Translate this page into:
Nevus lipomatosus cutaneus superficialis associated with nevus sebaceous of Jadassohn
2 Department of Dermatology, Dicle University School of Medicine, 21280-Diyarbakir, Turkey
3 Department of Pathology, Dicle University School of Medicine, 21280-Diyarbakir, Turkey
4 Batman Regional Government Hospital, Department of Pathology, Batman, Turkey
5 Istanbul Education and Research Hospital, Department of Dermatology, Istanbul, Turkey
Correspondence Address:
Enver Turan
Department of Dermatology, Faculty of Medicine, University of Harran, 63200, Sanliurfa
Turkey
| How to cite this article: Turan E, Yesilova Y, U�mak D, T�rk�� G, �elik �I, G�rel MS. Nevus lipomatosus cutaneus superficialis associated with nevus sebaceous of Jadassohn. Indian J Dermatol Venereol Leprol 2014;80:194 |
Sir,
Nevus lipomatosus cutaneous superficialis is an uncommon disease of unknown etiology characterized by lipocyte collections situated ectopically within the dermis. Hoffman and Zurhelle first described nevus lipomatosus cutaneous superficialis, (which is also termed pedunculated lipofibroma), in 1921. The typical presentation is as clustered, multiple skin-coloured or yellowish papules or nodules present on the lower trunk, especially on the buttocks. Two types of nevus lipomatosus cutaneous superficialis are defined: the multiple or classic type consists of zonal or segmentally distributed multiple lesions while the solitary type presents as a solitary papule or nodule. [1]
A 21-year-old man presented to our clinic with many asymptomatic nodular lesions distributed in a segmental pattern on the left buttock and left lumbar area. The lesion began 10 years ago and was gradually increasing in size. On dermatologic examination, multiple, skin-colored, soft coalescent papules and nodular lesions were observed in an approximately 15 × 25 cm area in the left sacral and left lumbar region. The lesions were unilateral and did not cross the midline. A 5 × 11 cm diameter flesh-colored, soft to firm, lobulated and smooth surfaced, non-tender, rubbery, sessile cerebriform mass extending to the perianal area was observed in the sacral area [Figure - 1]a. The overlying skin was normal in color and was non-hairy. An excisional biopsy of a lesion located in the gluteal region showed slight papillomatosis and unencapsulated, mature adipocyte aggregates embedded within the collagen bundles in the dermis [Figure - 1]b. A diagnosis of nevus lipomatosus cutaneous superficialis was made.
 |
| Figure 1: (a) Multiple, skin-colored, soft, coalescent papules and nodules spread over an area of approximately 25 cm in the left gluteal and lumbar region. A cerebriform surfaced, 12 cm diameter tumoral lesion extending to the perianal region. (b) Mature adipocyte aggregates of light papillomatosis observed through histopathological examination in the deep dermis, beneath the epidermis. Fat lobules unenclosed by capsule shows continuity with subcutaneous adipose tissue ([i] H and E, ×40; [ii] H and E, ×100) |
Physical examination of the forehead revealed a 2.0 cm × 1.0 cm brown-yellowish, hairless verrucous plaque [Figure - 2]a. The lesions had been noticed in early childhood, but grew larger after puberty. Enlarged local or regional lymph nodes were not detected. On histopathologic examination, the epidermis showed hyperkeratosis, irregular acanthosis and papillomatosis. The dermis showed abundant sebaceous glands and immature hair follicles [Figure - 2]b. Based on these clinical and histopathologic findings, the lesion was diagnosed as nevus sebaceous of Jadassohn.
