Translate this page into:
Nail involvement in Langerhans cell histiocytosis and its association with multisystem presentation and lung involvement
Corresponding author: Dr. Arturo Bonometti, Department of Molecular Medicine, Unit of Anatomic Pathology, IRCCS San Matteo Foundation, University of Pavia, Pavia, Italy. arturo.bonometti11@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bonometti A, Passoni E, Finotto S, Berti E. Nail involvement in Langerhans cell histiocytosis and its association with multisystem presentation and lung involvement: Case study and a comprehensive review of the literature. Indian J Dermatol Venereol Leprol 2021;87:850-4.
Sir,
Langerhans cell histiocytosis is a rare proliferation of cells of the mononuclear-phagocyte system mainly affecting children.1
The great heterogeneity of clinical presentation requires histopathological confirmation and a multidisciplinary approach. According to the number of involved sites, Langerhans cell histiocytosis is clinically classified into single-system or multisystem, the latter having a poor prognosis especially when “risk-organs” are involved.1
Nail involvement with varying morphology of changes has been reported, though rarely, in Langerhans cell histiocytosis. Nail involvement has also been considered an unfavorable prognostic sign and seems to be more frequent in multisystemLangerhans cell histiocytosis.2-4
A 41-year-old previously healthy Caucasian man, presented in October 2019, with multiple cutaneous erythematous papules over the scalp, persistent chronic paronychia with onychodystrophy and nail discoloration involving only the fifth finger of the right hand [Figure 1]. Differential diagnoses included onychomycosis, chronic candidiasis, Darier disease and Langerhans cell histiocytosis.

- The patient displayed an involvement of the fifth finger, featuring chronic paronychia with onychodystrophy and a discoloration of the nail lamina.
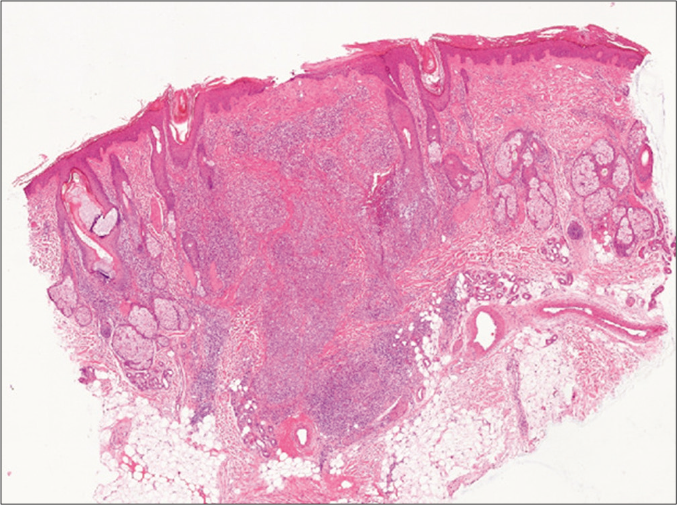
- The skin biopsy of a papular lesion of the scalp revealed a marked dermal, epidermotropic infiltrate made of medium-sized mononuclear cells admixed with macrophages, eosinophils and lymphocytes (H & E, ×20)
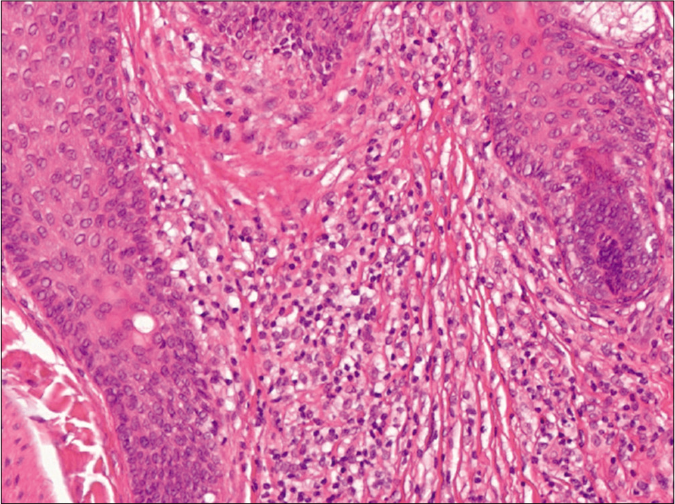
- A marked dermal, epidermotropic infiltrate made of medium-sized mononuclear cells with large indented nuclei admixed with macrophages, eosinophils and lymphocytes. (H & E, ×200)
A diagnostic biopsy of both skin and nail was performed. Both the biopsies revealed findings consistent with Langerhans cell histiocytosis. Complete skeletal survey, whole body computed tomography, laboratory, pulmonary and hematological investigations were normal ruling out the involvement of other organs hence depicting a single-system-Langerhans cell histiocytosis. Sequenced BRAF gene revealed wild-type and it was decided to follow up the patient with only symptomatic treatment. The clinical picture is stable even fourteen months into follow up.
