Translate this page into:
Mycoplasma pneumoniae-induced rash and mucositis: A new entity
Corresponding author: Dr. Mouna Korbi, Department of Dermatology, Fattouma Bourguiba University Hospital, University Of Medicine, University of Monastir, Monastir, Tunisia. korbimouna68@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ben Rejeb B, Ben Hammouda B, Korbi M, Belhadjali H, Toumi A, Youssef M, et al. Mycoplasma pneumoniae-induced rash and mucositis: A new entity. Indian J Dermatol Venereol Leprol 2022;88:349-53.
Abstract
Mycoplasma pneumoniae is a well-known cause of community-acquired pneumonia, mostly associated with dermatological manifestations especially with mucosal involvement and targetoid cutaneous lesions. For many years, it was considered among the spectrum of erythema multiforme. Recently, some authors have recommended the creation of a new syndrome called “mycoplasma-induced rash and mucositis.” This new syndrome has distinct epidemiological, clinical and histological features making it different from drug-induced Stevens-Johnson syndrome, toxic epidermal necrosis and erythema multiforme. Herein, we report two patients with acute Mycoplasma pneumoniae respiratory tract infection presenting severe mucocutaneous lesions in accordance with this new syndrome.
Keywords
Erythema multiforme
mucositis
Mycoplasma pneumoniae
Stevens-Johnson syndrome
Introduction
Mycoplasma pneumoniae infection is associated with extrapulmonary complications including mucocutaneous eruptions with prominent mucosal involvement already documented in erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrosis.1 However, it seems that Mycoplasma pneumoniae infection has distinctive clinical, physiopathological and evolution outcomes, leading to a long-standing debate in literature. Recently, some authors have considered it as a new entity1-4 and they have proposed the term “mycoplasma-induced rash and mucositis.”1-4 Herein, we report two patients with acute Mycoplasma pneumoniae respiratory tract infection and severe mucocutaneous lesions which were difficult to classify within the spectrum of erythema multiforme or Stevens-Johnson syndrome and toxic epidermal necrosis.
Case Reports
The first case
A 17-year-old woman presented with a one day history of acute onset symptomatic skin lesions and erosions on the oral, genital and nasal mucosa. Over the preceding 3 days, she complained of red painful eyes, difficulty in swallowing and nonproductive cough. On physical examination, the patient was febrile. Lung auscultation revealed crackling and ophthalmological examination showed bilateral conjunctivitis [Figure 1a]. On dermatological examination, we found multiple “targetoid” lesions which were edematous, infiltrated and purplish with some central vesicles on the face, limbs, trunk and perineum [Figure 1b]. The Nikolsky sign was negative. The palms and soles were not affected. We noted severe ulcerative stomatitis with multiple, painful ulcers affecting entire lips [Figure 1c], the palatine mucosa extending to the pharyngeal cavity and genital mucosa. The skin affected was approximately 5% of the body surface area. The chest radiography showed interstitial opacities. Routine laboratory testing showed lymphopenia and high C-reactive protein level. Serology for Epstein Barr virus, cytomegalovirus, parvovirus B19 and human herpes simplex virus were negative. However, serology for Mycoplasma pneumoniae was positive (immunoglobin M and immunoglobin G enzyme-linked immunosorbent assay were positive). A skin biopsy demonstrated perivascular inflammatory infiltrate, predominantly lymphocytic in the superficial and middle dermis [Figure 2a]. Isolated basal necrotic keratinocytes without vacuolar interface dermatitis were noted [Figure 2b]. Mycoplasma-induced rash and mucositis was considered. Because of extensive ulcerative stomatitis and dysphagia, we opted for intravenous methylprednisolone (0.5 mg/kg/day) and oral levofloxacin, 500mg/day for 2 weeks. Topical corticosteroid (desonide (Loatop®)) was applied on the conjunctival and oral mucosae. After 17 days, complete recovery was noted. [Figure 3].
