Translate this page into:
Mycosis fungoides with unusual vitiligo-like presentation
Correspondence Address:
Jayanta Kumar Das
BE 3, 193 Andul Road, Howrah - 711109, W.B
India
| How to cite this article: Das J, Gangopadhyay A. Mycosis fungoides with unusual vitiligo-like presentation. Indian J Dermatol Venereol Leprol 2004;70:304-306 |
Abstract
Mycosis fungoides (MF), the commonest variant of primary cutaneous T cell lymphoma (CTCL), is relatively uncommon among the Asians. Hypopigmented mycosis fungoides is a rare variant usually observed in dark-skinned individuals, especially children. Hypopigmented MF usually responds well to therapy, particularly to PUVA, and has a comparatively benign course. Mycosis fungoides in a 16-year-old boy, with extensive asymptomatic hypopigmented lesions developing gradually all over the body over eight years and vitiligo-like skin lesions developing for seven years, with no systemic features, is presented for its unusual clinical features and conspicuous histopathological findings of prominent epidermotropism. The case showed fairly good response to PUVASOL therapy.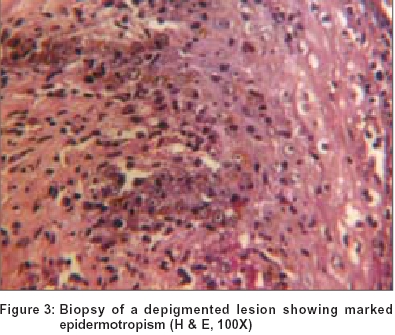 |
 |
 |
 |
 |
 |
INTRODUCTION
Mycosis fungoides is the commonest variant of primary CTCL and is generally associated with an indolent clinical course.[1] It is a neoplasm of mature helper T cells.[2] Although not very rare worldwide, it is commonest among Africans and relatively uncommon among Asians.[3]
The cutaneous lesions of MF typically progress through three stages: an early, erythematous, scaly patch stage with eczematous features; an infiltrated plaque stage; and a tumor stage.[2] In addition, a wide spectrum of cutaneous lesions has been described, rare manifestations being pustular, bullous, hyperpigmented, purpuric, follicular, and verrucous forms. Hypopigmented mycosis fungoides is a rare variant. It is usually observed in dark-skinned individuals, especially children and adolescents, although it has been reported in Caucasian patients.[1],[3],[4],[5]
CASE REPORT
A 16-year-old boy presented with a history of hypopigmented scaly patches developing gradually all over the body over the past eight years. Asymptomatic hypopigmented patches had first appeared on the trunk and were quickly followed by the appearance of new similar lesions on the proximal limbs. The lesions had gradually increased in size for a few months to assume their current dimensions, and then had remained more or less static. Two vitiligo-like, depigmented patches were noticed on the abdomen and the right thigh about seven years back; they had spread to assume their current size in one year. New hypopigmented as well as vitiligo-like lesions had continued to appear till the patient came to us. There was no history of systemic features such as fever, lassitude or weight loss.
On examination, there were many asymptomatic hypopigmented and a few vitiligo-like, depigmented oval and irregular, well-defined, atrophic patches 8 to 15 cm in diameter on the trunk and extremities. The patches showed a finely wrinkled slightly scaly surface. They were not indurated and there were no telangiectases. The vitiligo-like lesions were on the abdomen, right axilla and both thighs [Figure - 1] and [Figure - 2]. The largest such lesion was about 15 cm along the long axis. No lymphadenopathy was noted. General examination was unremarkable.
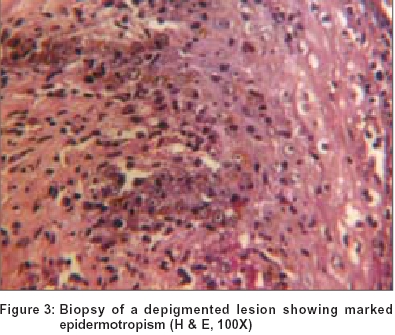
Histological examination of a vitiligo-like lesion on the abdomen showed an infiltrate of mononuclear cells at the interface with prominent epidermotropism, with lymphocytes cells lying singly as well as in groups [Figure - 3]. No atypical cells were seen. Hemogram, routine blood biochemistry, chest X-ray and urine analysis were normal. There were no atypical cells in the peripheral blood.
In view of the widespread atrophic patches the patient was put on PUVASOL. 8-methoxypsoralen (8-MOP) 30 mg (0.62 mg/kg, as the patient weighed 48 kg) was taken orally by the patient for three days a week at around 7 a.m. in the morning, after breakfast, followed after two hours by sun-exposure of the affected skin for 30 minutes. The skin lesions improved slowly and steadily, and after 6 months the depigmented lesions reduced by about 40% of their original size, and the hypopigmented lesion showed about 30% reduction in size. A few smaller hypopigmented lesions disappeared. Scaling was reduced, too.
