Translate this page into:
Necrobiosis lipoidica developing within a surgical scar in a non-diabetic patient: Type III Koebner phenomenon (isomorphic response), Wolf's isotopic response or Ruocco's immunocompromised cutaneous district?
2 Department of Dermatology, Jinemez Diaz Foundation, Madrid, Spain
3 Université Libre de Bruxelles, Bruxelles, Belgium
Correspondence Address:
Luc�a Prieto-Torres
Department of Dermatology, Lozano Blesa University Hospital, Avda. San Juan Bosco, 15, Zaragoza 50009
Spain
| How to cite this article: Prieto-Torres L, Bernárdez C, Hernández-Ostiz S, Pastushenko I, Ara-Martin M, Requena L. Necrobiosis lipoidica developing within a surgical scar in a non-diabetic patient: Type III Koebner phenomenon (isomorphic response), Wolf's isotopic response or Ruocco's immunocompromised cutaneous district?. Indian J Dermatol Venereol Leprol 2017;83:233-236 |
Sir,
Necrobiosis lipoidica is a chronic granulomatous disease typically associated with diabetes mellitus. We report a case of necrobiosis lipoidica occurring in a surgical scar in a non-diabetic patient. We found only nine previous reports of necrobiosis lipoidica appearing after trauma or in surgical scars, as a manifestation of Type III Koebner phenomenon. Most of these were in diabetic patients [Table - 1].
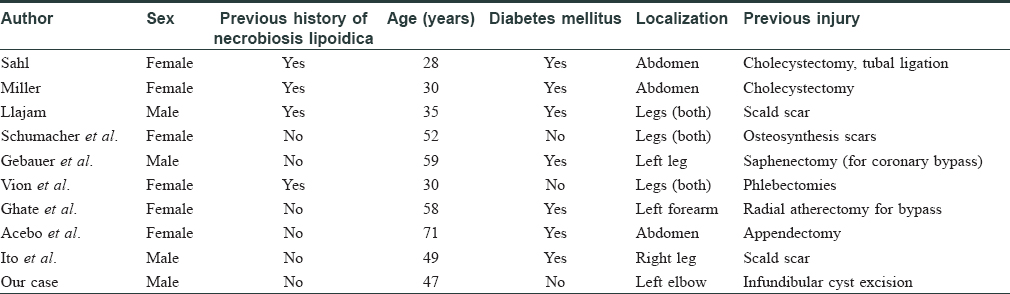
A healthy 47-year-old man presented with a 22-year history of an atrophic erythematous plaque with ulceration, telangiectasia and crusting on his left elbow [Figure 1a]. The patient had undergone a surgical procedure for an infundibular cyst in that region when he was 25 years old. Two months later, he developed an atrophic ulcerated plaque at the site which was considered a complication of surgery. He subsequently experienced numerous episodes of supposed infections. Thus, the entire plaque was excised and reconstructed with a local flap. About 8 months later, the lesions reappeared on the flap. Numerous biopsies were performed subsequently and were reported as granulomatous reaction, granuloma annulare and rheumatoid nodule. Besides this, repeated tissue cultures for fungi, bacteria and mycobacteria were performed with negative results. Radiological tests showed no bone or joint pathology. Hypersensitivity to suture materials was ruled out after doing the standard epidermal “as is” application of the suture material used on the elbow on the back of our patient.
 |
| Figure 1a: At presentation, the patient showed an atrophic, infiltrated plaque with areas of hyperkeratosis and ulceration |
As there was no improvement and no definitive diagnosis, all biopsies were reviewed together. The scanner view of the latest biopsy showed a “sandwich” appearance with the presence of necrobiotic palisading granulomas. These granulomas were composed of epithelioid histiocytes surrounded by lymphocytes and some plasma cells, alternating with horizontal bands of fibrosis and areas of degenerated collagen bundles. The lesion involved the deep reticular dermis and extended into the subcutis [Figure - 2]. On the basis of the clinical features and the histopathologic findings, we made a diagnosis of necrobiosis lipoidica arising in a surgical scar, as a manifestation of Wolf's isotopic response and began treatment with cyclosporine, 3 mg/kg/day. One month after starting treatment, the patient reported improvement with better mobility of the elbow and healing of the ulcer [Figure 1b].