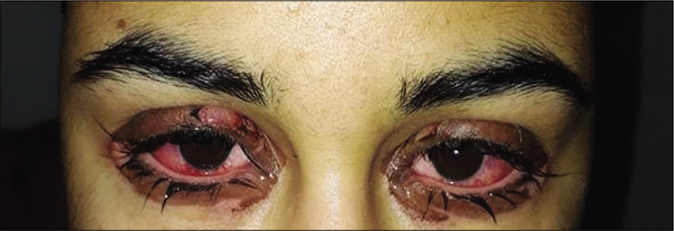
- Bilateral conjunctival hyperemia with discharge and blepharitis

- Atypical targetoid, an edematous and violaceous plaque with a central vesicle on the neck

- Confluent ulcers and scabs on the lips
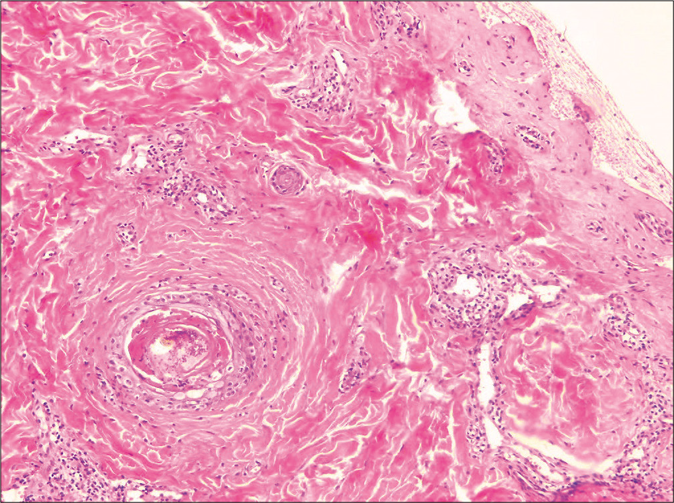
- Perivascular inflammatory infiltrate, predominantly lymphocytic, in the superficial and middle dermis (H and E, ×100) Children/young adolescents mean age=12
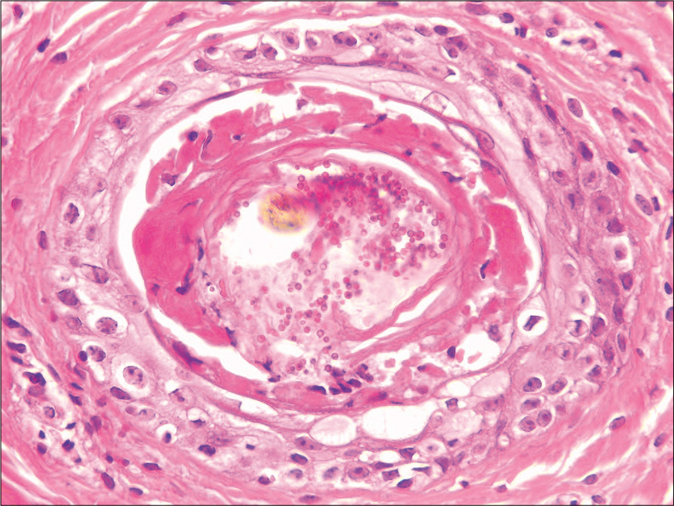
- Isolated basal necrotic keratinocytes without vacuolar interface dermatitis (H and E, ×400)

- Regressed lesions on lips after 2 weeks of treatment
The second case
A 10-year-old boy presented to the outpatient department with fever, cough, difficulty in swallowing and rapid onset of lesions on skin and mucosae evolving for 4 days. He did not receive any drugs and he did not report a history of cutaneous herpes infection. Dermatological examination revealed edematous reddish papules and plaques with central bulla/ vesicles, widespread on the face, trunk, limbs, palms and soles [Figure 4a]. Mucosal examination showed erosions, confluent ulcers and scabs on the lips [Figure 4b]. Genital examination showed targetoid lesions on the glans and scrotum. However, the conjunctival mucosa was not affected. About four per cent body surface involvement was noted. Auscultation revealed crackles and rales in the whole chest. Chest radiography detected bilateral alveolar-interstitial infiltrates. Complete blood cell count was within normal limits but c-reactive protein was high. The direct polymerase chain reaction in bronchial aspirate samples for Mycoplasma pneumoniae was positive. Serological testing for herpes simplex virus type 1 showed immunoglobin G positive and immunoglobin M negative. Serological testing for herpes simplex virus type 2 was negative. Skin biopsy revealed a subepidermal blister formation with necrotic keratinocytes and dense lichenoid infiltrate of lymphocytes occupied the widened papillary dermis [Figure 5]. Thus, the diagnosis of mycoplasma-induced rash and mucositis was established. Given the absence of swallowing difficulty, the patient was treated with only topical corticosteroid alongwith oral antibiotics (oral erythromycin 50 mg/kg/day used to treat infections due to atypical organism such as Mycoplasma pneumoniae) for 10 days. The child improved remarkably after 2 weeks of treatment.

