Translate this page into:
Nail fold dermoscopy in collagen vascular disorders: A cross-sectional study
Correspondence Address:
Parul Chojer
H. No. 119 Phulkian Enclave, Patiala, Punjab
India
| How to cite this article: Chojer P, Mahajan B B. Nail fold dermoscopy in collagen vascular disorders: A cross-sectional study. Indian J Dermatol Venereol Leprol 2019;85:439 |
Abstract
Background: The collagen vascular disorders, particularly systemic sclerosis, dermatomyositis, systemic lupus erythematosus and mixed connective tissue disorder, are often characterized by microangiopathic abnormalities of the nail folds. Nail fold dermoscopy is a well-established technique to assess these vascular changes.
Aims: To evaluate finger nail capillary vascular abnormalities by dermoscopy and their correlation with cutaneous and systemic involvement in the patients of collagen vascular disorders.
Methods: This was a cross-sectional study involving patients of collagen vascular disorders presenting to Government Medical College, Amritsar over a period of 2 years. Nail fold dermoscopy was done in these patients and correlated with cutaneous and systemic involvement. Statistical analysis was done using SPSS 17.0 version.
Results: A total of 30 patients were enrolled in the study. Sixteen (53.3%), 11 (36.7%) and 3 (10%) patients of systemic sclerosis, systemic lupus erythematosus and mixed connective tissue disorder, respectively were included for nail fold dermoscopy. The commonest change recorded in our study was dilated capillaries in 21 (70%) patients, followed by capillary dropouts in 17 (56.7%) patients and avascular areas in 16 (53.3%) patients. Of 17 patients presenting with sclerodactyly, active, early and late patterns were seen in 7 (41.2%), 2 (11.8%) and 7 (41.2%) patients, respectively. Out of 13 patients with respiratory involvement, active, early and late patterns were seen in 1, 1 and 7 (53.8%) patients, respectively (P value = 0.004).
Limitations: Owing to lesser number of patients in our study, it is difficult to draw conclusive recommendations, and more studies with a larger sample size are required.
Conclusion: Dermoscopy is a valuable tool not only to diagnose collagen vascular disorders but also for prognostication by correlating with systemic involvement.
Introduction
The collagen vascular diseases include a spectrum of disorders having certain features which are common, i.e. existence of autoimmunity in the form of antibody production or disordered cell-mediated immunity, vascular abnormalities, arthritis or arthralgia and skin disease. Vascular changes characterized by functional and structural abnormalities of the microcirculation play a central role in the pathogenesis of collagen vascular disorders. Nail fold capillaroscopy is a simple, noninvasive, inexpensive and useful tool for the study of microvasculature.[1],[2] So far, the gold standard for performing nail fold capillaroscopy has been nail fold videocapillaroscopy, which requires special equipment, is relatively expensive, time-consuming and not easily portable. Among the alternatives available to study the microcirculation, a handheld dermoscope is an easily available, inexpensive tool which is easy to learn and use. Dermoscopy is a noninvasive, repeatable bed-side investigation that shows minute details of skin lesions, thus making it a valuable tool in clinical dermatology, both for diagnosis and monitoring of skin diseases.
Nail fold capillaroscopy has been extensively studied in collagen vascular disorders, particularly systemic sclerosis. It provides information about the disease severity and degree of visceralization in the patients with systemic sclerosis. In this study we attempted to use it for studying microvascular changes in the proximal nail folds in patients of collagen vascular disorders. These changes were then correlated with the cutaneous and visceral involvement and thus, the severity of the disease.
Methods
This cross-sectional study was carried out in Government Medical College, Amritsar and attached Guru Nanak Dev Hospital, Amritsar over a period of 2 years. Patients of collagen vascular disorders presenting to Department of Dermatology and referred from other departments attached to Medical College were enrolled. Approval was taken from institution and ethics committee. After assessing for eligibility, a total of 30 patients of either sex aged >15 years, diagnosed on the basis of clinical criteria for specific collagen vascular disorders were included. Cases with psoriatic nail changes, onychomycosis and periungual eczematization were excluded from the study. Detailed history of the patient was taken; clinical examination, routine and other relevant investigations, including serology, skin biopsy, pulmonary function tests, high-resolution computed tomography of the chest, barium studies, renal function tests, 24 h urine protein, electrocardiogram, etc., were carried out and recorded in a pre-structured proforma. These changes were then correlated with nail fold capillaroscopic patterns.