We queried the PubMed database, searching for all the combinations of the word “nail” and synonyms of Langerhans cell histiocytosis. Deduplication, exclusion of non-relevant records and reference list analysis yielded 34 papers, describing a total of 38 patients.
The medical literature currently reports only 38 cases of Langerhans cell histiocytosis with associated nail involvement [Tables 1 and 2]. Most reported patients were young boys. In all but two cases, patients presented with cutaneous, nail and often systemic involvement.
| # | Author | Year | Age/sex/ethnicity | Clinical presentation | Skin/mucosae | n. nails involved | Nail biopsy | Bone | Lung | RO+ | CNS | Outcome | Follow-up (mo) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | TEs | ||||||||||||
| 1 | Bender B | 1958 | 43/F/Cauca | MS RO+ | x | >1 | x | x | x | PD | 48 | ||
| 2 | Kahn | 1969 | 3/F/Caucasi | MS RO+ | x | 10 | x | x | PR | 18 | |||
| 3 | Civatte | 1977 | 40/M/Cauc | MS RO+ | x | >1 | x | x | x | DOD | 108 | ||
| 4 | Diestelmeier | 1982 | 2/M | MS RO- | x | >1 | x | x | CR | 4 | |||
| 5 | Harper | 1983 | 1/M | MS RO- | x | >1 | x | x | DOD | 5 | |||
| 6 | Timpatanapong (4) | 1984 | 2/M/Asian | MS RO+ | x | 10 | x | x | DOD | 30 | |||
| 7 | Timpatanapong (6) | 1984 | 1/M/Asian | MS RO+ | x | 20 | x | x | x | DOD | 10 | ||
| 8 | Timpatanapong (7) | 1984 | 2/M/Asian | MS RO+ | x | 20 | x | x | x | DOD | 12 | ||
| 9 | Ellis | 1985 | 12/M | SS | x | 1 | CR | 21 | |||||
| 10 | Holzberg | 1985 | 0/M | MS RO+ | x | >1 | x | x | DOD | 19 | |||
| 11 | Pareek | 1985 | 20/M/Causi | MS RO- | x | 10 | x | DOD | 48 | ||||
| 12 | Munro | 1988 | 45/M | MS RO- | x | >1 | x | x | SD | 4 | |||
| 13 | Satriano (1) | 1988 | 30/M | MS RO- | x | >1 | x | x | |||||
| 14 | Satriano (2) | 1988 | 35/F | MS RO- | x | >1 | x | ||||||
| 15 | Alsina | 1991 | 31/M | MS RO- | x | 2 | x | x | x | PR | 5 | ||
| 16 | De Berker | 1994 | 0/M/Caucas | MS RO- | x | >1 | x | SD | 4 | ||||
| 17 | Jain | 2000 | 30/M/Cauc | MS RO- | x | >1 | x | 2 | |||||
| 18 | Mendes | 2006 | 3/M | MS RO- | x | 10 | x | x | CR | 24 | |||
| 19 | Moravvej | 2006 | 20/M/Cauc | SS | x | 20 | SD | 6 | |||||
| 20 | Querings | 2006 | 1/F | MS RO- | x | 10 | x | SD | 120 | ||||
| 21 | Ashena | 2007 | 0/F | MS RO- | x | 20 | x | x | DOD | 22 | |||
| 22 | Mataix | 2008 | 2/F | MS RO- | x | >10 | x | x | PR | 3 | |||
| 23 | Chander | 2008 | 1/M | MS RO+ | x | 20 | x | x | DOD | 4 | |||
| 24 | Yazc | 2008 | 3/M | MS RO- | x | >1 | x | x | SD | 130 | |||
| 25 | Sabui | 2009 | 3/F | MS RO+ | 20 | x | |||||||
| 26 | Ottink | 2013 | 2/M | MS RO- | >1 | x | SD | ||||||
| 27 | De Jesus Semblano Bittencourt | 2016 | 2/M | MS RO+ | x | >10 | x | x | LFU | 1 | |||
| 28 | Figueras-Nart | 2016 | 10/M | MS RO- | x | >1 | x | x | CR | 17 | |||
| 29 | Hocazade | 2016 | 24/F | MS RO+ | x | 10 | x | x | LFU | 108 | |||
