Translate this page into:
Multiple verruciform xanthomas following bone marrow transplant
2 Midwest Center for Dermatology and Cosmetic Surgery, Clinton Township, Michigan, USA
3 Ackerman Academy of Dermatopathology, New York, USA; Department of Dermatology, Kasr Al-Ainy University Hospital, Cairo University, Giza, Egypt,
Correspondence Address:
Zhiqiang Chen
Department of Dermatology, Guangdong Provincial Dermatology Hospital, No. 2, Lujing Road, Guangzhou, 510091
China
| How to cite this article: Xue R, Su W, Pei X, Huang L, Elbendary A, Chen Z. Multiple verruciform xanthomas following bone marrow transplant. Indian J Dermatol Venereol Leprol 2016;82:208-209 |
Sir,
Verruciform xanthoma is a rare benign mucocutaneous lesion which was first described by Shafer in 1971. [1] It usually presents as an asymptomatic, white or yellowish red plaque with a verrucous surface. However, polypoid, papillomatous and sessile lesions have also been reported. The condition has a predilection for the oral cavity. [1] Extraoral lesions have been reported, mainly involving the anogenital region. [2] Multiple lesions are extremely rare. Verruciform xanthoma has been reported in patients of bone marrow transplant who have graft versus host disease. [3] Though single lesions have been reported before, [4] we were unable to find any previous reports in the English literature of multiple verruciform xanthomas following bone marrow transplant, in the absence of graft versus host disease,
A 40-year-old man was evaluated for asymptomatic verrucous plaques on the upper gingiva and adjoining labial mucosa, and glans penis for 3 months. The lesions were slowly progressive. He had undergone allogenic bone marrow transplantation for chronic myeloid leukemia a year before the appearance of the lesions. The patient had received cyclosporine prophylaxis for graft versus host disease and was in complete hematological remission. Physical examination revealed a well demarcated, non-tender, pink to yellowish plaque with a verrucous surface, measuring 5 cm × 3 cm on the upper gingival mucosa, above the right incisor and canine and extending into the adjoining upper labial mucosa. Another yellowish sessile plaque measuring 3 cm × 2 cm was present on the glans penis [Figure - 1]a and b. A differential diagnosis of condyloma acuminata was considered. Biopsy from both the lesions revealed stratified squamous epithelium with papillary proliferation, uniformly long bulbous rete ridges, areas of bright eosinophilic parakeratosis with neutrophilic exocytosis and a dense infiltrate of foamy macrophages in the papillary dermis [Figure - 2]a and b, confirming the diagnosis of verruciform xanthoma. A lipid profile was normal and polymerase chain reaction from the lesion was negative for human papillomavirus. The lesions were re-excised and topical imiquimod was applied to treat any possibility of a residual lesion.
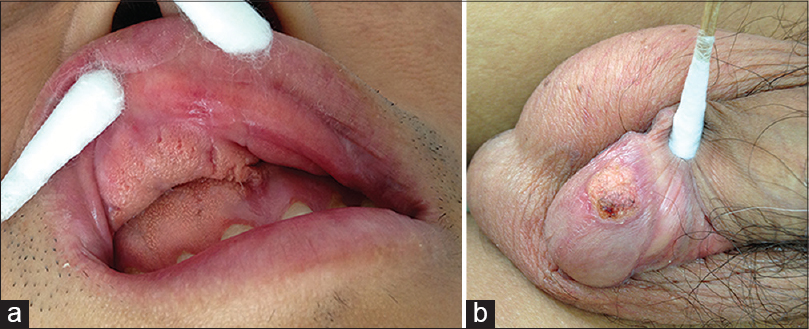 |
| Figure 1: Yellowish plaque with verrucous surface and sessile base, located on (a) upper gingival mucosa above the right incisor and canine and extending into the adjoining upper labial mucosa measuring 5 cm × 3 cm, (b) glans penis measuring 3 cm × 2 cm |