The capillaroscopic pattern in systemic sclerosis was first described by Maricq et al. (1980) and is known as the “scleroderma type” capillaroscopic pattern.[3],[4],[5],[6],[7],[8],[9],[10],[11] This specific nail fold capillaroscopic pattern is found in a number of cases with overt scleroderma (83–93%).[6],[7]
The various nail fold capillary patterns described in scleroderma are as follows:[5]
- Early pattern: Appearance of few dilated and/or giant capillaries and a few hemorrhages. Distribution is relatively preserved without loss of capillaries.
- Active pattern: Large number of giant capillaries and hemorrhages. Moderate loss of capillaries, slight derangement and diffuse pericapillary edema can be found.
- Late pattern: Severe loss of capillaries with extensive avascular areas.
Bushy and ramified capillaries, or more than one capillary loops in a dermal papilla are the morphological substrates of defective neoangiogenesis.
Maricq et al. also observed that some of the parameters of this pattern can also be observed in other scleroderma spectrum disorders such as mixed connective tissue disorder, undifferentiated connective tissue disease, dermatomyositis/polymyositis and overlap syndromes. They defined these findings as scleroderma-like capillaroscopic pattern.[3],[4],[6],[8],[12],[13],[14],[15],[16]
Nail fold dermoscopy was done using a handheld dermoscope, i.e. Handyscope by German company FotoFinder systems launched in 2010 attached to i-phone and ultrasound gel. The easy-to-use slide-in mechanism ensures tight fit, and the handyscope lens system comes exactly in front of camera for outstanding pictures. It gives an optical magnification of up to 20× with the quality of auto-focus and presence of several lenses. With its unique twin light system and six polarized and six white light-emitting diodes, the handyscope combines the advantages of cross-polarized light and immersion fluid dermoscopy. The nailfold dermoscopy was done after the patients were made to sit for 15 min at an ambient temperature. Ultrasound gel was placed on the cuticle, nail plate and nail folds of the fingers to be evaluated. The periungual region of the eight fingers (excluding the thumbs) was examined. Dermoscope attached to i-phone was placed over nail plate followed by nail fold (proximal and lateral). All the changes on the nail folds were recorded and photographically evaluated. Images were stored in JPEG/PNG format and correlated with the cutaneous and systemic involvement. The statistical analysis was done with Chi-square test using SPSS 17.0 version.
Results
A total of 30 patients were enrolled in the study with 16 (53.3%), 11 (36.7%) and 3 (10%) patients of systemic sclerosis, systemic lupus erythematosus and mixed connective tissue disorder, respectively. There was overwhelming majority of females, i.e. 86.7% (26 out of 30 patients) in our study. Mean age of our patients was 32.30 ± 13.792 years (range: 16–70 years), with the majority, i.e. 17 (56.7%) in the age group of 16–30 years. Mean duration of the disease from the point of onset of clinical symptoms in our study was 5.35 ± 3.5 years (range: 1–18 years). Most of the patients (66.7%) had disease duration in the range of 1–5 years.
Clinical examination
On comparing the clinical features of these patients, Raynaud's phenomenon was seen in all 16 (100%) patients of systemic sclerosis, 8 (72.7%) patients of systemic lupus erythematosus and all 3 (100%) patients of mixed connective tissue disorder. The most common clinical features in patients of systemic sclerosis were Raynaud's phenomenon, sclerodactyly and binding down of skin, which were present in all 16 patients. Among patients of systemic lupus erythematosus, the most common findings were photosensitivity and a history of alopecia which were present in all patients [Table - 1]. The most common clinical features in patients with mixed connective tissue disorder were the presence of Raynaud's phenomenon and joints involvement, which were present in all three patients. Out of these 30 patients, antinuclear antibodies were seen in 28 (93.3%) patients. In our study, antinuclear antibodies was positive in 14 (87.5%) patients of systemic sclerosis, 11 (100%) patients of systemic lupus erythematosus and 3 (100%) patients of mixed connective tissue disorder. Anti Scl-70 antibody positivity was seen in 10 (62.5%) out of 16 patients of systemic sclerosis and anti dsDNA antibody was detected in 9 (81.8%) out of 11 patients of systemic lupus erythematosus.

