Translate this page into:
Multiple subcutaneous abscesses: A rare presentation of cutaneous cryptococcosis
Correspondence Address:
Wanqing Liao
Department of Dermatology and Medical Mycology, Shanghai Key Laboratory of Molecular Medical Mycology Chang Zheng Hospital Second Military Medical University Shanghai 200433,
China
| How to cite this article: Pan B, Chen M, Jia H, Pan W, Liao W. Multiple subcutaneous abscesses: A rare presentation of cutaneous cryptococcosis. Indian J Dermatol Venereol Leprol 2013;79:118-119 |
Sir,
Cryptococcus neoformans is an opportunistic pathogen that mainly infects immunocompromised patients. The disease frequently involves the central nervous system and lung. Occasionally, skin may be the only apparent site of the infection. Cutaneous cryptococcosis can be caused by direct contact or via blood dissemination from the primary site of infection site. [1] The skin lesions may appear as nodules, ulcers, cellulitis, or molluscum contagiosum-like lesions. [2] We report a patient with chronic lymphocytic leukemia (CLL) with cryptococcosis presenting as subcutaneous abscesses, which were initially diagnosed as malignant neoplasms.
A 62-year-old man presented with a 3-week history of painless swellings over the right side of forehead, left elbow, and right side of chest wall. He denied prior trauma at the site of lesions. Additionally, he reported having fever and headache for 3 days. He was diagnosed with CLL 2 years back and had received 2 cycles of chemotherapy consisting of fludarabine and cyclophosphamide, followed by chlorambucil and prednisone. Physical examination identified a debilitated man with soft masses over the right side of forehead [Figure - 1]a, left elbow area [Figure - 1]b, and right chest wall [Figure - 1]c. There was no redness or pain. Neurological examination was normal. Laboratory data showed white blood cell count of 81.4 × 10 9 /L with 2% neutrophils, 98% lymphocytes. Renal and hepatic function tests were normal. Tests for HIV 1 and 2 antibodies were negative. A brain magnetic resonance imaging disclosed an osteolytic lesion in the right frontal bone. Chest X-ray revealed another osteolytic lesion in the 9 th rib (right side) and features of pneumonia.
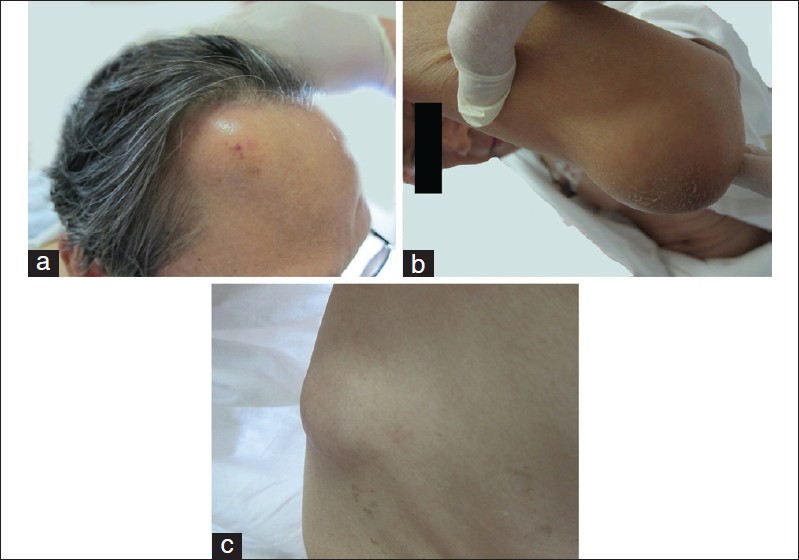 |
| Figure 1: (a) Soft, fluctuating mass at the right forehead nor redness or pain, sized by 4 cm × 4cm. (b) and (c) Nontender localized masses presented at left elbow and right chest wall with normal overlying skin, sized by 3 cm × 2 cm and 4 cm × 3 cm respectively. |
We thought of metastatic lesions at first as CLL patients are known to present ′second′ malignancies. However, skin biopsy (hematoxylin-eosin staining) only revealed granulomatous changes without malignant cells. Needle aspiration biopsy was also performed, and sticky hemorrhagic fluid was collected. Gram smear of the pus showed no bacteria. However, colonies of mucoid growth with creamy surface were noticed after 72 h on Sabouraud′s Agar Medium Cultures [Figure - 2]a. Microscopy of the colonies demonstrated budding yeast cells with capsule, and Cryptococcus was suspected. It was confirmed by the internal transcribed spacer region nucleotide sequencing. The sequence was submitted to GenBank (accession number JN603595) and demonstrated 99% identity with Cryptococcus neoformans var.grubii sequence (accession number AF356652). Aspirates were reexamined with India ink and revealed budding encapsulated yeasts [Figure - 2]b. Cryptococcal polysaccharide antigen in serum and cerebrospinal fluid (CSF) were positive at titers 1:1280 and 1:16, respectively. Blood and CSF cultures were negative. The patient was initially treated with intravenous amphotericin B deoxycholate 50 mg/d. However, his condition did not improve after 2 weeks treatment. Therefore, intravenous itraconazole 200 mg twice-daily was added, along with percutaneous drainage of the abscesses. After 8 weeks of therapy, his skin lesions had improved and serum cryptococcal antigen titer decreased to 1:320. The antifungal therapy was switched to oral fluconazole 400 mg/d for another 8 weeks. The patient continued to do well. No relapse was observed at one-year follow-up.