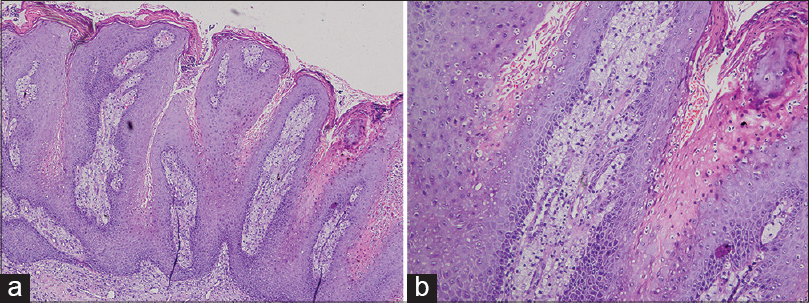 |
| Figure 2: (a) Exophytic growth, papillomatous and bright eosinophilic parakeratosis with neutrophils (H and E, ×100). (b) Brightly stained parakeratosis with neutrophils and foamy cells within the dermal papillae (H and E, ×200) |
The etiopathogenesis of verruciform xanthoma remains unclear. Postulated factors include immunologic factors, local inflammation and viral etiology. Ultrastructure and in situ hybridization from lesions of verruciform xanthoma have failed to demonstrate human papilloma virus making a viral etiology unlikely. [5] Immunologic factors were suggested based on the predominance of T-cell lymphocytes in the dermal infiltrate of verruciform xanthoma and a decreased number of Langerhans cells as compared to normal tissue. [5] A theory suggesting a role for a chronic inflammatory process in the development of verruciform xanthoma in patients with graft versus host disease proposed release of lipids from the phospholipid-rich cell membranes following epithelial tissue injury, which are engulfed by macrophages that later transform into foamy cells. [6] In our patient, presence of immunosuppression along with possible local irritation are probable factors involved in the pathogenesis of this disease.
The differential diagnosis of verruciform xanthoma includes warts, condyloma acuminate, squamous cell carcinoma and verrucous carcinoma. The diagnosis may be challenging, but the characteristic pathologic findings are diagnostic for this disease. It typically demonstrates papillomatous proliferation of the epidermis, bulbous rete ridges, bright eosinophilic parakeratosis with neutrophilic exocytosis and papillary dermal infiltration by foamy cells.
Treatment of verruciform xanthoma includes pulse dye laser, cryosurgery, electrocautery and surgical excision. Successful treatment with imiquimod is also reported. [7]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Shafer WG. Verruciform xanthoma. Oral Surg Oral Med Oral Pathol 1971;31:784-9.
[Google Scholar]
|
| 2. |
Philipsen HP, Reichart PA, Takata T, Ogawa I. Verruciform xanthoma - Biological profile of 282 oral lesions based on a literature survey with nine new cases from Japan. Oral Oncol 2003;39:325-36.
[Google Scholar]
|
| 3. |
Sibaud V, Marit G, Deminière C, Campana F, Taieb A, Fricain JC. Multiple verruciform xanthomas of the oral mucosa associated with graft versus host disease. Ann Dermatol Venereol 2006;133:995-9.
[Google Scholar]
|
| 4. |
Allen CM, Kapoor N. Verruciform xanthoma in a bone marrow transplant recipient. Oral Surg Oral Med Oral Pathol 1993;75:591-4.
[Google Scholar]
|
| 5. |
Sah K, Kale AD, Hallikerimath S. Verruciform xanthoma: Report of two cases and review on pathogenesis. J Oral Maxillofac Pathol 2008;12:41-4.
[Google Scholar]
|
| 6. |
Shahrabi Farahani S, Treister NS, Khan Z, Woo SB. Oral verruciform xanthoma associated with chronic graft-versus-host disease: A report of five cases and a review of the literature. Head Neck Pathol 2011;5:193-8.
[Google Scholar]
|
| 7. |
Guo Y, Dang Y, Toyohara JP, Geng S. Successful treatment of verruciform xanthoma with imiquimod. J Am Acad Dermatol 2013;69:e184.
[Google Scholar]
|
Fulltext Views
2,860
PDF downloads
1,980





