Translate this page into:
Multiple cherry angiomas and pyogenic granuloma in a patient treated with ramucirumab and paclitaxel
Correspondence Address:
Ji-Hye Park
Department of Dermatology, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul 06351
Korea
| How to cite this article: Choi YH, Byun HJ, Lee JH, Park JH. Multiple cherry angiomas and pyogenic granuloma in a patient treated with ramucirumab and paclitaxel. Indian J Dermatol Venereol Leprol 2020;86:199-202 |
Sir,
Secondary neoplasm may develop as a side effect of chemotherapy.[1],[2],[3] Anticancer drugs reported to cause secondary neoplasm are mainly the classic chemotherapeutic agents, including alkylating agents, possibly caused by the effects of DNA damage and immunosuppression.[2] Recently, there have been reports that newer anticancer drugs, including targeted agents and checkpoint inhibitors, may induce secondary neoplasm, such as vemurafenib-induced squamous cell carcinoma and keratoacanthoma.[3] Ramucirumab, one of the newer anticancer drugs, is a fully-human monoclonal antibody targeting the extracellular domain of vascular endothelial growth factor receptor-2 (VEGFR-2) thereby blocking proangiogenic effects of vascular endothelial growth factor (VEGF).[1],[4],[5],[6] The drug is used for treatment of gastric, colorectal and non-small cell lung cancers.[1],[5],[6] We present a case of two different vascular lesions, cherry angioma and pyogenic granuloma, which occurred after treatment with the newer anticancer drug ramucirumab and classic chemotherapeutic agent paclitaxel.
A 40-year-old man presented with 8 mm sized, reddish, dome-shaped, bleeding nodule on the left parietal region of the scalp [Figure - 1]a. He also reported newly appeared multiple tiny erythematous papules on the face and the neck [Figure - 1]a and [Figure - 1]b. He had history of advanced gastric cancer with metastasis to the omentum, pelvic cavity, and transverse mesocolon treated with capecitabine combined with oxaliplatin. Four months later, due