Translate this page into:
Multiple grouped nodules around the right ear in a young male
Correspondence Address:
Lalit Kumar Gupta
A-3, SaiVilla, Opp. Head Post Office, Madhuvan, Udaipur - 313 001, Rajasthan
India
| How to cite this article: Gupta LK, Bansal N K. Multiple grouped nodules around the right ear in a young male. Indian J Dermatol Venereol Leprol 2011;77:399-401 |
An 18-year-old male presented with a 3-year history of multiple, asymptomatic, smooth, dome-shaped, dull erythematous to bluish compressible, soft, papulo-nodular lesions of 5-25 mm size, grouped in and around the right ear [Figure - 1]. A few of the lesions were pedunculated. The overlying skin was intact. The lesions had developed spontaneously. General health of the patient was unaffected. There was no regional lymphadenopathy. Routine laboratory tests were normal. There was no peripheral eosinophilia. The IgE level was normal. Excision of the lesions attempted twice in the past led to recurrence within a period of about 2 months. Histopathological examination was performed [Figure - 2] and [Figure - 3].
 |
| Figure 1: Multiple smooth, dull red nodules, coalescent around the right ear |
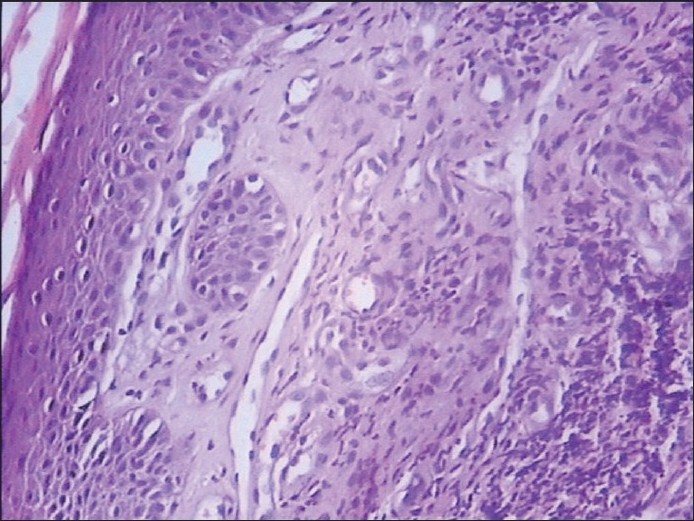 |
| Figure 2: Histology showing abundant proliferating blood vessels with prominent endothelial cells and dense lymphocytic infiltrate in the dermis (H and E, ×100) |
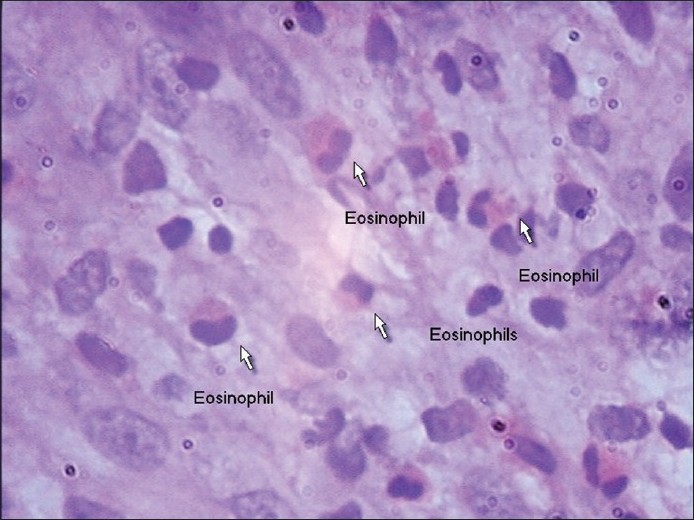 |
| Figure 3: Histology showing a fair number of eosinophils (H and E, ×400) |
What is your Diagnosis?
Diagnosis
Angiolymphoid hyperplasia with eosinophilia (ALHE)
Histopathology showed abundant proliferating, thick-walled blood vessels lined by prominent endothelial cells along with diffuse infiltration by lymphocytes [Figure - 2]. A fair number of eosinophils was also present [Figure - 3]. Lymphoid follicles with germinal centers were absent. There was no nuclear atypia, hyperchromasia or increased mitotic activity.
