Translate this page into:
Nail pitting and onycholysis
Correspondence Address:
Vikrant M Jadhav
Ward -33, Department of Skin & VD, Sasson Hospital, Pune - 1, Maharastra
India
| How to cite this article: Jadhav VM, Mahajan PM, Mhaske CB. Nail pitting and onycholysis. Indian J Dermatol Venereol Leprol 2009;75:631-633 |
Introduction
Nail disorders comprise of approximately 10% of all dermatologic conditions. [1] The nail unit may show specific changes that are markers for a wide range of systemic disorders. Furthermore, there are a number of heritable and non-heritable syndromes in which the nail disease is an integral part of the multisystem disorder.
Sometimes a developmental defect may be limited to the nail. Additionally, a number of dermatologic disorders may affect the nail. Consequently no dermatologic examination is complete without a detailed examination of the nails. However, the nail still remains an understudied, underutilized, yet quite an accessible structure that lends itself for examination and evaluation. Pathology in any portion of the nail apparatus results in an abnormal nail sign. Nail signs occur in the nail plate and the paronychial tissues, including the nail bed, nail fold, and the visible portion of the lunula. Among the various nail signs, we will concentrate on two common nail signs in this article (1) nail pitting (2) onycholysis.
Nail Pitting
Pits are superficial depressions within the nail plate that vary in morphology and distribution.
A pit indicates a defect in the uppermost layer of the nail plate, which arises from the proximal nail matrix. [2]
Pathogenesis
Clusters of parakeratotic cells in the stratum corneum disrupt the process of normal keratinization. As the nail plate grows outward, these parakeratotic foci are exposed to the surrounding environment and there is a gradual sloughing of these cells leaving a distinct depression within the nail plate. [2]
Although nail pitting is primarily associated with disease of the proximal nail matrix, the proximal nail fold can also contribute to this process, because the ventral surface of the proximal nail fold closely overlies the nail matrix. It is believed that the parakeratotic and inflammatory cells originating from this structure become entrenched into the surface of the nail plate as parakeratotic foci. [2]
Causes of Pitting
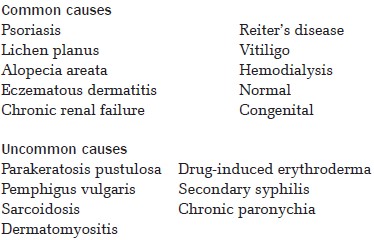
Types of Pitting
- Irregular pitting: - seen in psoriasis. Usually shallow and small (< 1 mm).
- Geometric pitting: - multiple small superficial pits, which are regularly distributed in a geometric pattern along longitudinal or transverse lines. Seen in alopecia areata. [3]
- Coarse pitting and cross ridging: - very irregular pits seen in eczematous dermatitis. [3]
- Elkonyxis: - very large pits, seen in syphilis, Reiters disease, after trauma, and after etretinate and isotretinoin therapy. [4],[5]
- Rosenaus depression: - small pitted craters found on the middle and ring finger and are reported to occur in diabetes mellitus. [6]
Important Facts About Nail Pitting
- Pits more commonly affect finger nails than toe nails.
- Isolated nail involvement with more than 20 pits are suggestive of having a psoriatic etiology. [7]
- A rare uniform pitting of the whole nail plate appears to be a developmental anomaly in its own right. [4]
- Pitted nail grows faster as compared to a normal nail.
- The distance of a pit from the proximal nail fold is suggestive of the length of time for which the matrix was affected by the pathology. [2]
- A deeper depression would be indicative of intermediate and ventral matrix involvement, in addition to the dorsal section. [2]
- The amount of time for which the matrix is free of any pathology directly corresponds to the length of normal nail plate growth observed. [2]
- Pitting is occasionally helpful in building a clinical case for psoriatic arthritis, in the absence of other definitive markers, especially where it is the only cutaneous manifestation of psoriasis.
Onycholysis
Onycholysis is defined as a distal or distal lateral separation of the nail plate from the underlying and/or lateral supporting structures (nail bed, hyponychium, lateral nail fold). When the separation begins proximally near the nail matrix, the process is called onychomadesis. Onycholysis is a common disorder. [8]
The pathogenesis in a number of cases may be unclear. It is known that a normal nail bed does not have a granular layer. Any process that disturbs the normal formation of the nail bed, like psoriasis or lichen planus, which can form a nail bed granular layer, can cause onycholysis. Trauma, be it physical, irritation-induced, or allergic can cause onycholysis.
The area of separation below the nail plate appears white or yellow due to air beneath the nail. Discoloration may occur from the accumulation of bacteria, most commonly pseudomonas or yeast, for example, Candida albicans. Color change such as green may be seen due to pyocyanin from pseudomonas, black or blue discoloration may also be seen.