- Edematous reddish plaques with central bulla, over left cheek

- Severe cheilitis with multiple erosions and scabs on the lips and mucosa
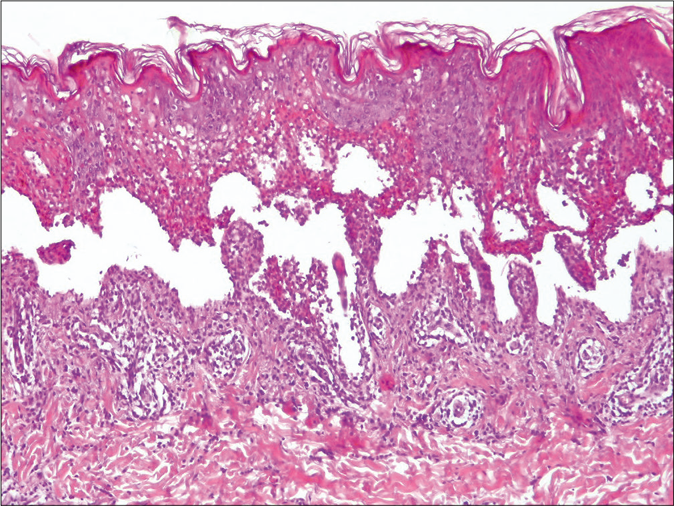
- Subepidermal blister formation (H and E, ×100)
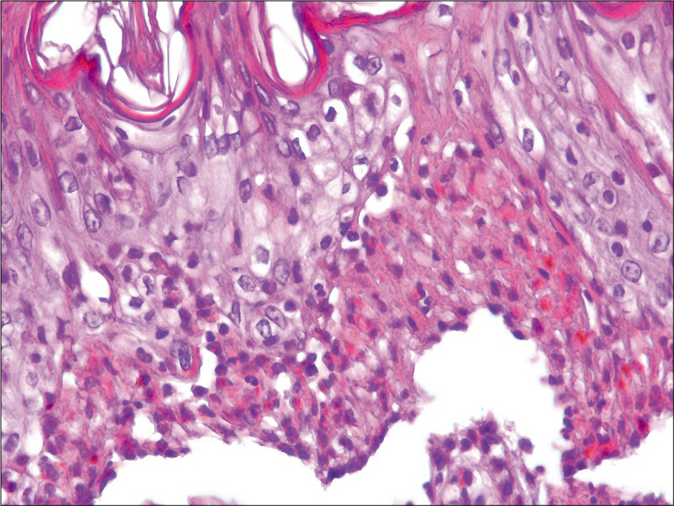
- Necrotic keratinocytes with full-thickness epithelial necrosis (H and E, ×400)
Discussion
Mycoplasma pneumoniae is a bacterial pathogen that typically causes community-acquired pneumonia.1 It is associated with mucocutaneous eruptions in almost 25% of patients mostly children and young adults.1 Skin lesions are characterized by severe mucositis with moderate cutaneous involvement. Recently, a study published by Canavan et al., based on epidemiological and clinical features of the 202 published cases of mucocutaneous lesions associated with Mycoplasma pneumoniae, suggested the creation of a new entity separate from the erythema multiforme.2 They proposed the term “mycoplasma-induced rash and mucositis.”2 In fact, their results showed a distinctive clinical presentation, in comparison with classical erythema multiforme.2 They reported male preponderance, frequent prodromal symptoms, severe and multiple mucosal involvement, a good response with corticosteroids and antibiotics treatment, minimal respiratory and ocular sequelae and a low rate of skin recurrences.2 Amode et al. in a comparative study investigated the differences between mycoplasma-induced rash and mucositis and erythema multiforme not associated with Mycoplasma pneumoniae.3 In accordance with our two reported cases, Amode et al. found that mycoplasma-induced rash and mucositis was characterized by occurrence of prodromal symptoms commonly preceding the rash, more common atypical targets with non-acral distribution, more multiple and severe mucosal involvements and a toxic epidermal necrosis-like histological pattern in skin biopsy.3
Their results were in agreement with recent publications.5-7 In fact, histopathologic features to mycoplasma-induced rash and mucositis still remain unclear. Erythema multiforme, Stevens-Johnson syndrome and mycoplasma-induced rash and mucositis have similar histopathologic features.3,5 These contain apoptotic keratinocytes and superficial dermal infiltrate with a sparse perivascular lymphocytes. Compared to mycoplasma-induced rash and mucositis, the dermal infiltrate is denser in Stevens-Johnson syndrome and more lichenoid in erythema multiforme.3,5-7 The histological findings of mycoplasma-induced rash and mucositis seem to be a mixture of Stevens-Johnson syndrome and erythema multiforme. Indeed, the pathogenic hypothesis differentiates between erythema multiforme or Stevens-Johnson syndrome/toxic epidermal necrosis and mycoplasma-induced rash and mucositis which is due to the production of immunoglobulins by proliferating clones of B-cells inducing an immune complexes depot in the skin in opposition with Stevens-Johnson syndrome/toxic epidermal necrosis or erythema multiforme caused by a type IV delayed hypersensitivity reaction and by Fas-ligand mediated cytotoxicity.4
Based on our case reports and the review of literature, we can deduce some particular features of this new syndrome which we have summarized in Table 1. Thus, we suggest specific criteria to establish the diagnosis of mycoplasma-induced rash and mucositis. As for the clinical criteria, young age of onset (median age: 12 years) and a history of an upper respiratory infection are characteristic. Clinical features are especially prominent mucositis (with at least two mucosal involvement), predominantly ulcerative and hemorrhagic oral mucosal involvement and atypical cutaneous targets. As for the histological findings, a toxic epidermal necrosis-like pattern is characteristic. An excellent response to systemic corticosteroids and oral antibiotics is considered as a suggestive criterion for the diagnosis, as in all the reported cases of mycoplasma-induced rash and mucositis. A positive Mycoplasma pneumoniae immunoglobulin M antibodies or positive polymerase chain reaction confirm the diagnosis of this syndrome.
