Translate this page into:
Nevus lipomatosus superficialis associated with deep penetrating nevus
Correspondence Address:
Min Geol Lee
Yonsei Ro 50, Seodaemun Gu, Department of Dermatology,Severance Hospital, Yonsei University, College of Medicine, Seoul, 120-752
Korea
| How to cite this article: Kim HJ, Lee MG. Nevus lipomatosus superficialis associated with deep penetrating nevus. Indian J Dermatol Venereol Leprol 2015;81:410-411 |
Sir,
A 52-year-old Korean female complained of a large cerebriform mass on her lower back that had present since birth. Physical examination revealed a 5 × 6 cm, brownish, soft, non-tender, rubbery, sessile, cerebriform mass with some terminal hair on her sacral area [Figure - 1]. The mass was generally asymptomatic but recently itching was noted with gradual and slight increase in size of the mass. She had a history of total thyroidectomy due to thyroid cancer and was taking levothyroxine. She was otherwise healthy without any systemic disease. The family history was unremarkable. Histopathologic evaluation revealed acanthosis of the epidermis as well as clusters of ectopic mature adipocytes in the dermis, which was consistent with the diagnosis of nevus lipomatosus superficialis [Figure - 2]a. The salient feature of this case was that there were also melanocytic proliferations arranged in loose nests or vertically oriented fascicles which extended deep into the subcutis, demonstrating a concomitant deep penetrating nevus. On higher magnification [Figure - 2]b, the cell nests had a more epithelioid component in the upper dermis while a spindle cell population was more prominent in the deeper parts. Melanocytes had finely granulated melanin, oval or elongated nuclei, dispersed chromatin and prominent nucleoli. Ectopic mature adipocytes had a tendency to be present between the nevus cell nests. There was a junctional component composed of lentiginous proliferation and nests of melanocytes with uniform, round to oval nuclei.
 |
| Figure 1: Brown pigmented soft, nontender, rubbery sessile cerebriform mass with some terminal hairs on the sacral area |
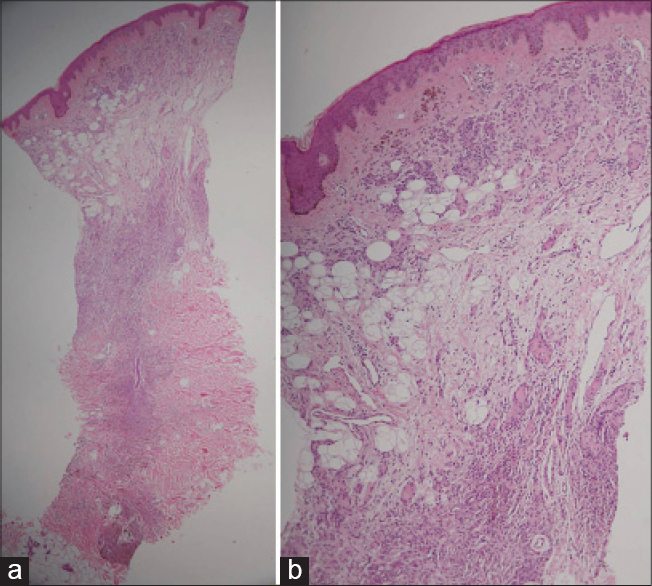 |
| Figure 2: (a) There are ectopic mature adipocytes in the dermis along with melanocytic proliferation arranged in loose nests or vertically oriented fascicles which extend deep into the subcutis (H and E ×100). (b) On higher magnification, the cell nests have more of an epithelioid component in upper dermis and spindle cell population is more prominent in deep dermis. Ectopic mature adipocytes demonstrate a tendency to be present between the nevus cell nests. There are junctional components of lentiginous proliferation and nests of melanocytes with uniform, round to oval nuclei (H and E ×200) |
Nevus lipomatosus superficialis is an uncommon cutaneous hamartoma composed of flesh-colored to yellowish soft papulo-nodules with smooth or wrinkled surface. Histologically, mature fat cells are ectopically located embedded among the bundles of dermal collagen as high as the papillary dermis. [1] The pathogenesis is largely unknown but theories of perivascular differentiating lipoblasts, adipose metamorphosis by degenerative collagen and a developmental displacement of adipose tissue have been suggested. [2] Rare cases have been reported to be associated with folliculo-sebaceous anomalies such as foliculo-sebaceous cystic hamartoma. [1]
