Translate this page into:
Narrow-band ultraviolet B home phototherapy in vitiligo
2 Department of Dermatology, Shandong Provincial Institute of Dermatology and Venereology, Jinan, Shandong, China
3 Department of Dermatology, Shandong Clinical College of Skin Diseases, Anhui Medical University; Department of Dermatology, Shandong Provincial Institute of Dermatology and Venereology; Department of Dermatology, Shandong Provincial Key Lab for Dermatovenereology, Jinan, Shandong, China
Correspondence Address:
Furen Zhang
Shandong Provincial Institute of Dermatology and Venereology, 27397 Jingshi Road, Jinan, Shandong Province, 250022
China
| How to cite this article: Shan X, Wang C, Tian H, Yang B, Zhang F. Narrow-band ultraviolet B home phototherapy in vitiligo. Indian J Dermatol Venereol Leprol 2014;80:336-338 |
Sir
Conventional narrow-band ultraviolet B (NB-UVB) therapy entails frequent visits to a hospital-based phototherapy unit over several months. The financial and logistical requirements push this modality out of the reach of many vitiligo patients. Home phototherapy, which was introduced for the treatment of psoriasis and other dermatoses, [1] is safe and cost-effective and the level of effectiveness is similar to that achieved with hospital phototherapy. [2] Earlier studies have been conducted mostly in western populations; we report its use in Chinese vitiligo patients.
The study protocol was approved by the institute review board of the Shandong Provincial Institute of Dermatology and Venereology, Jinan, China. The study was open and uncontrolled; vitiligo patients were enrolled and each patient gave written consent to be included in the trial and to be photographed.
Home phototherapy was carried out using the SS-01 UV phototherapy instrument (Shanghai Sigma High-tech Co. Ltd, Shanghai, China) which bears two Philips TL-9W/01 lamps. The equipment delivers NB-UVB rays of wavelength spectrum 310-315 nm, with a maximum of 311 nm and radiant intensity of ~ 10 mW/cm 2 , over a 9 × 7 cm area [Figure - 1].
 |
| Figure 1: The portable phototherapy device used in the study |
Treatment was started with a dose of 0.3 J/cm 2 , independent of skin type, with increments of 0.1 J/cm 2 per session until a dose causing pink erythema was reached. Treatments were given thrice a week on non-consecutive days. It should be noted that the optimal dose is different for different sites of the body; for example, a patient might require 0.4 J/cm 2 to induce pink erythema on the trunk, but 0.9 J/cm 2 on the back of the hand. The dose was increased independently in different affected areas until the pink erythema dose was reached and these area-wise dosages were maintained during subsequent treatment sessions unless erythema was not evident. Eyes, genitalia, and other uninvolved areas were protected during treatment
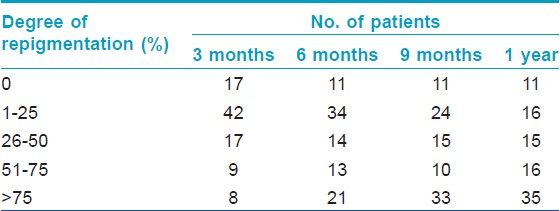
Patients were examined at baseline and reviewed every 3 months for up to one year, to assess repigmentation and any side-effects. Throughout the study, photographs of all vitiligo patches were taken with a digital camera and repigmentation was evaluated by comparison of photographs by two independent observers. Repigmentation was graded as follows: score 0, none; score 1, poor (up to 25%); score 2, moderate (26%-50%); score 3, good (51%-75%); and score 4, excellent (76%-100%). Data was analyzed using SPSS (Windows version 12.01).
A total of 93 vitiligo patients (46 males and 47 females) were enrolled in this study. None of them had any prior experience of home phototherapy and most had never received phototherapy. The patients (or their parents, in case of children) were taught how to use the phototherapy instrument at home. Training took no longer than 30 min for any patient and younger people learnt more quickly.
The mean patient age was 22.58 ± 13.3 years (range 2-65 years) and the mean disease duration was 44.66 ± 59.89 months (range 1-360 months). In 11, 5, 4, and 5 cases, patients decided to discontinue the treatment at less than 3, 6, 9, and 12 months, respectively, owing to poor repigmentation.