Dermoscopic examination
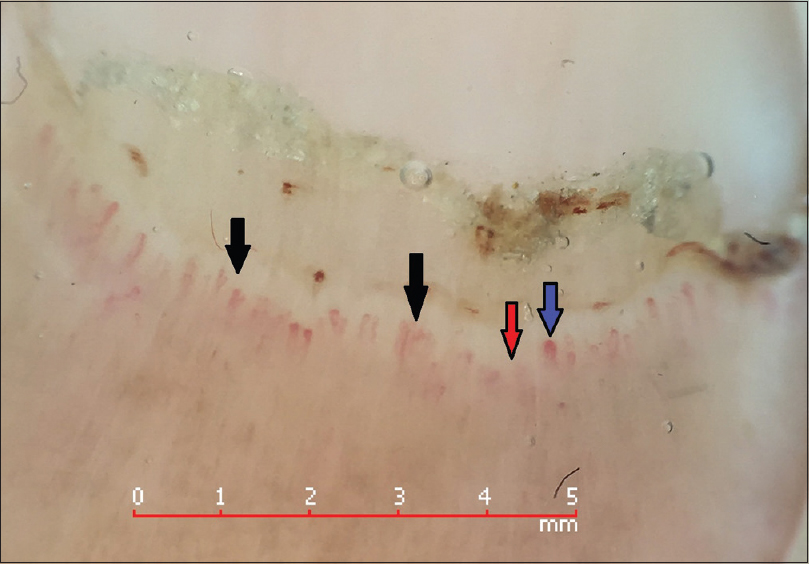
The commonest change recorded in nail fold capillaries in our study was dilated capillaries in 21 (70%) patients, followed by capillary dropouts in 17 (56.7%) patients and avascular areas in 16 (53.3%) patients [Table - 2]. Out of 11 patients of systemic lupus erythematosus, 8 (73%) showed altered capillaroscopy and scleroderma pattern and 3 (27%) patients revealed normal capillary architecture. Dilated capillaries were seen in 8 (72.7%) patients of systemic lupus erythematosus, followed by hemorrhages in 36.4% patients [Figure - 1], [Figure - 2], [Figure - 3], [Figure - 4], [Figure - 5], [Figure - 6], [Figure - 7].

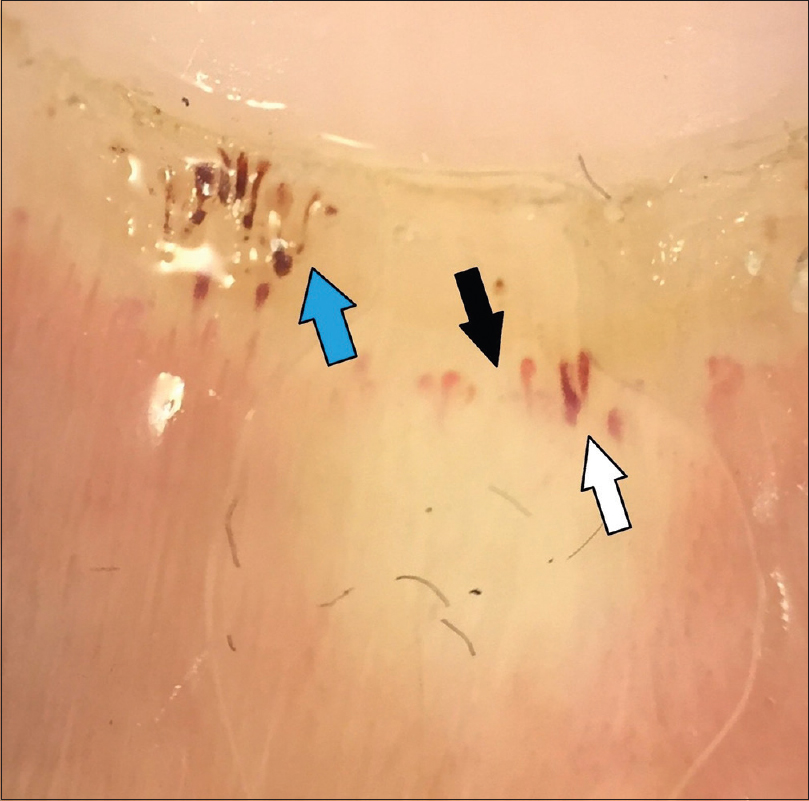 |
| Figure 1: Polarized contact dermoscopy (20x) of nail showing ragged cuticle and dilated capillary (white arrow), hemorrhages (blue arrow) and capillary dropouts (black arrow) |
 |
| Figure 2: Polarized contact dermoscopy (20x) showing capillary dropouts (black arrow), criss cross capillary (blue arrow) and dilated capillaries |
 |
| Figure 3: Polarized contact dermoscopy (20x) of nail fold showing ragged cuticle, dilated capillary (blue arrow) and capillary dropouts |
 |
| Figure 4: Polarized noncontact dermoscopy (20x) showing criss cross capillary (black arrow), dilated capillary (blue arrow), capillary dropouts and avascular areas (red arrow) |
 |
| Figure 5: Polarized noncontact dermoscopy (20x) showing tortuous capillary (black arrow), bushy capillary (blue arrow) and avascular areas (red arrow) |
