Translate this page into:
Multiple subcutaneous tender nodules in an adult male
Corresponding author: Dr. Sivaranjini R, Department of Dermatology & Sexually Transmitted Diseases, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. sivaranjini11@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agrawal A, Ramassamy S, Jinkala SR, Elango SR. Multiple subcutaneous tender nodules in an adult male. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_26_2025
A 38-year-old man presented with multiple painful skin lesions all over the body for the past one week. Lesions initially started on the bilateral lower limbs and later progressed to the trunk and upper limbs within the next few days. There was an associated history of intermittent fever and joint pain involving bilateral knee and ankle joints. There was no history of ulceration of skin lesions, abdominal pain, dyspnoea/cough, slippage of slippers, oral ulcers, photosensitivity, alcohol intake, previous abdominal surgeries, or any comorbidities. He was febrile on general examination with no pallor, icterus, or lymphadenopathy. Cutaneous examination revealed multiple erythematous tender indurated nodules on the trunk [Figure 1a] and bilateral upper and lower limbs [Figure 1b]. Systemic and nerve examinations did not reveal any positive findings. Laboratory investigations showed anaemia, leukocytosis (27,810/μL) with neutrophilia (90%), and elevated serum aspartate aminotransferase (159 U/L), amylase (950 U/L), and lipase (421.4 U/L) levels. Erythrocyte sedimentation rate (120 mm/hr) and C-reactive protein (4.8 mg/dl) were also elevated. Histopathology revealed predominantly lobular panniculitis [Figure 2a], showing distortion of the lobular architecture in the adipose tissue. Ghost-like adipocytes were seen [Figure 2b] with inflammatory infiltrate composed primarily of foamy macrophages and neutrophils. Areas of fat necrosis and saponification [Figure 2c] were also seen. Periodic acid- Schiff staining did not highlight any organisms. Ziehl-Neelsen staining for acid-fast bacilli, GeneXpert for M. tuberculosis, were negative. Repeated culture studies from both synovial fluid and blood did not show any growth of organisms. Computed tomography of the abdomen also did not reveal any significant findings. CA19-9 was within normal limits. An X-ray of bilateral knee joints showed periarticular hypodensities with soft tissue swelling suggestive of osteopenia and osteolytic changes [Figure 3a]. MRI of bilateral ankle joints showed multifocal osteonecrosis and periarticular cystic changes [Figure 3b].

- Multiple erythematous tender indurated nodules on the trunk.

- Multiple erythematous tender indurated nodules on the upper limb.
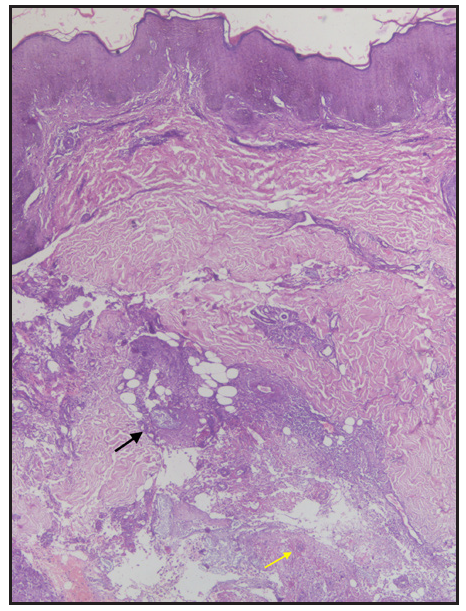
- Histopathology showing predominantly lobular panniculitis (Haematoxylin & eosin, 40x). Distortion of lobular architecture in the adipose tissue (black arrow) and ghost-like adipocytes (yellow arrow).