| Features | EM | SSJ | MIRM |
|---|---|---|---|
| Gender | No differences between men and women | No differences between men and women | Male predominance (60%) |
| Age of disease onset (years) | Young adults Mean age=25 |
Adults Mean age=45 |
Children/young adolescents mean age=12 |
| Season onset | Autumn/winter | No particular season | Winter |
| Past herpes recurrent infection | ++ | +/− | − |
| Prodromal of respiratory symptoms | − | +/− | ++ |
| Atypical pneumonia | − | − | +++ |
| Acral distribution | +++ | +/− | +/− |
| Typical targets | ++ | +/− | +/− |
| Atypical targets | +/− | ++ | ++ |
| Bullae | +/− | ++ | +++ |
| Skin involvement (percentage BSA) | <10 | <10 | <10 |
| Mucosal involvement | Minimal+/− | Severe+++ | Severe++++ ≥2 mucosas |
| Histology | Hydropic degeneration of basal keratinocytes Spongiosis Apoptotic keratinocytes Moderate perivascular lymphocytic infiltrate |
More necrotic keratinocytes Denser dermal infiltrate Microscopic red blood cell extravasation |
Apoptotic keratinocytes Sparse perivascular dermal infiltrate TEN-like pattern |
| Etiology | HSV+++ | Drug-related++ | Mycoplasma pneumoniae |
| Treatment | Symptomatic | Systemic corticosteroids | Oral antibiotic and corticosteroid |
| Prognosis | Favorable (30% recurrence rate) | Mortality rate (5%) | Favorable (8% recurrence rate) |
| Sequelae | − | + Ocular synechiae Blindness Postinflammatory pigmentary changes |
+/− Ocular mucosal damage (8.9%) Corneal ulcerations and ocular synechiae Restrictive lung disease |
EM: erythema multiforme, SSJ: Stevens-Johnson syndrome, MIRM: mycoplasma-induced rash and mucositis, BSA: body surface area, HSV: herpes simplex virus, TEN: toxic epidermal necrosis,-:absent, +/-: rarely, +:present, ++/+++: frequent/very frequent
In conclusion, mycoplasma-induced rash and mucositis seems to have a distinctive presentation compared with other mucocutaneous eruptions characterized by a skin involvement less than 10% of the body surface area, suggestive involvement of at least two mucosal sites, atypical targets and evidence of Mycoplasma pneumoniae infection. Recognition of mycoplasma-induced rash and mucositis as an independent entity may lead to easier clinical diagnosis and better treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Erythema multiforme associated with Mycoplasma pneumoniae. Infection. 2014;42:797-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mycoplasma pneumoniae induced rash and mucositis as a syndrome distinct from Stevens Johnson syndrome and erythema multiforme: A systematic review. J Am Acad Dermatol. 2015;72:239-45.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and histologic features of Mycoplasma pneumoniae related erythema multiforme: A single center series of 33 cases compared with 100 cases induced by other causes. J Am Acad Dermatol. 2018;79:110-7.
- [CrossRef] [PubMed] [Google Scholar]
- Mycoplasma pneumoniae induced mucocutaneous rash: A new syndrome distinct from erythema multiforme? report of a new case and review of the literature. Actas Dermosifiliogr. 2016;107:e47-51.
- [CrossRef] [Google Scholar]
- Mycoplasma pneumoniae associated mucositis: A recently described entity. Eur J Case Rep Intern Med. 2018;5:0977.
- [CrossRef] [PubMed] [Google Scholar]
- Mycoplasma pneumonia induced mucositis without rash in an 11 year old boy. Clin Case Rep. 2018;6:551-52.
- [CrossRef] [PubMed] [Google Scholar]