 |
| Figure 6: Polarized noncontact dermoscopy (20x) showing ragged cuticle, dilated capillary (blue arrow), bizarre capillaries (black arrow), capillary dropouts and avascular areas (red arrow) |
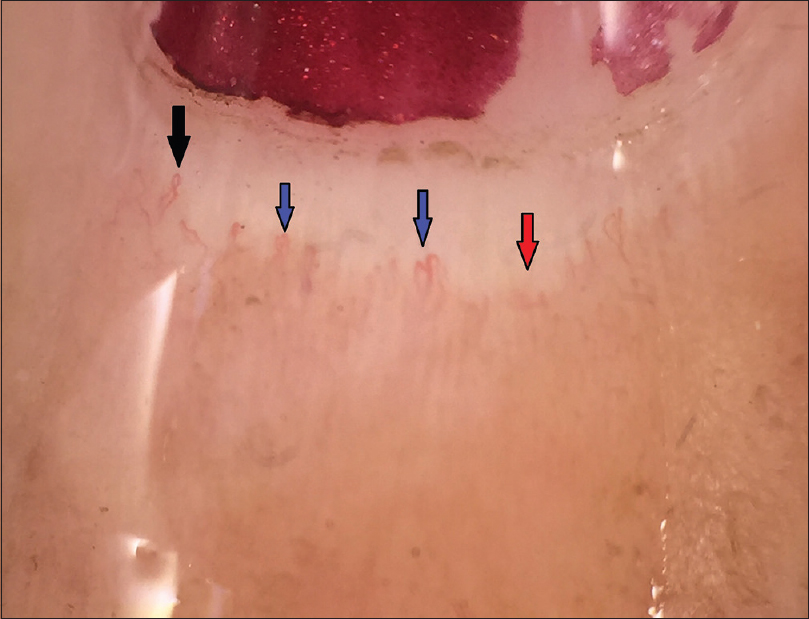 |
| Figure 7: Polarized noncontact dermoscopy (20x) showing bizarre capillaries (blue arrow), criss cross capillaries (black arrow) and avascular areas (red arrow) |
In our study, capillary dropouts were seen in 9 (52.9%), 2 (11.8%) and 6 (35.3%) patients with active, early and late patterns of capillary changes, respectively. Avascular areas were seen in 8 (50%), 1 (6.3%) and 7 (43.8%) patients of active, early and late patterns of capillary changes, respectively. Bizarre capillaries were present in 5 (35.7%), 1 (7.1%) and 8 (57.1%) patients of active, early and late patterns of capillary changes respectively.
Correlation of dermoscopic examination with cutaneous and systemic involvement
Of 17 patients presenting with sclerodactyly, active, early and late patterns were seen in 7 (41.2%), 2 (11.8%) and 7 (41.2%) patients respectively, which was statistically significant (P value = 0.041) [Table - 3] and [Figure - 8]. Out of 11 patients with gastrointestinal symptoms, active, early and late scleroderma pattern were seen in 2 (18.2%), 2 (18.2%) and 5 (45.5%) patients, respectively. However, in 13 patients with respiratory involvement, active, early and late patterns were seen in 1, 1 and 7 (53.8%) patients, respectively (P value = 0.004) [Table - 4] and [Table - 5].