Onycholysis can be classified as primary (idiopathic) and secondary.
Idiopathic
This is a painless separation of the nail from the nail bed, which occurs without apparent cause. Overzealous manicure, frequent wetting, and cosmetic solvents may be the cause. Minor trauma can cause this condition in persons who keep their nails abnormally long. The affected nail grows very quickly. [9]
Pain occurs only if there is further separation as a result of trauma or if active infection supervenes. The infective organisms include Candida albicans and pseudomonas pyocyanea.
The condition is most commonly seen in women and many cases return to normal after a few months. The longer it lasts, the less likely is the nail to become reattached, due to keratinization of the exposed nail bed.
Secondary
It can be further classified into:
- Dermatologic causes
- Drug-induced
- Systemic causes
- Others
Dermatologic Causes
The numerous dermatologic conditions leading to onycholysis include psoriasis, fungal infection, Reiters syndrome, hyperhydrosis, pemphigus vulgaris, pellagra, leprosy, syphilis, occupational trauma, psoriatic arthritis, and so on.
Drugs
Numerous drugs have been reported to induce onycholysis.
Antibiotics
Cefaloridin, chloramphenicol, chlortetracycline, doxycycline, minocycline. Chemotherapeutic agents;- Adriamycin, bleomycin, 5-fluorouracil, mitoxantrone, paclitaxel, and docetaxel.
Miscellaneous
Acridine, captopril, phenothiazines, retinoids, sulfa drugs, and thiazides.
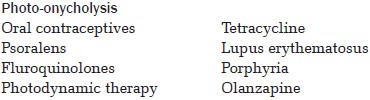
In drug-induced photo-onycholysis, the lateral margins of the nails are never involved and thumbs are also rarely affected. The nail is tender and painful in tetracycline or psoralen-induced photo-onycholysis. Photosensitivity, nail discoloration, and onycholysis are typical of the former (Segal′s triad). [10]
Systemic Causes
Thyroid diseases, Yellow nail syndrome, Shell nail syndrome, Bronchogenic carcinoma, Multiple myeloma, Scleroderma, Anemia, Peripheral vascular diseases, and diabetes mellitus.
Plummer nail
In this type of onycholysis the free edge of the nail is undulated and curved upward, characteristically seen in thyrotoxicosis. [11]
Others
Nail cosmetics, Pregnancy, Hereditary.
| 1. |
Guidelines/Outcomes Committee, American Academy of Dermatology. Guidelines of care for nail disorders. J Am Acad Dermatol 1996;34:375-8.
[Google Scholar]
|
| 2. |
Zaias N. The nail in health and disease, 2 nd ed Norwalk: Appleton and lange; 1990.
[Google Scholar]
|
| 3. |
Tosti A, Piraccani B, Dermatologic diseases. In: Scher RK, editor. Nails Diagnosis, Therapy and Surgery, 3 rd edition. Phiadelphia: Saunders; 2005. p. 116.
[Google Scholar]
|
| 4. |
Baran R, Dawber RPR. Physical signs. In: Baran R, Dawber RPR, editors. Diseases of the nail and their management. 2 nd ed. Oxford: Blackwell Scientific Publications; 1994. p. 35-80.
[Google Scholar]
|
| 5. |
Yung A, Johnson P, Goodfield MJD. Isotretinoin - induced elkonyxis. Br J Dermatol 2005;153:669-70.
[Google Scholar]
|
| 6. |
Greene RA, Scher RK. Nail Changes associated with diabetes mellitus. J Am Acad Dermatol 1987;16:1015-21.
[Google Scholar]
|
| 7. |
Baran R, Dawber RPR. The nail in dermatologic diseases. In: Baran R, Dawber RPR editor. Diseases of nail and their management, 2 nd edition. Oxford: Blackwell Scientific Publications; 1994. p. 135-73.
[Google Scholar]
|
| 8. |
Daniel CR 3rd. Onycholysis: an overview. Seminars in Dermatology 1991;10:34-40.
[Google Scholar]
|
| 9. |
Dawber RP, Samman PD, Bottoms E. Fingernail growth in idiopathic and psoriatic onycholysis. Br J Dermatol 1971;85:558-60.
[Google Scholar]
|
| 10. |
Baran R, Juhlin L. Photo-onycholysis due to tetracycline. Photodermatol Photoimmunol Photomed 2002;18:202-7.
[Google Scholar]
|
| 11. |
Tosti A, Baran R, Dawber RPR. The nail in systemic diseases and drug induced changes. In: Baron R, Dawber RPR, editors. Diseases of the nail and their management. 2 nd edition. Oxford: Blackwell Scientific Publications; 1994. p. 175-261.
[Google Scholar]
|
Fulltext Views
24,032
PDF downloads
4,706





