Translate this page into:
Needle radiofrequency ablation (RFA) and topical tacrolimus combination therapy for primary localised cutaneous nodular amyloidosis
Corresponding author: Dr. Neetu Bhari, Department of Dermatology & Venereology, All India Institute of Medical Sciences, Delhi, India. drntbhari@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Danish M, Ahuja R, Gupta S, Bhari N. Needle radiofrequency ablation (RFA) and topical tacrolimus combination therapy for primary localised cutaneous nodular amyloidosis. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_851_2024
Dear Editor,
Primary localised cutaneous nodular amyloidosis (PLCNA) is a rare skin disorder caused by the deposition of amyloid light chains in the skin and associated with minimal systemic involvement. It typically presents as firm, shiny, waxy nodules on acral sites, face, or trunk, and is often resistant to treatment. Managing PLCNA is challenging, and various therapeutic approaches have been explored. This report highlights a case managed using needle radiofrequency ablation (RFA) in combination with a topical tacrolimus 0.1% ointment. The combination therapy resulted in significant improvement, offering a promising and effective treatment option for this rare and difficult-to-treat dermatological condition.
A 50-year-old man presented with asymptomatic, gradually progressive nodular lesions over the left side of the nose since two years. There were no systemic complaints, and the family history was non-contributory. Cutaneous examination revealed yellowish-orange shiny waxy nodules coalescing to form plaques. There was overlying erythema and telangiectasia involving the dorsum and the left side of the nasal bridge [Figure 1]. No other sites were involved. The differential diagnoses of cutaneous sarcoidosis, cutaneous nodular amyloidosis, and lupus vulgaris were considered. Histopathology showed Congo red positive eosinophilic amorphous material in the dermis, along with mild lympho-histiocytic infiltrates, confirming the diagnosis of primary cutaneous nodular amyloidosis [Figures 2a and 2b]. The serum and urine electrophoresis were normal.
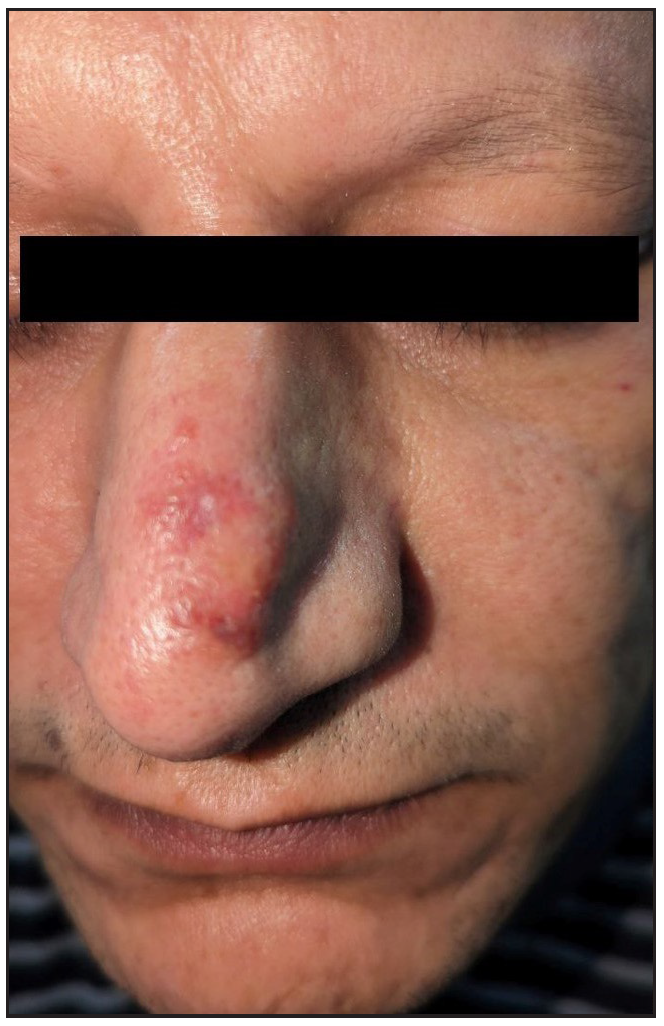
- Yellowish-orange, shiny, waxy nodulo-plaque with erythema and telangiectasias on the left nasal dorsum.