 |
| Figure 8: Correlation of nail fold dermoscopic patterns with cutaneous and systemic involvement |


Discussion
Nail fold dermoscopy is an established method to assess the circulation in patients with Raynaud's phenomenon and collagen vascular disorders, as well as in the early diagnosis and monitoring of these diseases. Dermoscopic nail fold changes, as already been discussed, can be classified into early, active and late patterns, which can be used in evaluating the progression of the microangiopathy.
Antitopoisomerase (Anti Scl-70) antibodies are useful markers to study the activity of disease. Previous studies have revealed correlation of Anti-Scl 70 with active and late capillaroscopic changes. Our study was consistent with earlier studies described in the literature.[3]
In a study conducted by Nagy and Czirjak 102 patients with systemic sclerosis (16 with diffuse cutaneous type and 86 with limited cutaneous type), 14 (87.5%) and 53 (61.6%) showed the scleroderma capillary pattern respectively. Four of the 47 (8.5%) with systemic lupus erythematosus and seven of the 26 (26.9%) with dermato/polymyositis exhibited the scleroderma capillary pattern.[17] In our study, out of 16 patients of systemic sclerosis, the most common nail fold capillary changes were avascular areas and bizarre/bushy capillaries seen in 13 (81.25%) patients each, followed by capillary dropouts and dilated capillaries in 12 (75%) and 11 (68.75%) patients, respectively. Similar frequency of nail fold capillaroscopy changes have been reported by Maricq et al.[11] (83–93% of systemic sclerosis patients) and Bergman et al.[18] (70.4% systemic sclerosis patients). In an Indian study of 42 patients with systemic sclerosis, a similar frequency of bushy capillaries (86.4%) and dilated capillaries (57.6%) was reported.[19]
Our results of SLE patients were discordant with the previous studies by Maricq et al., where only 2% patients of systemic lupus erythematosus (despite the presence of Raynaud's phenomenon) had scleroderma pattern[3] and Blockmans et al., where no patients revealed scleroderma pattern changes.[20] However, our study is in concordance with a study by Furtado et al., where 100 patients of systemic lupus erythematosus were studied. The presence of altered capillaries and scleroderma pattern was associated with the isolated presence of Raynaud's phenomenon (P value <0.001) and anti U1 RNP antibodies (P value <0.001).[21] This difference can be explained by the presence of Raynaud's phenomenon in 8 (72.7%) out of 11 patients of systemic lupus erythematosus in our study, though the number of cases was too small to reach at a conclusion. 66.7% patients of mixed connective tissue disorder revealed nail fold capillaroscopic changes. This frequency is higher as compared to previous studies described in the literature. In the studies by Blockmans et al.[20] and Maricq et al.,[11] 56% and 54% patients respectively of mixed connective tissue disorder revealed these changes. This difference may be explained by the lesser number of patients enrolled in our study Amongst dermoscopic features, dilated capillaries were frequently seen in early and active patterns of the disease, whereas capillary dropouts and avascular areas were commonly seen in active and late patterns. Bizarre capillaries were exclusive to the patients with late patterns. The results of our study were comparable with the study of 97 patients by Cutolo et al.[5],[9]
Various studies have explored correlation between nail fold capillaroscopy changes and type of systemic sclerosis, its clinical activity, as well as visceral involvement[3],[5],[7],[9],[22],[23],[24],[25],[26],[27] but the results are not uniform.[28] The findings of our study [Table - 4] were comparable with the previous studies described in the literature. In a study of 44 patients with collagen vascular disorders by Maricq et al., nail fold capillary changes correlated with systemic involvement, and 26 out of 44 patients with capillary class III–V had 3 or more systems involved.[29] The results of our study are discordant with a previous study of 44 patients of systemic sclerosis by Lovy et al., where no relation was found between nail fold capillary changes and systemic involvement.[30]
To conclude, vascular changes caused by functional and structural abnormalities of the microcirculation play a central role in the pathogenesis of collagen vascular disorders. Nail fold capillaroscopy is a simple, noninvasive, inexpensive and useful tool for the study of microvasculature. So far, the gold standard for performing nail fold capillaroscopy has been nail fold videocapillaroscopy, which requires special equipment, is relatively expensive, time-consuming and not easily portable. A dermoscope is a new, noninvasive, diagnostic tool that visualizes subtle clinical patterns of skin lesions and subsurface skin structures not normally visible to the unaided eye.