| 30 | Calderòn-Castrat | 2017 | 36/F/Cauca | MS RO- | x | 10 | x | x | SD | 180 | |||
| 31 | Ishikawa | 2017 | 43/F | MS RO- | x | 7 | x | ||||||
| 32 | Kumar | 2017 | 1/M | MS RO+ | x | 20 | x | x | x | ||||
| 33 | Mahajan (1) | 2017 | 22/M | MS RO+ | x | 20 | x | x | CR | 11 | |||
| 34 | Mahajan (2) | 2017 | 43/M | MS RO- | x | 20 | x | 60 | |||||
| 35 | Fu | 2018 | 19/M | MS RO+ | x | >1 | x | x | |||||
| 36 | Bender NR | 2018 | 10/M/Afrod | SS | x | 20 | x | PD | 36 | ||||
| 37 | Narayanasamy | 2019 | 1/F | MS RO+ | x | 20 | x | x | PR | ||||
| 38 | Prayogo | 2019 | 0/M | MS RO- | x | 20 | x | x | DOD | 3 | |||
| 39 | Present case | 2020 | 41/M/Cauc | SS | x | 1 | x | SD | 10 |
| All pts. | Pediatric pts. | Adult pts. | |
|---|---|---|---|
| n. of patients | 39/39 (100) | 23/39 (61.5) | 16/39 (41) |
| M/Tot (%) | 28/39 (71.8) | 17/23 (73.9) | 11/16 (68.8) |
| Median age at presentation (y) (range) | 3 (0–45) | 2 (0–12) | 33 (19–45) |
| Clinical picture | |||
| Single-system n(%) | 4/39 (10.3) | 2/23 (8.7) | 2/16 (12.5) |
| MS Tot n(%) | 35/39 (89.7) | 22/23 (95.7) | 14/16 (87.5) |
| MS RO+ (%) | 15/39 (38.5) | 10/23 (43.5) | 5/16 (31.3) |
| Skin involvement n(%) | 37/39 (94.9) | 22/23 (95.7) | 16/16 (100) |
| Bone involvement n(%) | 14/39 (35.9) | 11/23 (47.8) | 3/16 (18.8) |
| Lung involvement n(%) | 19/39 (48.7) | 13/23 (56.5) | 6/16 (37.5) |
| CNS-ND n(%) | 3/39 (7.7) | 1/23 (4.3) | 2/16 (12.5) |
| CNS-DI n(%) | 12/39 (30.8) | 1/24 (4.3) | 11/16 (68.8) |
| Outcome Tot n=31 (Pediatric=21, Adults=10) | |||
| CR | 5/31 (16.1) | 4/21 (19) | 1/10 (10) |
| PR | 4/31 (12.9) | 3/21 (14.3) | 1/10 (10) |
| SD | 8/31 (25.8) | 4/21 (19) | 4/10 (40) |
| PD | 2/31 (6.5) | 1/21 (4.8) | 1/10 (10) |
| DOD | 10/31 (32.3) | 8/21 (8.1) | 2/10 (20) |
| Median time to death for DOD (mo) (range) | 15.5 (3–108) | 11 (3–30) | 78 (48–108) |
| Median FU (mo) (range) | 18 (1–180) | 18 (1–130) | 29.5 (4–180) |
CNS-DI: Diabetes insipidus, CNS-ND: Neurodegeneration, CR: Complete remission, DOC: Dead for other cause, DOD: Dead of disease, FU: Follow-up, LFU: Lost at follow-up, M: Male, mo: Months, MS: Multisystem, PD: Progressive disease, PR: Partial remission, pts.: Patients, Rel: Relapse, RO: Risk-organs involvement, SD: Stable disease, SS: Single-system, Tot: Total, y: Years
Nail changes included onycholysis (28/38, 73.7%), subungual hyperkeratosis (23/38, 60.5%), purpuric striae (21/38 55.3%), nail dystrophy (21/38, 55.3%), paronychia (11/38, 28.9%), pachyonychia (8/38, 21.0%) and longitudinal grooving (8/38, 21.0%). In most cases, more than one nail presented with changes and in 21/38 (55.3%) of them, all fingernails were involved. Nail involvement by Langerhans cell histiocytosis was histopathologically proven in nine cases [Table 1]. In 35 (92.3%) of cases, the nail changes were present at disease onset.