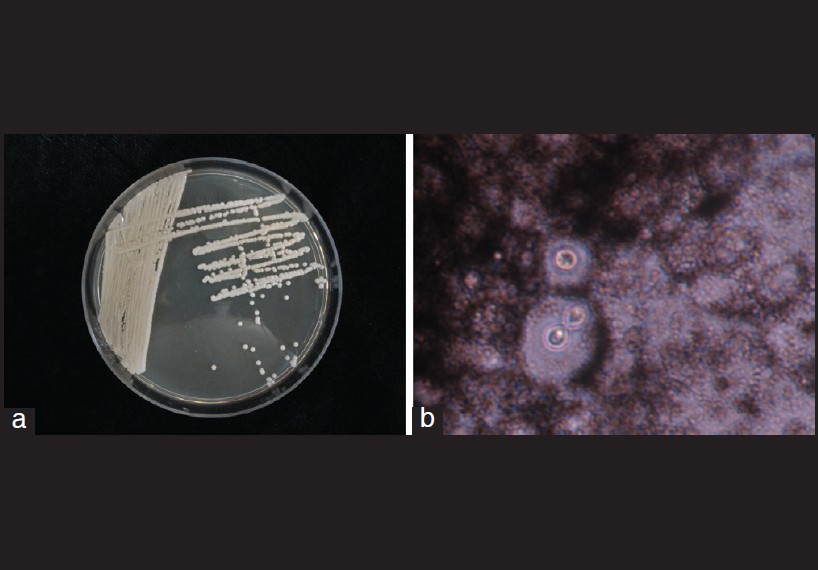 |
| Figure 2: (a) Colony of Cryptococcus neoformans arising from aspirates of subcutaneous abscess. (b) India ink examination of aspirates showed yeast-like cells with capsule appearing as clear halo surrounding |
The presence of multiple cutaneous masses with osteolytic lesions is an uncommon clinical feature of cryptococcosis, which may be confused with metastatic diseases, especially in patients with underlying malignancy. [3] This atypical presentation shares many characteristics with cryptococcal osteomyelitis. However, bone involvement occurs in less than 10% of disseminated cases, most of which had only one single site of bone involvement. [4] Preliminary diagnosis could be established by finding oval encapsulated yeast cells in the aspirates India ink stain. Our report indicates that patients with subcutaneous cryptococcal abscess should be thoroughly evaluated as it may be the first manifestation of a systemic disease.
According to the Infectious Diseases Society of America (IDSA) guideline, recommended treatment regimen for disseminated cryptococcosis in non-HIV patients is amphotericin B-based combination therapy with flucytosine for induction therapy followed by fluconazole consolidation and maintenance therapy. [5] Because patients with hematological disorders are particularly likely to develop bone-marrow depression after flucytosine treatment. [6] This drug was not used in our patient. The present patient was cured by amphotericin B followed by itraconazole and fluconazole. Although itraconazole does not penetrate well into the CSF, its concentration is significantly high in skin, fat, muscle and bone and higher in pathological tissues than in non-pathological tissues. [7] Our case demonstrates a disseminated cryptococcosis clinically mimicking metastatic malignancies in a patient suffering from CLL. Therefore, cryptococcosis has to be investigated as a differential diagnosis in patients with malignancy with cutaneous lesions.
| 1. |
Neuville S, Dromer F, Morin O, Dupont B, Ronin O, Lortholary O. Primary cutaneous cryptococcosis: A distinct clinical entity. Clin Infect Dis 2003;36:337-47.
[Google Scholar]
|
| 2. |
Langewar DN, Shroff HJ, Kohli MA, Hira SK. Cutaneous cryptococcosis and molluscum contagiosum occurring in the same lesion in a patient with AIDS. Indian J Dermatol Venereol Leprol 1998;64:25-8.
[Google Scholar]
|
| 3. |
Plaza JA, Perez-Montiel D, Mayerson J, Morrison C, Suster S. Metastases to soft tissue: A review of 118 cases over a 30-year period. Cancer 2008;112:193-203.
[Google Scholar]
|
| 4. |
Al-Tawfiq JA, Ghandour J. Cryptococcus neoformans abscess and osteomyelitis in an immunocompetent patient with tuberculous lymphadenitis. Infection 2007;35:377-82.
[Google Scholar]
|
| 5. |
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis 2010;50:291-322.
[Google Scholar]
|
| 6. |
Vermes A, Guchelaar HJ, Dankert J. Flucytosine: A review of its pharmacology, clinical indications, pharmacokinetics, toxicity and drug interactions. J Antimicrob Chemother 2000;46:171-9.
[Google Scholar]
|
| 7. |
Seishima M, Oyama Z, Oda M, Ishigo S. Distribution of an antifungal drug, itraconazole, in pathological and non-pathological tissues. Eur J Dermatol 2004;14:24-7.
[Google Scholar]
|
Fulltext Views
4,304
PDF downloads
2,066