 |
| Figure 1b: One month after administration of cyclosporine, lesion is resolving with healing of the ulcerated areas |
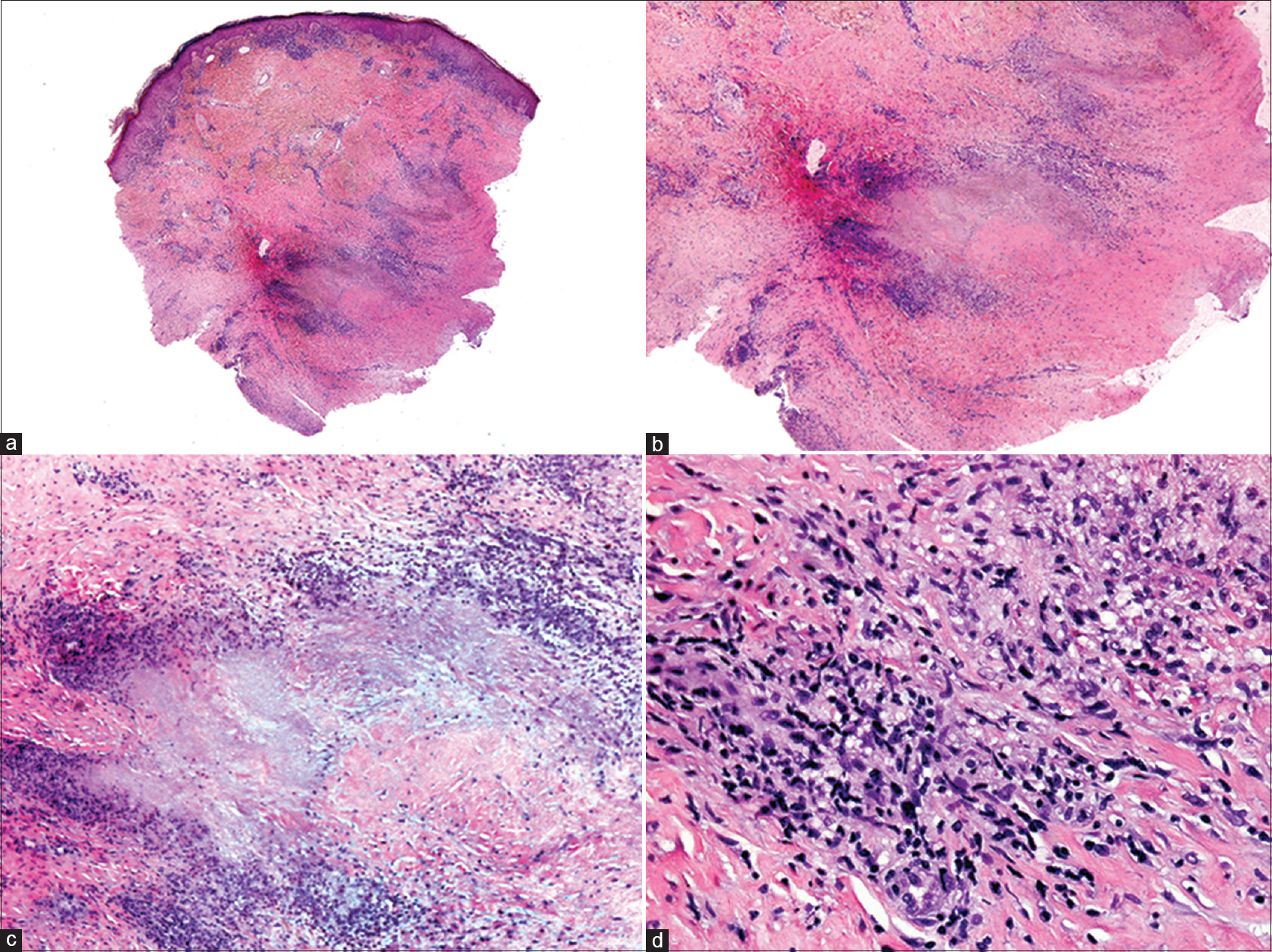 |
| Figure 2: (a) Scanning view showing the characteristic “sandwich” picture involving the dermis and subcutis which consists of alternating horizontal bands of fibrosis and inflammatory infiltrate (H and E, ×20) (b) Higher magnification showing areas of degenerated collagen surrounded by inflammatory infiltrate (H and E, ×100) (c) Higher magnification showing histiocytic infiltrates around areas of degenerated collagen and some mucin deposition (H and E, ×400) (d) Small granulomas in the deep dermis composed of epithelioid histiocytes, surrounded by lymphocytes and plasma cells (H and E, ×400) |
The main histopathologic differential diagnosis in this case is subcutaneous granuloma annulare. Although there was some mucin deposition in the center of the areas of degenerated collagen the extensive fibrosis, the alternating horizontal bands of degenerated collagen and fibrosis as well as the presence of small granulomas composed of epithelioid histiocytes surrounded by plasma cells favored necrobiosis lipoidica rather than subcutaneous granuloma annulare.