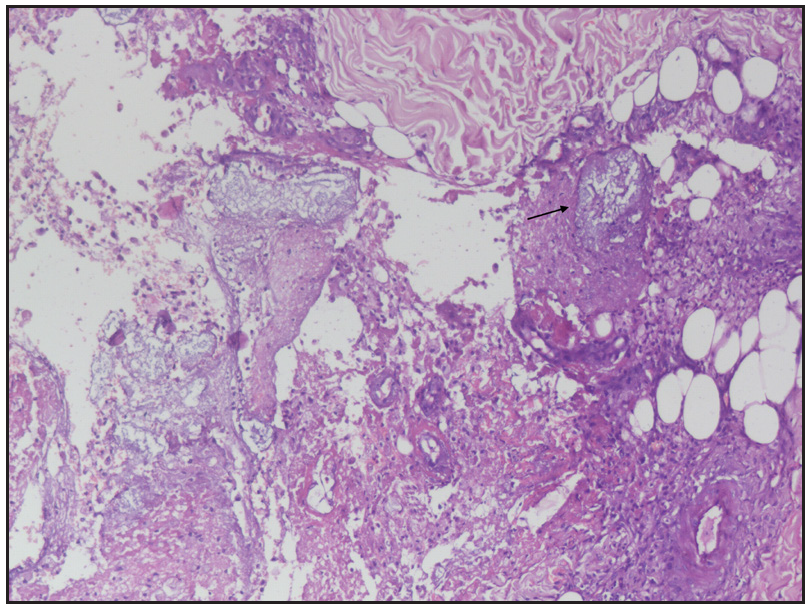
- Histopathology showing distortion of lobular architecture and saponification (black arrow) (Haematoxylin & eosin, 100x).
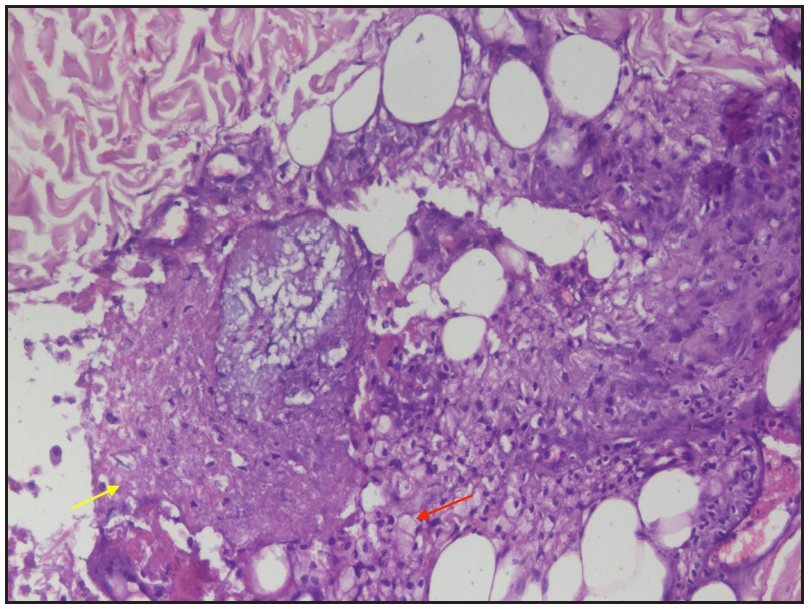
- Histopathology showing inflammatory infiltrate composed primarily of foamy macrophages (red arrow) and neutrophils and areas of fat necrosis (yellow arrow) (Haematoxylin & eosin, 200x).

- X-ray of bilateral knee joints showing periarticular hypodensities with soft tissue swelling suggestive of osteopenia and osteolytic changes.
