Translate this page into:
Multifocal lupus vulgaris with involvement of palpebral conjunctiva
Correspondence Address:
Deep Anurag
Department of Dermatology, School of Tropical Medicine, 108, Chittaranjan Avenue, Kolkata - 700 073, West Bengal
India
| How to cite this article: Barua JK, Anurag D, Damji SA, Banerjee G. Multifocal lupus vulgaris with involvement of palpebral conjunctiva. Indian J Dermatol Venereol Leprol 2017;83:216-218 |
Sir,
Cutaneous tuberculosis constitutes about 1–2% of all tuberculosis cases.[1],[2] Lupus vulgaris is the most common type of cutaneous tuberculosis in India and represents a progressive form of the disease, occurring in individuals with a moderate to high degree of immunity. The lesions are usually solitary, but two or more sites may also be involved simultaneously. Rarely, mucosal involvement can also occur. The disease can manifest in a variety of morphological forms and unusual clinical presentations with the involvement of face, nose, conjunctiva and buttocks.[3],[4] One such case with the involvement of the face, eyelid and conjunctiva is reported here.
A 13-year-old girl presented to the Dermatology out-patient department, School of Tropical Medicine, Kolkata, with skin lesions present over the right side of the face, right eye and upper eyelid. The lesions were noticed around 6 months back as a solitary papule over the right cheek, which slowly enlarged and involved other areas too. The patient also complained of watering of eyes. She was treated with multiple antibiotics with little response.
Local examination revealed two well-circumscribed plaques - one over the right side of the face, in the parotid area and the other plaque over the right upper eyelid, extending to involve the ipsilateral bridge of the nose. The lesions had erythematous borders and adherent brown scales and crusts on the surface, with slight scarring. There was involvement of the upper palpebral conjunctiva of the right eye with conjunctival congestion and epiphora, leading to upper lid ectropion [Figure 1a] and [Figure 1b]. The lesions were non-tender on palpation and regional lymph nodes were not palpable. The patient did not recollect any history of trauma and there was no family history of tuberculosis. Hematological and biochemical investigations revealed no abnormalities. Chest X-ray was normal. Considering the possibilities of deep fungal infections and cutaneous tuberculosis, a skin biopsy was taken. Tissue histopathology showed noncaseating granulomatous infiltrates consisting of multiple Langhans type of giant cells, lymphocytes and epithelioid cells [Figure - 2]. Fungal cultures were negative. The Ziehl–Neelsen staining on tissue section was negative for acid-fast bacilli. Mantoux test was performed with five tuberculin units and was positive with an induration measuring 16 mm after 48 h.
 |
| Figure 1a: Lesion over the right side of face |
 |
| Figure 1b: Lesion involving the right eyelid and the conjunctiva |
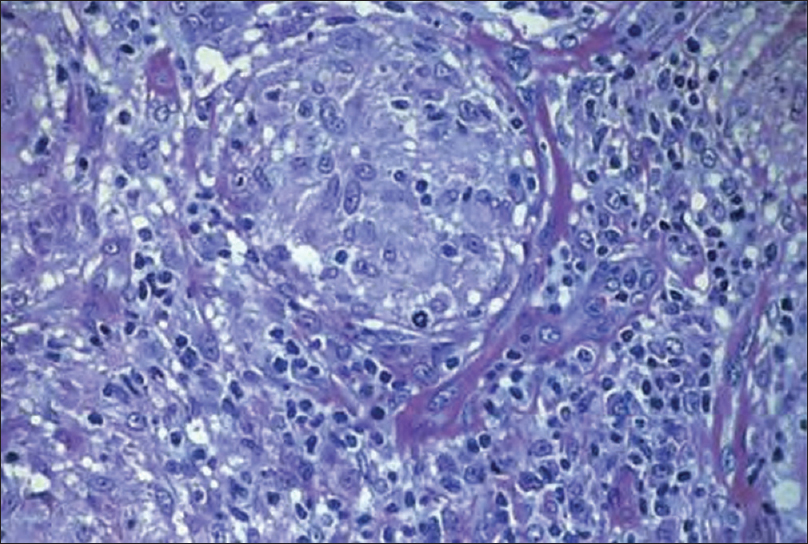 |
| Figure 2: Histopathological image showing non caseating granulomatous infiltrates consisting of multiple Langhans type of giant cells, lymphocytes and epithelioid cells (H and E, ×400) |
The patient was started on conventional, category I antitubercular therapy. For the right eye, lubricating eye drops and antibiotic eye ointment were prescribed. The lesions on the face healed with scarring [Figure - 3] by 6 months of treatment. Further, the patient was referred to the ophthalmology department for ectropion surgery.