Weiss et al.[1] included necrobiosis lipoidica in the Category III of “diseases that may occasionally present as Koebner's phenomenon,” after trauma or surgery. In 1978, Shall reported a case of necrobiosis lipoidica developing within surgical scars following cholecystectomy and tubal ligation, in a diabetic woman.[2] He postulated that reduced resistance of connective and vascular tissue in scars triggers inflammatory and granulomatous diseases. Since then, there have been additional reports of necrobiosis lipoidica which developed at sites of previous trauma or surgery. Most of them were women, in a female-male ratio of 3:2 and the majority were located on the legs and abdomen, following vascular and abdominal surgery.[2],[3],[4] The interval between surgery/trauma and the appearance of the disease was variable from some months as in our case, to 38 years in one case.[4] Some of the patients had, in addition, other dermatological conditions such as psoriasis, morphea or silicotic granulomas.[3],[4]
The pathogenesis of necrobiosis lipoidica remains unknown although several theories have been proposed including alteration in the microvasculature, reduction of lymphatic vessels in the scar area and altered immune response with a predominance of CD8 cells.[3] Controversy still persists about the initiating factor: degeneration of dermal collagen which induces an inflammatory response resulting in the formation of a palisading granuloma; or degeneration of collagen occurring as a consequence of inflammation.[3]
Another interesting point to note is that, of the ten cases we found in the literature, four had a previous history of necrobiosis lipoidica [Table - 1], whereas in the other cases, including ours, this was the first manifestation of the disease. This made us wonder whether this was an isomorphic Koebner's phenomenon or Wolf's isotopic response, which is not previously described in necrobiosis lipoidica, but described in granuloma annulare. Wolf's phenomenon was originally described as the occurrence of a new skin disorder at the site of a previous and already healed herpetic eruption, though a similar phenomenon has been subsequently reported to occur following dermatological conditions not related to herpes.[5] The pathogenic mechanisms may be explained by the larger concept of the immunocompromised cutaneous district. This refers to a locoregional cutaneous immune dysregulation following a prior damaging event that makes a localized area of skin prone to immune-related eruptions or skin disorders. The factors responsible for localized immune dysregulation are multifarious, being represented by chronic lymphatic stasis, herpetic infections, ionizing or ultraviolet radiation, burns, trauma (especially amputation), tattooing, intradermal vaccinations and others of diverse nature (e.g., paralytic stroke and poliomyelitis). Whatever the cause, in time, an immunocompromised cutaneous district may become a vulnerable site, prone to develop opportunistic infections, tumors or dysimmune reactions (often of the granulomatous type), strictly confined to the district itself.[6],[7]
The treatment of necrobiosis lipoidica is challenging. Sometimes, it responds to topical or intralesional corticosteroids [2],[3] and other agents including alprostadil alfadex ointment. We were unable to find any previous reports of improvement following treatment with cyclosporine in necrobiosis lipoidica arising in a surgical scar.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Weiss G, Shemer A, Trau H. The Koebner phenomenon: Review of the literature. J Eur Acad Dermatol Venereol 2002;16:241-8.
[Google Scholar]
|
| 2. |
Sahl WJ Jr. Necrobiosis lipoidica diabeticorum. Localization in surgical scars. J Cutan Pathol 1978;5:249-53.
[Google Scholar]
|
| 3. |
Vion B, Burri G, Ramelet AA. Necrobiosis lipoidica and silicotic granulomas on Muller's phlebectomy scars. Dermatology 1997;194:55-8.
[Google Scholar]
|
| 4. |
Acebo E, Gardeazábal J, Marcellán M, Lasa O, Burgos JJ, Díaz-Pérez JL. Necrobiosis lipoidica over appendectomy scar in a patient with morphea of the breast. Actas Dermosifiliogr 2006;97:52-5.
[Google Scholar]
|
| 5. |
Wolf R, Brenner S, Ruocco V, Filioli FG. Isotopic response. Int J Dermatol 1995;34:341-8.
[Google Scholar]
|
| 6. |
Piccolo V, Baroni A, Russo T, Schwartz RA. Ruocco's immunocompromised cutaneous district. Int J Dermatol 2016;55:135-41.
[Google Scholar]
|
| 7. |
Ruocco V, Ruocco E, Piccolo V, Brunetti G, Guerrera LP, Wolf R. The immunocompromised district in dermatology: A unifying pathogenic view of the regional immune dysregulation. Clin Dermatol 2014;32:569-76.
[Google Scholar]
|
Fulltext Views
3,991
PDF downloads
1,979