to progression of advanced gastric cancer, capecitabine and oxaliplatin were discontinued. Subsequently, the patient was treated with ramucirumab (8 mg/kg) every two weeks and paclitaxel (80 mg/m2) once a week. Four months after starting the changed regimen, he came to our clinic due to the development of lesions described above. for which he claimed no preceding trauma. We performed excisional biopsy on the scalp lesion. The histopathological findings showed dilated capillary vessel proliferation and lymphohistiocytic infiltration in the dermis with epidermal collarettes [Figure - 2]. The scalp mass was diagnosed as pyogenic granuloma, and multiple reddish papules on the face and the neck were clinically diagnosed as cherry angioma. He opted to treat the multiple cherry angiomas for cosmetic reasons and they were removed with carbon dioxide laser. Ramucirumab and paclitaxel was also discontinued due to progression of advanced gastric cancer. The patient was started on pembrolizumab after stopping ramucirumab. Four months after discontinuation of ramucirumab, there were no new lesions.
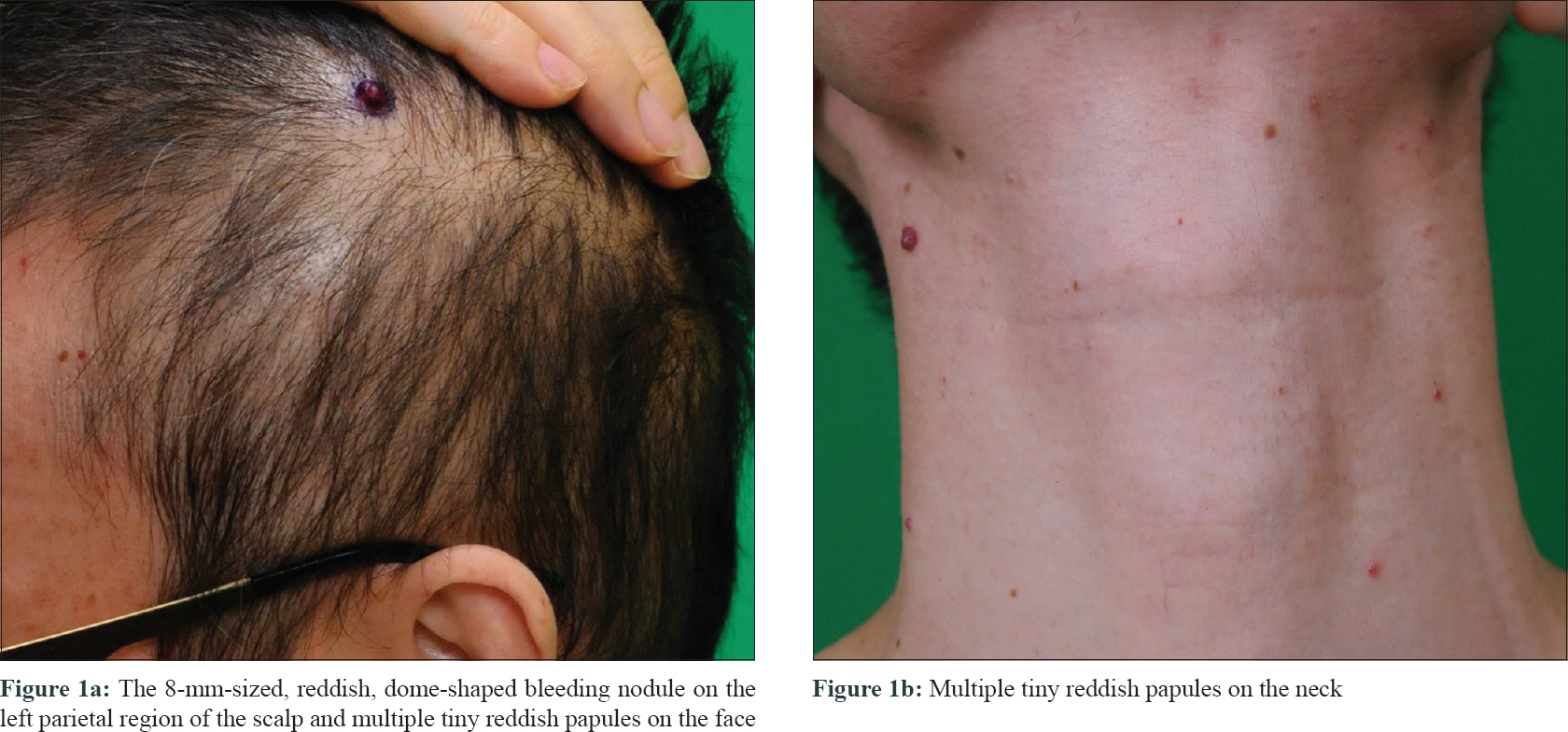 |
| Figure 1: |
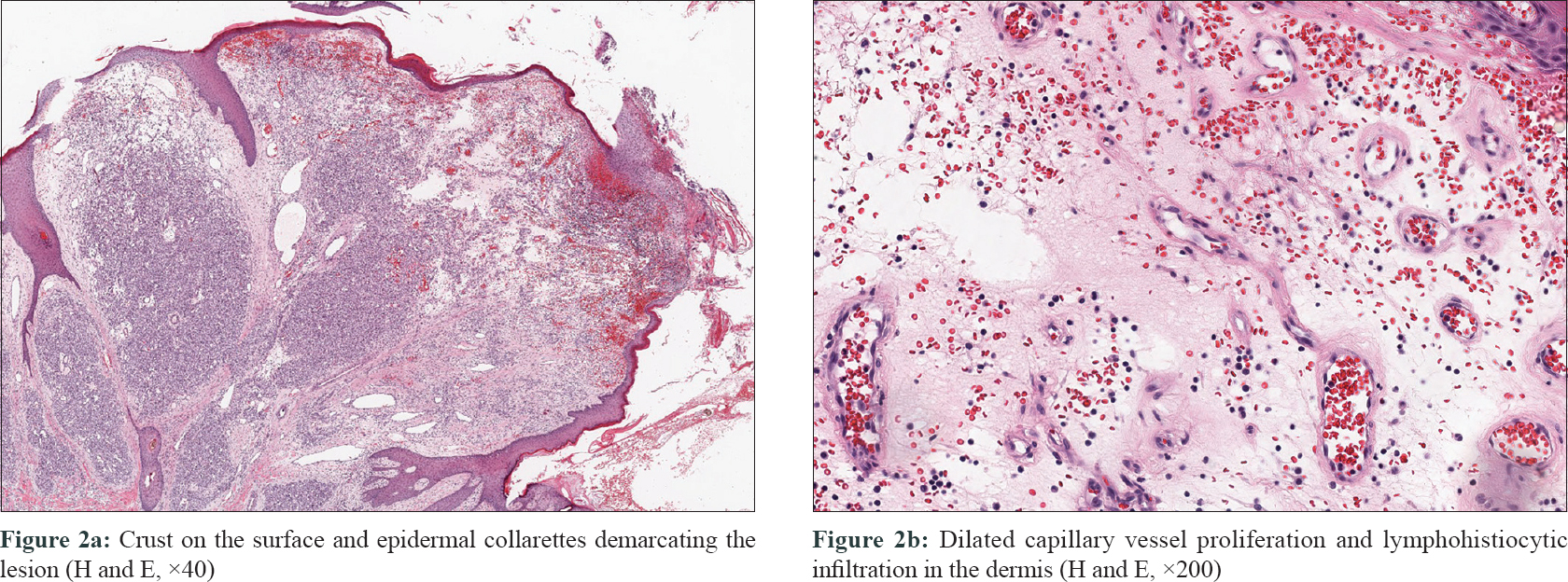 |
| Figure 2: |
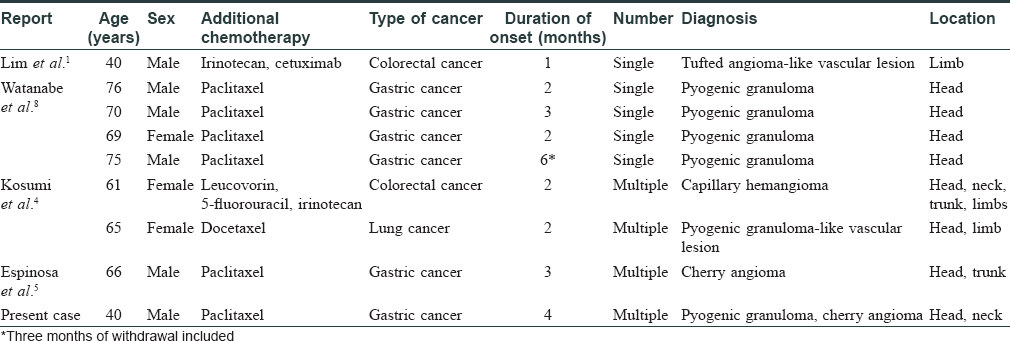
Angiogenesis is one of the hallmarks of cancer and therapies targeting angiogenesis are integral modalities in cancer treatment.[1],[7] As there is increased expression and secretion of the key angiogenesis regulators VEGF and VEGFR in cancers, several newer anticancer drugs inhibiting this pathway have been developed, one of them is ramucirumab.[1],[7] In the English literature, we found only eight cases which reported vascular lesions following treatment with ramucirumab [Table - 1].[1],[4],[5],[8] Seven of the nine cases reported ramucirumab treatment combined with taxanes.[4],[5],[8] In six of these seven cases, pyogenic granuloma-like vascular lesions developed, while eight cases showed vascular lesions on sun-exposed areas such as head and neck.[4],[5],[8]