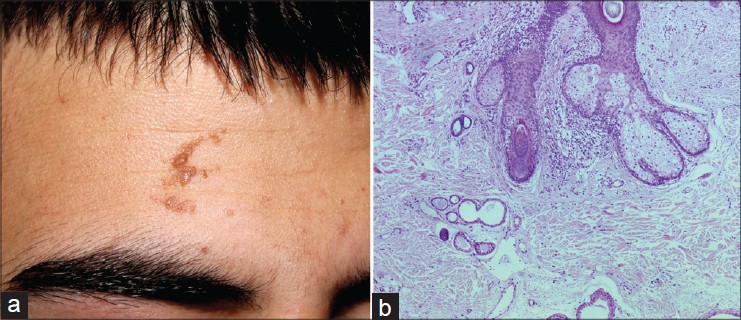 |
| Figure 2: (a) Yellowish verrucous plaque of the forehead, (b) abundant sebaceous glands and dilated apocrine glands in the dermis |
His routine baseline investigations (complete blood count, liver and kidney function, electrolytes and urinalysis) were normal. No pathologic findings were seen on the chest X-ray and abdominal ultrasonography examination. Surgical excision was recommended and the patient was referred to the clinic for plastic and reconstructive surgery.
Discussion
Nevus lipomatosus cutaneous superficialis typically occurs after birth or in the first decades of life. In the classic type, there are skin-colored or yellowish papules or nodules displaying a zosteriform distribution. In the solitary type, which is more common, a single nodule is seen. [1]
The most frequent locations are the pelvic girdle, lumbar region, buttocks, sacrum and the upper back of the thigh. However, unusual cases of the disease occurring on the scalp, neck, face, knee, scrotum, vulva and clitoris have also been reported. There is no definite explanation for the marked predilection of classic type nevus lipomatosus cutaneous superficialis for the pelvic girdle area. In our case, the onset in early childhood, unilateral, segmental distribution and the location were consistent with the classic type of nevus.
There is no reported association with systemic diseases but cases of connective tissue naevi, hemangiomas, café au lait macules, leukodermic spots, [2] angiokeratoma of Fordyce, [3] cavernous hemangiomas, folliculosebaceous cystic hamartoma [4] and basal cell carcinoma [5] accompanying nevus lipomatosus cutaneous superficialis have been reported. However, an association with nevus sebaceous of Jadassohn, a complex, congenital skin hamartoma affecting the pilosabaceous follicle, epidermis and other adnexal structures has not been reported previously.
The origin of nevus lipomatosus cutaneous superficialis remains unclear. Nevus lipomatosus cutaneous superficialis is considered by some as a type of connective tissue nevus because it includes altered mesenchymal dermal components, including collagen bundles, elastic fibers and fibroblasts. Moreover, pilar anomalies, such as hypertrophic pilosebaceous units, fibrofolliculomas and folliculosebaceous cystic hamartomas, have been reported in some cases. Studies are required to determine the role of genetic abnormalities in the development of these two conditions and to clarify the possible relationship between nevus lipomatosus cutaneous superficialis and nevus sebaceous of Jadassohn. The simultaneous presence of two different hamartomatous lesions in our patient may be coincidental but there is a possibility of a common genetic basis.
Another lesson from our case is that lesions co-existing with nevus lipomatosus cutaneous superficialis should not be assumed to be the same condition but should be diagnosed histopathologically.
| 1. |
Khandpur S, Nagpal SA, Chandra S, Sharma VK, Kaushal S, Safaya R. Giant nevus lipomatosus cutaneous superficialis. Indian J Dermatol Venereol Leprol 2009;75:407-8.
[Google Scholar]
|
| 2. |
Jones EW, Marks R, Pongsehirun D. Naevus superficialis lipomatosus. A clinicopathological report of twenty cases. Br J Dermatol 1975;93:121-33.
[Google Scholar]
|
| 3. |
Al-Mutairi N, Joshi A, Nour-Eldin O. Naevus lipomatosus cutaneous superficialis of Hoffmann-Zurhelle with angiokeratoma of Fordyce. Acta Derm Venereol 2006;86:92-3.
[Google Scholar]
|
| 4. |
Kang H, Kim SE, Park K, Son SJ, Song KY. Nevus lipomatosus cutaneous superficialis with folliculosebaceous cystic hamartoma. J Am Acad Dermatol 2007;56:S55-7.
[Google Scholar]
|
| 5. |
Maeda A, Aragane Y, Ueno K, Yamazaki F, Kawada A, Tezuka T. A case of naevus lipomatosus cutaneus superficialis of the scalp associated with pedunculated basal cell carcinoma. Br J Dermatol 2003;148:1084-6.
[Google Scholar]
|
Fulltext Views
3,411
PDF downloads
4,301