 |
| Figure 3: Post treatment photograph showing healed lesion with scarring over right side of face and upper eyelid along with ectropion of right upper eyelid |
Lupus vulgaris usually is a post-primary lesion of the skin in a person who has been infected elsewhere with Mycobacterium tuberculosis.[5] Usually, the transmission is through contiguous, lymphatic or hematogenous routes. Rarely, it can appear at the site of the primary inoculation or at the site of a Bacillus Calmette–Guérin vaccination.[6] The disease may have different morphological types including plaque, ulcer, mutilating forms, vegetative and tumor-like lesions. Complications include scarring deformities such as ectropion and microstomia, requiring plastic surgery.
In our patient, the lesions present over the face were characteristic with the added involvement of the upper eyelid and the upper palpebral conjunctiva, resulting in ectropion of the eyelid. However, the extension of lesions to the eyelids and conjunctiva did not lead to any visual impairment. Such exceptional cases of facial lupus vulgaris with ocular involvement have been rarely reported earlier.[3],[4]
Diagnosis of cutaneous tuberculosis may often pose difficulties as the clinical appearance of the lesions may not always be characteristic. Demonstration of acid-fast bacilli may be difficult with the high immune status of the patient, as in our case. In tuberculosis, there is a granulomatous inflammatory reaction in which the granuloma shows central caseous necrosis which is diagnostic, but its absence may not rule out the diagnosis of tuberculosis. In this case too, there was no evidence of caseation necrosis in the biopsy specimen. The Mantoux test is positive in most cases, as in our case. The absolute criteria for the diagnosis of cutaneous tuberculosis include a positive culture of M. tuberculosis from the lesion or deoxyribonucleic acid amplification by polymerase chain reaction. However, the culture was negative and polymerase chain reaction could not be performed in our case. A therapeutic trial with antitubercular therapy is justified, if clinical suspicion is strong and the diagnosis can be made based on the therapeutic response.
Our case emphasizes the importance of early diagnosis and treatment to prevent complications of lupus vulgaris like ectropion, which develop with the involvement of the conjunctiva.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Bravo FG, Gotuzzo E. Cutaneous tuberculosis. Clin Dermatol 2007;25:173-80.
[Google Scholar]
|
| 2. |
Hernández Solis A, Herrera González NE, Cazarez F, Mercadillo Pérez P, Olivera Diaz HO, Escobar-Gutierrez A, et al. Skin biopsy: A pillar in the identification of cutaneous Mycobacterium tuberculosis infection. J Infect Dev Ctries 2012;6:626-31.
[Google Scholar]
|
| 3. |
Warin AP, Jones EW. Cutaneous tuberculosis of the nose with unusual clinical and histological features leading to a delay in the diagnosis. Clin Exp Dermatol 1977;2:235-42.
[Google Scholar]
|
| 4. |
Cook CD, Hainsworth M. Tuberculosis of the conjunctiva occurring in association with a neighbouring lupus vulgaris lesion. Br J Ophthalmol 1990;74:315-6.
[Google Scholar]
|
| 5. |
Sehgal VN, Jain MK, Srivastava G. Changing pattern of cutaneous tuberculosis. A prospective study. Int J Dermatol 1989;28:231-6.
[Google Scholar]
|
| 6. |
Marcoval J, Servitje O, Moreno A, Jucglà A, Peyrí J. Lupus vulgaris. Clinical, histopathologic, and bacteriologic study of 10 cases. J Am Acad Dermatol 1992;26 (3 Pt 2):404-7.
[Google Scholar]
|
Fulltext Views
3,666
PDF downloads
1,972





