387:679-91.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiological, clinical and virological characteristics of four cases of monkeypox support transmission through sexual contact. Euro Surveill Bull Eur Sur Mal Transm Eur Commun Dis Bull. 2022;27
- [Google Scholar]
- Monkeypox claims new victims: The outbreak in men who have sex with men. Infect Dis Poverty. 2022;11:84.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