Although the pathological mechanisms underlying development of vascular lesions by ramucirumab are unknown, somatic gene mutation and paradoxical angiogenesis have been suggested.[1],[7] Lim et al. reported that a single somatic VEGFR-2 precursor mutation, which has been reported in angiosarcoma, was identified in the vascular neoplasms induced by ramucirumab.[1] It is thought that disturbance of the VEGF axis, such as increased plasma levels of placental growth factor, VEGF-C, and VEGF-D in patients receiving the VEGF-A inhibitor bevacizumab or complementary enhancement of non-VEGF-mediated angiogenetic pathways involving fibroblast growth factors, contributes to development of vascular neoplasms.[1],[7]
In seven of the nine cases, ramucirumab was used in combination with taxanes.[4],[5],[8] Paclitaxel has been reported to cause periungual pyogenic granuloma and may inhibit functional cytoskeletons required for cell migration, proliferation, secretion, and capillary-like structure formation in angiogenesis by microtubule stabilization.[9] The researchers reported that pyogenic granuloma may be induced by an imbalance between inhibition of angiogenesis and other proangiogenic factors activated by paclitaxel.[9] Although the pathological mechanisms underlying the attribution of paclitaxel and ramucirumab in developing vascular lesions are unknown, changed pharmacokinetics of paclitaxel by VEGFR-2 inhibitor could be one of the mechanisms.[10] Steins et al. reported that a murine VEGFR-2 inhibitor showed systemic effects in decreasing vasculature in patient-derived xenograft mouse models. In addition, after the administration of paclitaxel, pharmacokinetics of paclitaxel was interfered in VEGFR-2-inhibitor-treated group compared with the control group. 10 As the VEGFR-2 inhibitor alters the pharmacokinetics of paclitaxel resulting in imbalance of angiogenic factors, angiomas and pyogenic granuloma-like vascular lesions have developed in cases treated with ramucirumab combined with taxane.