Most patients displayed multisystem Langerhans cell histiocytosis, especially in the pediatric sub-cohort (22/28, 92.8% vs. 14/16 87.5% among adult patients). Around half of the cases displayed lung involvement. Bone involvement, diabetes insipidus and risk organ involvement were seen in a third of cases each. Risk organ involvement had similar incidence in children and adults.
Two papers investigated the BRAF mutational status (including present case) and both were wild-type.4
Most patients were treated with polychemotherapy including prednisone, vinca alkaloids, 6-mercaptopurine, methotrexate, cyclophosphamide, etoposide, and/or cytosine arabinoside. 5/31 (16.1%) patients with follow-up data, achieved complete remission, while 9/31 (29.0%) died of disease after a median of 15.5 months.
Among the patients who died of the disease, most were males (7/8, 87.5%) with all fingernails involved, had a median age at diagnosis of two years (range 0–40) and all displayed multisystem involvement.
According to our review of literature, nail involvement in Langerhans cell histiocytosis is rare; it occurs more frequently in male children and is often associated with skin lesions.
Clinically, the major differential diagnosis of nail changes in Langerhans cell histiocytosis includes onychomycosis, psoriasis, chronic mucocutaneous candidiasis, Darier disease, pachyonychia and dyskeratosis congenita. Clinical, histopathological and laboratory findings are needed to confirm the diagnosis.
Nail involvement in Langerhans cell histiocytosis associates with a multisystem presentation and with an unusually high incidence of lung involvement in children. While pulmonary involvement is observed in around 25% of children with Langerhans cell histiocytosis, in our review, lung involvement occurred in 13/23, (56.5%) of pediatric patients with Langerhans cell histiocytosis with nail changes. The opposite was observed for adults, with 6/16 (37.5%) having lung involvement in patients with nail involvement, compared with 62% in the general adult Langerhans cell histiocytosis population, respectively.
Interestingly, both patients showing the involvement of a single nail (including ours), presented with single-system cutaneous involvement and displayed a favorable outcome, while most patients who had a fatal outcome showed involvement of all fingernails.
Despite BRAF mutation in Langerhans cell histiocytosis is associated with a worse prognosis in both low and high-risk patients; data are lacking concerning Langerhans cell histiocytosis patients with nail involvement. Therefore, we could not analyze this aspect in our work.5
Our review highlights an association between nail involvement in Langerhans cell histiocytosis and multisystem presentation with lung involvement in pediatric patients. This is of special interest given the rarity of the lungs involvement in Langerhans cell histiocytosis children and may be a useful and inexpensive dermatological marker of disease extent and perhaps of prognosis.
Acknowledgments
The authors would like to thank Dr. Chiara Moltrasio and Dr. Carlo Alberto Maronese for their help in the gathering of data for the preparation of the paper.
Authors’ contributions
Study concept, design and supervision: AB. AB wrote the first draft. Acquisition, analysis and interpretation of data: AB, EB. EP, SF and EB provided the data and performed clinicopathological correlations. Histological and immunohistochemical reviews were performed by AB and EB. All authors edited and approved the final draft.
Ethics approval
The study was conducted following local ethical guidelines (Fondazione IRCCS Ca' Granda Institutional review board approval #179/13).
Consent to participate and for publication
The patient’s informed consent was gathered and the study was conducted following the Helsinki declaration.
Availability of data and material
All presented data are available and accessible from international literature.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016;127:2672-81.
- [CrossRef] [Google Scholar]
- Nail changes in Langerhans cell histiocytosis. J Eur Acad Dermatol Venereol. 2000;14:212-5.
- [CrossRef] [Google Scholar]
- Nail changes in Langerhans cell histiocytosis: A possible marker of multisystem disease. Pediatr Dermatol. 2008;25:247-51.
- [CrossRef] [Google Scholar]
- Langerhans cell histiocytosis with prominent nail involvement. J Cutan Pathol. 2019;46:1-5.
- [CrossRef] [Google Scholar]
- BRAF mutation correlates with high-risk Langerhans cell histiocytosis and increased resistance to first-line therapy. J Clin Oncol. 2016;34:3023-30.
- [CrossRef] [Google Scholar]