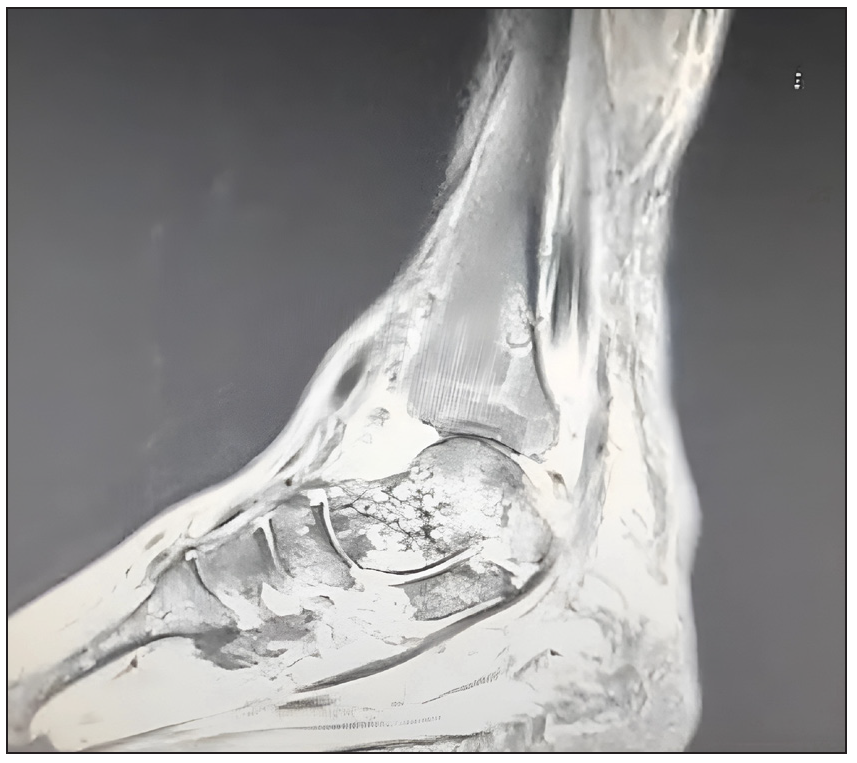
- MRI of ankle joint showing multifocal osteonecrosis and periarticular cystic changes.
Question
What is your diagnosis?
Answer
Diagnosis: Pancreatitis panniculitis and polyarthritis syndrome
Discussion
Pancreatitis panniculitis and polyarthritis syndrome is a rare entity characterised by the triad of painful nodules generally on the extremities, polyarthritis or oligoarthritis, and features of pancreatitis. It can cause diagnostic dilemmas and lead to high morbidity if not managed adequately.1
The pathophysiology of the pancreatitis, panniculitis and polyarthritis syndrome remains to be fully elucidated. It is hypothesised that the underlying pancreatic disease leads to the release of pancreatic enzymes, especially lipase, into the peripheral tissues resulting in fat necrosis and secondary inflammation in multiple sites, such as visceral organs, joints, and the skin.2 Pancreatic panniculitis develops in around 2 to 3 per cent of patients with underlying pancreatic disease. Clinically, patients with pancreatitis, panniculitis and polyarthritis syndrome present with subcutaneous erythematous nodules on the extremities, predominantly of the lower limbs (almost 98% of cases), and can also develop spontaneous ulcerations and oily sterile discharge. Our differential diagnosis for this case included erythema nodosum, sweet syndrome, erythema nodosum leprosum, and pancreatic panniculitis. Table 1 elucidates the clinical and histopathological differences among these entities. Polyarthritis is more commonly polyarticular (74%) and symmetrical (68%) and involves the ankle joints most, followed by knee joints and joints of the upper limb. For one-fourth of patients with the triad of pancreatitis, panniculitis and polyarthritis syndrome, arthralgia is the leading symptom. Gastrointestinal symptoms are absent in 45.8% of patients, which may be one of the causes of delay in diagnosis. Among the various causative factors of pancreatic disease involved in pancreatitis, panniculitis and polyarthritis syndrome, acute pancreatitis is the most frequent (54.2% of patients), followed by chronic pancreatitis and pancreatic malignancy including disorders like pancreatic neuroendocrine tumours and pancreatic-type acinar cell carcinoma.3
| Differentials | Clinical features | Histopathological features |
|---|---|---|
| Erythema nodosum | Acute onset of bilaterally symmetrical tender nodules commonly involving the shins, ankles, and knees usually associated with fever, joint pain, and headache | Primarily septal panniculitis without vasculitis, presence of Miescher’s radial granulomas, neutrophilic inflammatory infiltrate in early stage, granulomatous infiltrate with multinucleated giant cells |
| Sweet syndrome | Crops of painful, tender, erythematous, or violaceous nodules located more frequently on the lower limbs and associated with systemic symptoms | Predominantly lobular panniculitis without vasculitis, neutrophilic infiltrate that may present with leukocytoclasia involving lobules and septa |
| Erythema nodosum leprosum | Eruption of tender evanescent subcutaneous nodules associated with constitutional symptoms and features of Hansen’s disease | Predominantly lobular panniculitis with necrotising vasculitis, neutrophilic inflammatory infiltrate |
| Pancreatic panniculitis | Reddish-brown nodules around ankles and decubitus area, which may ulcerate and release oily discharge | Mostly neutrophilic lobular panniculitis with aggregates of ghost adipocytes that can become calcified. Ghost adipocytes lose their nuclei, and within their cytoplasm, they present a finely granular and amphophilic material as there is a saponification of the hydrolysed triacylglycerols. |