Many patients had some degree of repigmentation within 1 month, mainly in perifollicular areas. The rate of repigmentation was fastest within the first 3 months and was maintained in the next 3 months. For patients with a poor therapeutic effect in the first 3 months, there was no improvement in the response to subsequent treatments. Although the repigmented area gradually expanded as treatment progressed, there seemed to be a tendency for the rate of repigmentation to reduce after 6 months. [Table - 1] details the response to therapy seen in the 93 studied patients. At the end of 1 year, 35 patients achieved excellent repigmentation, 16 achieved good repigmentation, 15 showed moderate repigmentation, 16 had poor repigmentation, and 11 had no repigmentation.
Of the 93 patients in the study, 36, 43, 34, and 29 had lesions on the face/neck, trunk, limbs, and hands/feet, respectively. It was observed that some sites on the body responded better than others. The best response (excellent repigmentation) after 1 year was seen in 27 of 36 cases with face and neck lesions [Figure - 2], followed by 16 of 43 cases with truncal vitiligo and 9 of 34 with limb lesions. Lesions on the hands and feet were resistant to treatment and excellent repigmentation was achieved in only 2 out of 29 such cases.
 |
| Figure 2: Different response to the treatment in face and abdomen of a patient before (a, c) and after the treatment (b, d) |
Adverse effects of phototherapy were minimal and did not necessitate treatment discontinuation. Eleven patients complained of burning or pruritus in the lesions and 6 reported dryness of skin. These minor problems were addressed by adjusting the irradiation dose or by application of emollients.
NB-UVB phototherapy normally takes only a few minutes but patients need to travel to the hospital during working hours, twice or thrice a week, over a considerable length of time, usually several months. In an attempt to overcome the drawbacks of conventional UVB treatment, home UVB phototherapy was introduced in 1979. [1] The effectiveness of home phototherapy appears to be similar to that of hospital-based phototherapy and it appears to be safe and cost-effective. [2],[3],[4]
To our knowledge, this is the first report of home phototherapy for vitiligo from China. In our study, most patients had good compliance. Repigmentation was usually observed after 1 month and some patients with localized lesions achieved complete repigmentation within 3 months. Our findings indicate that excellent results can be achieved when a positive response is seen in the early stages of treatment. Further, if a patient has no response within 3 months, discontinuation of treatment should be considered.
Unlike earlier studies on home phototherapy, [2],[3] our study utilized a portable device affordable by most Chinese patients. This portable device can irradiate only a limited area at a time, hence, patients with extensive vitiligo lesions need longer to complete each treatment. However, the slightly greater time taken for each session of home phototherapy is trivial compared with the total time and cost of frequent visits to a hospital phototherapy unit. Another important benefit of the device we used is in the context of variation in sensitivity to phototherapy of different body sites; for example, lesions on hands and feet need more radiation to obtain the optimal dose. The advantage of this portable device is that lesions on different body sites can be given different doses of radiation.
In keeping with available literature [5] short-term adverse effects in our study were minimal and easily resolved. As for long-term side effects, most patients received phototherapy for longer than 1 year and no cutaneous malignancy was found though a significantly longer follow up is required to document the frequency of this complication.
| 1. |
Larko O, Swanbeck G. Home solarium treatment of psoriasis. Br J Dermatol 1979;101:13-6.
[Google Scholar]
|
| 2. |
Cameron H, Yule S, Moseley H, Dawe RS, Ferguson J. Taking treatment to the patient: Development of a home TL-01 ultraviolet B phototherapy service. Br J Dermatol 2002;147:957-65.
[Google Scholar]
|
| 3. |
Wind BS, Kroon MW, Beek JF, van der Veen JP, Nieuweboer-Krobotová L, Meesters AA, et al. Home vs. outpatient narrowband ultraviolet B therapy for the treatment of nonsegmental vitiligo: A retrospective questionnaire study. Br J Dermatol 2010;162:1142-4.
[Google Scholar]
|
| 4. |
Haykal KA, DesGroseilliers JP. Are narrow-band ultraviolet B home units a viable option for continuous or maintenance therapy of photoresponsive diseases? J Cutan Med Surg 2006;10:234-40.
[Google Scholar]
|
| 5. |
Kishan Kumar YH, Rao GR, Gopal KV, Shanti G, Rao KV. Evaluation of narrow-band UVB phototherapy in 150 patients with vitiligo. Indian J Dermatol Venereol Leprol 2009;75:162-6.
[Google Scholar]
|
Fulltext Views
5,976
PDF downloads
1,847