Nail dermoscopy can act as mirror for the microangiopathy and thus, the prognosis of these diseases. This is one of the initial studies using a handheld dermoscope to study the same. Handheld dermoscopy is a new upcoming tool for evaluating diseases of microcirculation, particularly collagen vascular disorders. These new-age dermoscopes are compact, handy, pocket-sized instruments that allow us to capture images and store for future references.
However, the study had a few limitations. One is low patient numbers. Inclusion of larger number of patients would have strengthened the observations of the current study. The other is the lack of follow-up. Repeated dermoscopy over a period of time in these cases would have acted as a better method of evaluating the findings vis-a-vis the course of the disease. Though the number of cases in our study was too small to reach at a conclusion, but by looking at the observations of our study, we recommend that dermoscopy be used not only to diagnose collagen vascular disorders but also for establishing the prognosis of the disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Cortes S, Cutolo M. Capillarosecopic patterns in rheumatic diseases. Acta Reumatol Port 2007;32:29-36.
[Google Scholar]
|
| 2. |
Shore AC. Capillaroscopy and the measurement of capillary pressure. Br J Clin Pharmacol 2000;50:501-13.
[Google Scholar]
|
| 3. |
Bollinger A, Fargrell B. Clinical Capillaroscopy – A Guide to its Use in Clinical Research and Practice. Toronto: Hogrefe and Huber Publishers; 1990. p. 1-123.
[Google Scholar]
|
| 4. |
Cutolo M, Grassi W, Matucci Cerinic M. Raynaud's phenomenon and the role of capillaroscopy. Arthritis Rheum 2003;48:3023-30.
[Google Scholar]
|
| 5. |
Cutolo M, Sulli A, Pizzorni C, Accardo S. Nailfold videocapillaroscopy assessment of microvascular damage in systemic sclerosis. J Rheumatol 2000;27:155-60.
[Google Scholar]
|
| 6. |
Cutolo M, Pizzorni C, Sulli A. Capillaroscopy. Best Pract Res Clin Rheumatol 2005;19:437-52.
[Google Scholar]
|
| 7. |
Cutolo M, Sulli A, Secchi ME, Paolino S, Pizzorni C. Nailfold capillaroscopy is useful for the diagnosis and follow-up of autoimmune rheumatic diseases. A future tool for the analysis of microvascular heart involvement? Rheumatology (Oxford) 2006;45 Suppl 4:iv43-6.
[Google Scholar]
|
| 8. |
Cutolo M, Sulli A, Secchi ME, Olivieri M, Pizzorni C. The contribution of capillaroscopy to the differential diagnosis of connective autoimmune diseases. Best Pract Res Clin Rheumatol 2007;21:1093-108.
[Google Scholar]
|
| 9. |
Maricq HR, Harper FE, Khan MM, Tan EM, LeRoy EC. Microvascular abnormalities as possible predictors of disease subsets in Raynaud phenomenon and early connective tissue disease. Clin Exp Rheumatol 1983;1:195-205.
[Google Scholar]
|
| 10. |
Maricq HR, Valter I. A working classification of scleroderma spectrum disorders: A proposal and the results of testing on a sample of patients. Clin Exp Rheumatol 2004;22:S5-13.
[Google Scholar]
|
| 11. |
Maricq HR, LeRoy EC, D'Angelo WA, Medsger TA Jr., Rodnan GP, Sharp GC, et al. Diagnostic potential ofin vivo capillary microscopy in scleroderma and related disorders. Arthritis Rheum 1980;23:183-9.
[Google Scholar]
|
| 12. |
de Holanda Mafaldo Diógenes A, Bonfá E, Fuller R, Correia Caleiro MT. Capillaroscopy is a dynamic process in mixed connective tissue disease. Lupus 2007;16:254-8.
[Google Scholar]
|
| 13. |
Fichel F, Baudot N, Gaitz JP, Trad S, Barbe C, Francès C, et al. Systemic sclerosis with normal or nonspecific nailfold capillaroscopy. Dermatology 2014;228:360-7.