Histopathologically, pancreatic panniculitis seen in pancreatitis, panniculitis and polyarthritis syndrome shows lobular panniculitis without vasculitis and mostly neutrophilic infiltrate (as seen in our patient). Pancreatic panniculitis also shows liquefactive or enzymatic type of fat necrosis characterised by the complete destruction of the adipocyte cellular structure, ghost-like adipocytes, and saponification.4 Radiographic images classically feature multiple osteolytic lesions and, less commonly, features suggestive of periostitis, osteonecrosis, and fractures.5 Treatment of patients with pancreatitis, panniculitis and polyarthritis syndrome should be directed at the underlying pancreatic disease. The appropriate antibiotic coverage should be given to treat secondary infections, as they are very common and can cause sepsis. It is crucial to identify any anatomical abnormalities in the pancreas that may contribute to high levels of pancreatic enzymes, as they may need surgical intervention. Management of skin lesions and arthritis with corticosteroids and NSAIDs is usually ineffective and only provides symptomatic relief. Other anecdotal treatment options include subcutaneous octreotide and plasmapheresis.6 In our case, he was started on oral antibiotics and supportive management and underwent arthrotomy and lavage for knee and ankle joints with improvement in lesions within the next few weeks, and resolution of joint pain. Repeat amylase and lipase levels were within normal limits (69 U/L and 10 U/L, respectively).
Pancreatitis, panniculitis and polyarthritis is a rare syndrome that can have high mortality and morbidity due to uncontrolled pancreatic disease, sepsis, and/or bone necrosis leading to bone collapse. Since more than 50% of patients do not present with gastrointestinal complaints, pancreatitis, panniculitis and polyarthritis syndrome should be ruled out in patients presenting with fever, joint pain, and painful nodules. The delay in diagnosis of pancreatitis, panniculitis and polyarthritis syndrome can result in a poor prognosis for the patient. The prognosis is also closely linked to the underlying pancreatic disorder, with patients with acute pancreatitis having a mortality of around 16% compared with 25% for patients with chronic pancreatitis. The patients with pancreatic cancer also have a very poor prognosis. We wish to highlight the importance of the early diagnosis and treatment of pancreatitis, panniculitis and polyarthritis syndrome through this case report.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Pancreatitis, panniculitis, and polyarthritis syndrome with a fatal course. Ann Dermatol. 2022;34:83-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A case of pancreatitis, panniculitis and polyarthritis syndrome: Elucidating the pathophysiologic mechanisms of a rare condition. J Pediatr Surg Case Rep. 2015;3:223-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical characteristics, treatment, and outcome of pancreatitis, panniculitis, and polyarthritis syndrome: A case-based review. Clin Rheumatol. 2021;40:1625-33.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A practical approach to the clinico-pathological diagnosis of panniculitis. Diagn Histopathol. 2021;27:34-41.
- [Google Scholar]
- Board review vignette: PPP syndrome: Pancreatitis, panniculitis, polyarthritis. Am J Gastroenterol. 2017;112:1215-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pancreatitis, panniculitis, and polyarthritis. Semin Arthritis Rheum. 2010;39:417-23.
- [CrossRef] [PubMed] [Google Scholar]