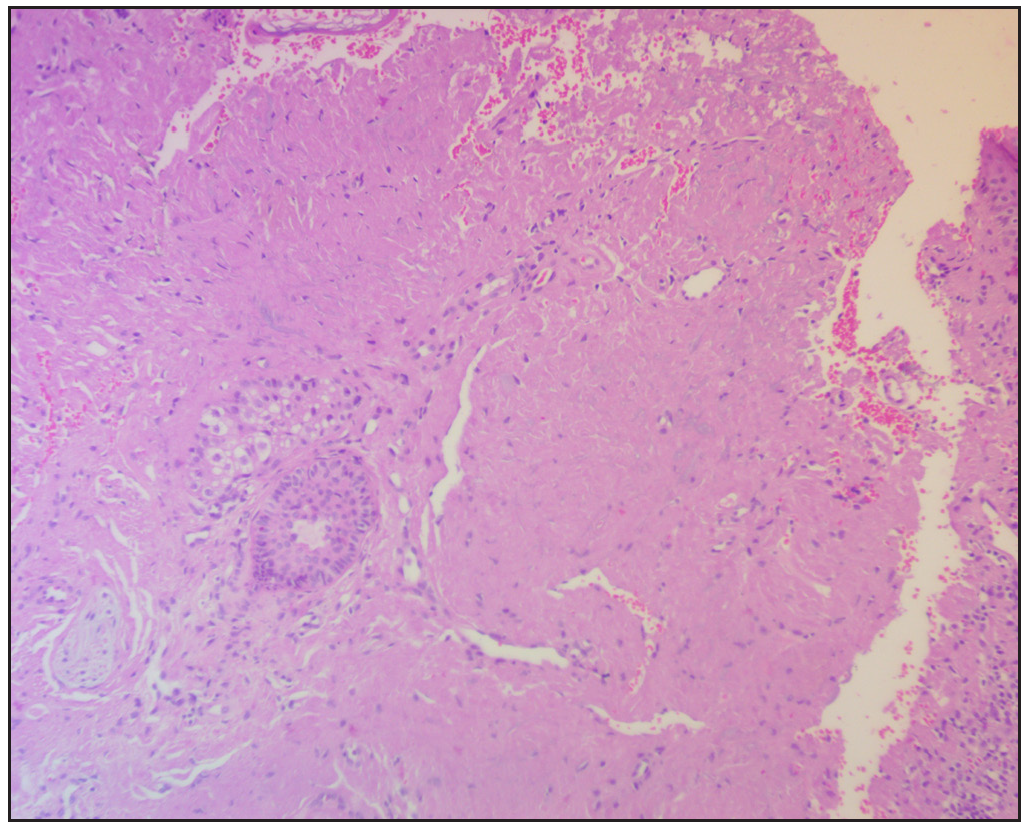
- Histopathology showing deposition of eosinophilic amorphous material in the dermis (Haematoxylin and eosin, 100x)
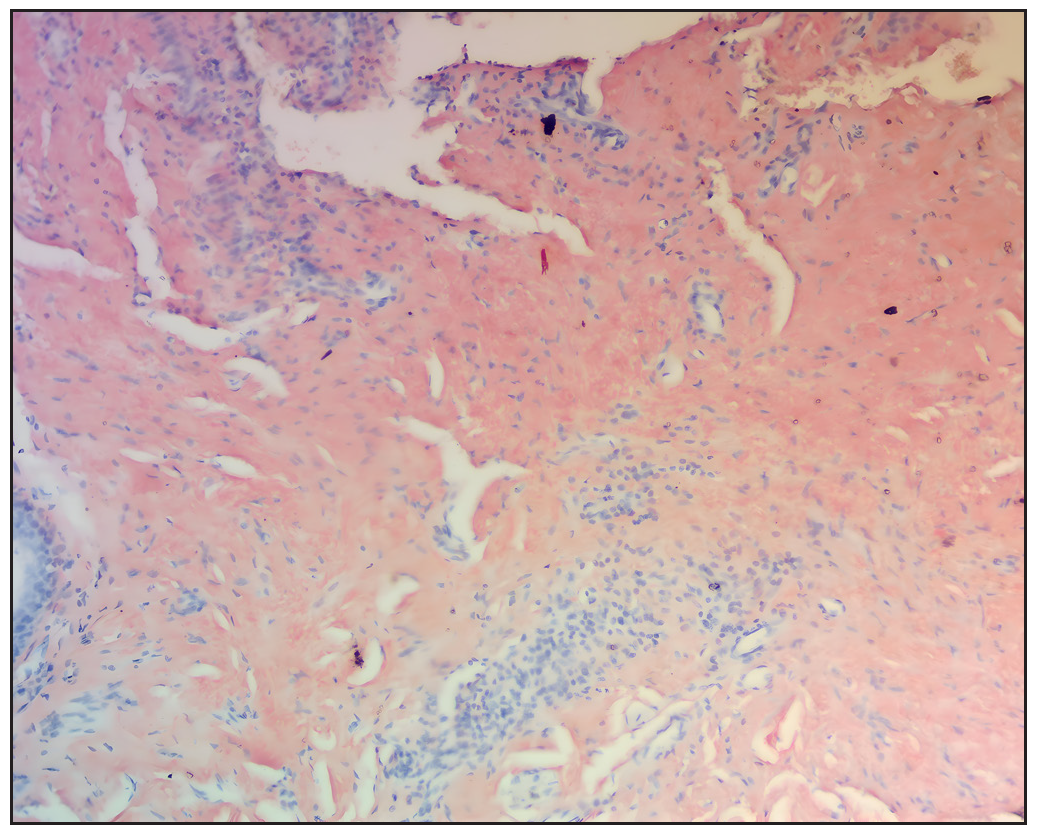
- Congo red stain showing amorphous eosinophillic amyloid deposits in the upper and mid dermis (original magnification ×100)
The lesions were treated with needle RFA. 1 Initially, a non-insulated 27- gauge hypodermic needle was inserted approximately 2-4 mm deep into the lesions. The tip of a radiofrequency probe was then placed on the proximal un-inserted portion of the needle. Low-power energy in the coagulation mode (RF Surgical Generators, power supply: 220 V, Monopolar: 1–80 W) with power ranging from 2 to 5 was applied for 1 to 2 seconds and stopped before removing the needle to coagulate only the central portion of the lesions. This induced contraction of the dermal tissue and resulted in flattening of the lesions while preserving the overlying epidermis. Photoprotection and topical mupirocin were advised for 7 days post-procedure. The patient underwent three sessions of needle RFA over 6 months, resulting in about a 50% reduction in the bulk of the nodules with some scarring. In view of persistent erythema, the patient was started on tacrolimus 0.1% ointment twice a day for 3 months, resulting in almost complete resolution of erythema [Figure 3].