Discussion
ALHE (epithelioid hemangioma, pseudopyogenic granuloma) was first described in 1969 by Wells and Whimster, [1] who considered it to be a late stage of Kimura′s disease, described in the Japanese literature in 1948. There is a controversy whether Kimura′s disease and ALHE are variants of the same disorder or separate clinicopathological entities. It is now generally accepted that these are two separate entities. [2] In Kimura′s disease, the lesions occur in younger patients, are deep seated, are associated with lymphadenopathy, have no initial overlying skin lesions and do not contain epithelioid endothelial cells. [3] ALHE occurs in young to middle-aged adults, with a female preponderance. The index case was, however, male. ALHE typically presents as papules or nodules, tan, brown, pink or dull red in color, located predominantly in the head and neck region, especially around the ears and on the forehead and scalp. In one Indian report, the lesions occurred linearly in the left infrascapular region. [4] Most lesions are dermal in location, but some are subcutaneous. About half of the patients have multiple lesions, generally grouped in the same area. [5] The pathogenesis of ALHE is unknown, but it is considered to be a reactive phenomenon, possibly arising in response to or in association with an underlying vascular malformation. A history of trauma may be elicited in some cases. [6] Lesions are asymptomatic or can be painful, pruritic or pulsatile. [6] It is not accompanied by regional lymphadenopathy or elevated lgE levels. [7] Peripheral blood eosinophilia has been reported in approximately 20% of the patients. [8] One Indian report showed peripheral eosinophilia of 10%. [9]
Histologically, it appears as an angiomatous lesion with abundant proliferating blood vessels lined by prominent endothelial cells with a "histiocytoid" or "epitheloid" appearance and vacuolated cytoplasm. There is diffuse infiltration by lymphocytes and eosinophils, the eosinophils being less abundant than in Kimura′s disease. [7]
ALHE may resemble benign lymphoid hyperplasia, lymphoma cutis, sarcoidosis and richly vascularized metastatic tumors. Kimura′s disease has a tendency for more extensive lesions, often with involvement of salivary tissue and lymph nodes and much larger lymphoid follicles in histology. Angiosarcoma lacks the eosinophils and, cytologically, is more atypical and hemorrhagic. [5] Treatment of ALHE is dictated in part by the number, location and size of the lesions. Patients with solitary or a few small lesions may benefit from excision or Moh′s surgery. [8] A variety of other treatment modalities have been used with success, including systemic and intralesional steroid administration, interferon therapy, cryotherapy, laser therapy and topical application of tacrolimus. [8] There is an anecdotal report of response to imiquimod cream. [10]
| 1. |
Wells GC, Whimster IW. Subcutaneous angiolymphoid hyperplasia with eosinophilia. Br J Dermatol 1969;81:1-14.
[Google Scholar]
|
| 2. |
Googe PB, Harris NL, Mihm MC Jr. KImura's disease and angiolymphoid hyperplasia with eosinophila: Two distinct histopathological entities. J Cutan Pathol 1987;19:263-71.
[Google Scholar]
|
| 3. |
Fetsch JF, Weiss SW. Observations concerning the pathogenesis of epithelioid hemangioma/angiolymphoid hyperplasia. Mod Pathol 1991;4:449-55.
[Google Scholar]
|
| 4. |
Ramachandra BV, Suneetha C, Sunde. Angiolymphoid hyperplasia with eosinophilia. Indian J Dermatol Venereol Leprol 1994;60:45-6.
[Google Scholar]
|
| 5. |
North PE, Kincannon J. Vascular neoplasm and noeplastic - like proliferations. In: Bolgonia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2 nd ed. St. Louis: Mosby; 2008. p. 1774-6.
[Google Scholar]
|
| 6. |
Olsen TG, Helwig EB. Angiolymphoid hyperplasia with eosinophilia: A clinicopathologic study of 116 Patients. J Am Acad Dermatol 1985;12:781-96.
[Google Scholar]
|
| 7. |
Khandpur S, Raman M. Skin tumors. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3 rd ed. Mumbai: Bhalani Publishing House; 2008. p. 1520-1.
[Google Scholar]
|
| 8. |
Leiferman KM, Peters MS. Angiolymphoid hyperplasia with eosinophilia and Kimura disease. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's Dermatology in General Medicine. 7 th ed. New York: McGraw-Hill; 2008. p. 313-4.
th ed. New York: McGraw-Hill; 2008. p. 313-4.'>[Google Scholar]
|
| 9. |
Kumar JV, Guruprasad KY. Angiolymphoid hyperplasia with eosinophilia. Indian J Dermatol Venereol Leprol 1998;64:133-4.
[Google Scholar]
|
| 10. |
Gencoglan G, Karaca S, Ertekin B. Angiolymphoid hyperplasia with eosinophilia successfully treated with imiquimod. A case report. Dermatology 2007;215:233-5.
[Google Scholar]
|
Fulltext Views
2,518
PDF downloads
3,263