Furthermore, in eight of the nine cases, vascular lesions developed on the head or the neck.[4],[5],[8] Yano et al. reported that ultraviolet radiation may induce angiogenesis by upregulation of VEGF and downregulation of the endogenous angiogenesis inhibitor thrombospondin-1.[11] We believe that ultraviolet exposure might have contributed to the development of vascular lesions on sun-exposed areas.[11]
Therefore, we suggest that clinicians should be aware of the potential development of various vascular lesions especially on the head and the neck when opting for combination therapy with ramucirumab and taxane.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
| 1. |
Lim YH, Odell ID, Ko CJ, Choate KA. Somatic p.T771R KDR (VEGFR2) mutation arising in a sporadic angioma during ramucirumab therapy. JAMA Dermatol 2015;151:1240-3.
[Google Scholar]
|
| 2. |
Boffetta P, Kaldor JM. Secondary malignancies following cancer chemotherapy. Acta Oncol 1994;33:591-8.
[Google Scholar]
|
| 3. |
Su F, Viros A, Milagre C, Trunzer K, Bollag G, Spleiss O, et al. RAS mutations in cutaneous squamous-cell carcinomas in patients treated with BRAF inhibitors. N Engl J Med 2012;366:207-15.
[Google Scholar]
|
| 4. |
Kosumi H, Nishie W, Sugai T, Toyonaga E, Yoshimoto N, Nakamura H, et al. Ramucirumab-induced multiple haemangiomas of the skin: Two case reports. Acta Derm Venereol 2018;98:454-5.
[Google Scholar]
|
| 5. |
Espinosa Lara P, Medina-Puente C, Riquelme Oliveira A, Jiménez-Reyes J. Eruptive cherry angiomas developing in a patient treated with ramucirumab. Acta Oncol 2018;57:709-11.
[Google Scholar]
|
| 6. |
Vennepureddy A, Singh P, Rastogi R, Atallah JP, Terjanian T. Evolution of ramucirumab in the treatment of cancer – A review of literature. J Oncol Pharm Pract 2017;23:525-39.
[Google Scholar]
|
| 7. |
Clarke JM, Hurwitz HI. Understanding and targeting resistance to anti-angiogenic therapies. J Gastrointest Oncol 2013;4:253-63.
[Google Scholar]
|
| 8. |
Watanabe R, Nakano E, Kawazoe A, Kuboki Y, Bando H, Shitara K, et al. Four cases of paradoxical cephalocervical pyogenic granuloma during treatment with paclitaxel and ramucirumab. J Dermatol 2019;46:e178-80.
[Google Scholar]
|
| 9. |
Paul LJ, Cohen PR. Paclitaxel-associated subungual pyogenic granuloma: Report in a patient with breast cancer receiving paclitaxel and review of drug-induced pyogenic granulomas adjacent to and beneath the nail. J Drugs Dermatol 2012;11:262-8.
[Google Scholar]
|
| 10. |
Steins A, Ebbing EA, Pistorius MC, Waasdorp C, Krishnadath KK, Medema JP, et al. Systemic effects of angiogenesis inhibition alter pharmacokinetics and intratumoral delivery of nab-paclitaxel. Drug Deliv 2017;24:1801-10.
[Google Scholar]
|
| 11. |
Yano K, Kadoya K, Kajiya K, Hong YK, Detmar M. Ultraviolet B irradiation of human skin induces an angiogenic switch that is mediated by upregulation of vascular endothelial growth factor and by downregulation of thrombospondin-1. Br J Dermatol 2005;152:115-21.
[Google Scholar]
|
Fulltext Views
6,110
PDF downloads
3,448