[Google Scholar]
|
| 14. |
Smolen JS, Steiner G. Mixed connective tissue disease: To be or not to be? Arthritis Rheum 1998;41:768-77.
[Google Scholar]
|
| 15. |
Grassi W, De Angelis R. Capillaroscopy: Questions and answers. Clin Rheumatol 2007;26:2009.
[Google Scholar]
|
| 16. |
Maricq HR, LeRoy EC. Patterns of finger capillary abnormalities in connective tissue disease by “wide-field” microscopy. Arthritis Rheum 1973;16:619-28.
[Google Scholar]
|
| 17. |
Nagy Z, Czirják L. Nailfold digital capillaroscopy in 447 patients with connective tissue disease and Raynaud's disease. J Eur Acad Dermatol Venereol 2004;18:62-8.
[Google Scholar]
|
| 18. |
Bergman R, Sharony L, Schapira D, Nahir MA, Balbir-Gurman A. The handheld dermatoscope as a nail-fold capillaroscopic instrument. Arch Dermatol 2003;139:1027-30.
[Google Scholar]
|
| 19. |
Bhakuni DS, Vasdev V, Garg MK, Narayanan K, Jain R, Mullick G. Nailfold capillaroscopy by digital microscope in an Indian population with systemic sclerosis. Int J Rheum Dis 2012;15:95-101.
[Google Scholar]
|
| 20. |
Blockmans D, Beyens G, Verhaeghe R. Predictive value of nailfold capillaroscopy in the diagnosis of connective tissue diseases. Clin Rheumatol 1996;15:148-53.
[Google Scholar]
|
| 21. |
Furtado RN, Pucinelli ML, Cristo VV, Andrade LE, Sato EI. Scleroderma-like nailfold capillaroscopic abnormalities are associated with anti-U1-RNP antibodies and Raynaud's phenomenon in SLE patients. Lupus 2002;11:35-41.
[Google Scholar]
|
| 22. |
Cutolo M, Sulli A, Smith V. How to perform and interpret capillaroscopy. Best Pract Res Clin Rheumatol 2013;27:237-48.
[Google Scholar]
|
| 23. |
Caramaschi P, Canestrini S, Martinelli N, Volpe A, Pieropan S, Ferrari M, et al. Scleroderma patients nailfold videocapillaroscopic patterns are associated with disease subset and disease severity. Rheumatology (Oxford) 2007;46:1566-9.
[Google Scholar]
|
| 24. |
Kim H, Seo SH, Kwok SK, Ju JH, Yoon CH, Park KS, et al. Nailfold capillaroscopic abnormality in systemic sclerosis: Relationship with clinical manifestation. Ann Rheum Dis 2006;65 Suppl 2:396.
[Google Scholar]
|
| 25. |
Ostojić P, Damjanov N. Different clinical features in patients with limited and diffuse cutaneous systemic sclerosis. Clin Rheumatol 2006;25:453-7.
[Google Scholar]
|
| 26. |
Sato LT, Kayser C, Andrade LE. Nailfold capillaroscopy abnormalities correlate with cutaneous and visceral involvement in systemic sclerosis patients. Acta Rheumatol Port 2009;34:219-27.
[Google Scholar]
|
| 27. |
van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A, et al. 2013 classification criteria for systemic sclerosis: An American College of Rheumatology/European League against Rheumatism Collaborative Initiative. Arthritis Rheum 2013;65:2737-47.
[Google Scholar]
|
| 28. |
Lee P, Leung FY, Alderdice C, Armstrong SK. Nailfold capillary microscopy in the connective tissue diseases: A semiquantitative assessment. J Rheumatol 1983;10:930-8.
[Google Scholar]
|
| 29. |
Maricq HR, Spencer-Green G, LeRoy EC. Skin capillary abnormalities as indicators of organ involvement in scleroderma (systemic sclerosis), Raynaud's syndrome and dermatomyositis. Am J Med 1976;61:862-70.
[Google Scholar]
|
| 30. |
Lovy M, MacCarter D, Steigerwald JC. Relationship between nailfold capillary abnormalities and organ involvement in systemic sclerosis. Arthritis Rheum 1985;28:496-501.
[Google Scholar]
|
Fulltext Views
8,126
PDF downloads
3,402