- Showing response to treatment 9 months post treatment.
PLCNA is characterised by the deposition of extracellular amyloid light chains in the skin without systemic involvement. 2 The amyloid deposits in PLCNA are composed of λ and/or ĸ immunoglobulins (AL proteins) produced by local plasma cells, in contrast to the more common types: macular and lichen amyloidosis, where amyloid protein is derived from degenerated keratinocytes. PLCNA usually affects middle aged adults both males and females. The most common sites of involvement include the face, 3 genitalia, acral sites, periauricular area, and occasionally the breast. 4 There are few reports of its association with Sjogren syndrome; therefore, some authors recommend screening with anti-SS-A antibodies. 5 It presents as solitary or multiple asymptomatic shiny, waxy erythematous to yellowish-orange nodules, plaques, or occasionally tumours. These may display a purpuric appearance or surface telangiectasias. Histopathology shows large deposits of amorphous, sometimes fissured, pale, eosinophilic amyloid material in the dermis, extending into the subcutaneous tissue. Special stains such as Congo red, periodic acid-Schiff, or crystal violet can aid in amyloid identification. Primary localised cutaneous nodular amyloidosis shares clinical and histological similarities with the cutaneous lesions seen in primary systemic amyloidosis, both being characterised by deposits of light- chain amyloid protein. Studies have reported about a 4-50% rate of progression to systemic amyloidosis. 6 The patient has been asked to undergo regular follow-up for screening for progression to systemic amyloidosis.
Several treatment modalities have been tried in the literature, including cyclophosphamide pulse, curettage, surgical excision, shave excision followed by dermabrasion, cautery, lasers such as fractional CO2 and PDL lasers, and intralesional methotrexate, bortezomib, or dexamethasone. 7 Surgical excision is the most commonly used treatment for PLCNA. This is the first case report of PLCNA showing response with a less invasive combination therapy of needle RFA and topical tacrolimus, with over 50% improvement in the thickness of nodules and almost complete resolution of erythema. Further studies are needed to confirm the efficacy of this treatment.
In conclusion, a combination therapy of needle RFA and topical tacrolimus is a novel, effective, and safe treatment for PLCNA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Intralesional radiofrequency with a thin hypodermic needle in the management of papular acne scars. J Am Acad Dermatol. 2021;84:e259-60.
- [CrossRef] [PubMed] [Google Scholar]
- Primary localized cutaneous amyloidosis: A systematic treatment review. Am J Clin Dermatol. 2017;18:629-42.
- [CrossRef] [PubMed] [Google Scholar]
- A rare case of primary cutaneous nodular amyloidosis of the face. J Eur Acad Dermatol Venereol. 2008;22:1011-2.
- [CrossRef] [PubMed] [Google Scholar]
- Primary localized cutaneous nodular amyloidosis on areola. Indian J Dermatol Venereol Leprol. 2022;88:653-5.
- [CrossRef] [PubMed] [Google Scholar]
- Localized cutaneous nodular amyloidosis and Sjögren’s syndrome. Intern Med. 2021;60:2513-4.
- [CrossRef] [PubMed] [Google Scholar]
- Nodular localized primary cutaneous amyloidosis: A long-term follow-up study. Br J Dermatol. 2001;145:105-109.
- [CrossRef] [PubMed] [Google Scholar]
- Nodular cutaneous amyloidosis effectively treated with intralesional methotrexate. JAAD Case Rep. 2016;2:373-6.
- [CrossRef] [PubMed] [Google Scholar]