DISCUSSION
Mycosis fungoides is a polymorphous skin disease. Hypopigmented mycosis fungoides is an uncommon variant with 113 cases having hypopigmented lesions either as the sole manifestation of the disease or presenting in association with erythematous patches having been reported.[4] Vitiligo-like lesions are rare. In 2000, Cribier, et al reported four cases of vitiligo with histologic features simulating MF, but it has been opined that these cases represented MF and not vitiligo.[4] Hypopigmented MF is overwhelmingly common in non-Caucasian races, with only 16 cases reported so far in Caucasians.[4] Compared to other clinical presentations of MF, the hypopigmented form is more prevalent in the younger age group, particularly in children.[1],[3],[4],[5]
Histopathologically, hypopigmented MF lacks epidermal atrophy and demonstrates moderate to marked exocytosis resembling pagetoid reticulosis.[6] In this regard the present case is typical. Hypopigmented MF often shows a T suppressor cell CD8 positive phenotype, although the CD4 positive phenotype has also been reported.[4] In this variant monoclonal proliferation of T lymphocytes, which is characteristic but not diagnostic of MF, has been found to be confined mainly to the epidermis.[4] These studies, however, could not be done in our patient due to lack of facilities.
The pathogenesis of hypopigmented MF is still unclear. Hypopigmentation may be due to the cytotoxic effect of T suppressor lymphocytes on melanocytes, at least in cases showing the CD8-positive phenotype, probably with the non-neoplastic CD8-positive lymphocytes playing a role. The pathomechanism may be similar to vitiligo, which Goudie in 1991 categorized as a ′benign cutaneous lymphoma′.[4] Hypopigmented MF is characterized by good response to therapy, particularly to PUVA, with a biologically benign course, although recurrences are common.[5] Our case was responding well to PUVASOL.
We administered 8-MOP at the dosage recommended for the clearing phase of PUVA in CTCL, but had to use the sun as the source of UVA due to non-compliance of the patient. The recommended treatment schedule of PUVA in CTCL is essentially the same as for psoriasis, with 8-MOP given at the dose of 0.6 mg to 0.8 mg/kg of body weight 1 to 3 hours before exposure[7]. The treatment consists of a clearing phase, a maintenance phase, and a follow-up phase without therapy. In the clearing phase treatment is given three times weekly, followed by maintenance therapy of two treatments per week for 1 month and one treatment per week for another month. Thereafter, therapy is discontinued and the patient is monitored. The patient is subjected to a full PUVA course in case of a relapse. PUVA therapy may induce long-lasting remission in early stages of CTCL, and a significant drop in death rate in patients of CTCL may be attributed to this therapy. [7]
The present case is reported for its rarity, particularly in the Indian literature, and for the unusual clinical and histopathological features, i.e. early age of onset, hypopigmented and vitiligo-like lesions, and pronounced epidermotropism.
| 1. |
MacKie RM. Cutaneous lymphomas and lymphocytic infiltrates. In: Champion RH, Burton JL, Burns DA, Breathnach SM. editors. Rook/ Wilkinson/ Ebling Textbook of Dermatology. Vol 1, 6th Ed. Oxford: Blackwell Science Ltd.; 1998. p. 2373-84.
[Google Scholar]
|
| 2. |
Lambroza E, Kohen SR, Phelps R, Lebwohl M, Braverman IM, DiCostanzo D. Hypopigmented variant of mycosis fungoides: Demography, histopathology, and treatment of seven cases. J Am Acad Dermatol 1995;32:987-93.
[Google Scholar]
|
| 3. |
Latkowski J, Heald P. Cutaneous T cell lymphoma. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Dermatology in General Medicine. 6th Ed. New York: McGraw-Hill; 2003:1537-58.
[Google Scholar]
|
| 4. |
Ardigo M, Borroni G, Muscardin L, Kerl H, Cerroni L. Hypopigmented mycosis fungoides in Caucasian patients: A clinicopathologic study of 7 cases. J Am Acad Dermatol 2003;49:264-70.
[Google Scholar]
|
| 5. |
Akaraphanth R, Douglass MC, Lim HW. Hypopigmented mycosis fungoides: Treatment and 6.5 year follow-up of 9 patients. J Am Acad Dermatol 2000;42:33-9.
[Google Scholar]
|
| 6. |
Ortonne J, Bahadoran P, Fitzpatrick TB, Mosher DB, Yashiaki H. Hypomelanoses and hypermelanoses. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Dermatology in General Medicine. 6th Ed. New York: McGraw-Hill; 2003:836-81.
[Google Scholar]
|
| 7. |
Honigsmann H, Szeimies R, Knobler R, Fitzpatrick TB, Pathak MA, Wolff K. Photochemotherapy and photodynamic therapy. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Dermatology in General Medicine. 6th Ed. New York: McGraw-Hill; 2003:2477-93.
[Google Scholar]
|
Fulltext Views
3,189
PDF downloads
1,812