Deep penetrating nevus is a distinctive melanocytic nevus that clinically and histopathologically has similarities with cellular blue nevus, Spitz nevus and even melanoma. It usually occurs in the second and third decades of life and less than 5% are reported to develop after the age of 50 years. A characteristic histopathologic feature at scanning magnification is the sharply demarcated, circumscribed, often symmetrical and usually wedge-shaped configuration with the base towards the epidermis and the tip towards the reticular dermis and subcutis. A limited junctional melanocytic component is present in 60-85% of deep penetrating nevus. [3] Cytologically, melanocytic nuclei are hyperchromatic with variation in their size and shape from round to oval. There might be mitoses and cytologic atypia. Cellular nests and fascicles are usually composed of a population of plump fusiform to spindle cells but epithelioid cell components are sometimes conspicuous. The proportion of both the epithelioid and the spindle-shaped components can vary greatly within and among lesions. Robson et al. [4] reported that 22 out of 31 cases had an epithelioid component. The epithelioid cells differed from those seen in common acquired melanocytic nevi by more abundant cytoplasm and larger, albeit regular nuclei. Melanocytes commonly grow along skin adnexa and neurovascular bundles without destroying them. Perineural extension and infiltration of the arrector pili muscle are frequent findings. Deep penetrating nevus is known to often extend into the subcutis. In this case, however, mature adipocytes extended up to the upper reticular dermis, consistent with the findings of nevus lipomatosus superficialis and were admixed with nevus cell nests.
Microscopic evaluation of the current case showed sheets and fascicles of nevus cells between ectopic mature adipose tissue in the dermis and they extended downwards into the subcutis. We were unable to find previous reports of nevus lipomatosus superficialis combined with deep penetrating nevus. The relationship between the two components needs to be elucidated. Although there have been reports of nevus lipomatosus superficialis associated with co-existent pigmentary anomalies including café-au-lait macules or multiple leukodermic spots, nevi composed of melanocytic nests have not been reported. Robinson et al. [4] considered nevus lipomatosus superficialis as a true nevus owing to its location and the histologic changes such as hyperpigmentation, hyperkeratosis, acanthosis and the fact that adipose cells seemed to extend from the subcutis into the dermis. Yakovlev et al. [5] suggested that angiomatosis and other connective tissue nevi were of ectodermal origin, not purely mesodermal maldevelopments. The clinicopathologic consideration of the vascular neurocutaneous syndrome was thought to imply that on the background of congenital malformation of the neuro-ectodermal tissues, develops a superimposed hyperplasia of mesodermal tissues. [5] In this regard, neuroectodermal melanocytic proliferation forming sheets or fascicles of nevus could be associated with hamartomatous changes of mesodermal adipocytes.
| 1. |
Kang H, Kim SE, Park K, Son SJ, Song KY. Nevus lipomatosus cutaneous superficialis with folliculosebaceous cystic hamartoma. J Am Acad Dermatol 2007;56 (2 Suppl):S55-7.
[Google Scholar]
|
| 2. |
Jones EW, Marks R, Pongsehirun D. Naevus superficialis lipomatosus. A clinicopathological report of twenty cases. Br J Dermatol 1975;93:121-33.
[Google Scholar]
|
| 3. |
Barnhill RL, Mihm MC, Jr., Magro CM. Plexiform spindle cell naevus: A distinctive variant of plexiform melanocytic naevus. Histopathology 1991;18:243-7.
[Google Scholar]
|
| 4. |
Robson A, Morley-Quante M, Hempel H, McKee PH, Calonje E. Deep penetrating naevus: Clinicopathological study of 31 cases with further delineation of histological features allowing distinction from other pigmented benign melanocytic lesions and melanoma. Histopathology 2003;43:529-37.
[Google Scholar]
|
| 5. |
Yakovlev PI, Guthrie RH. Congenital ectodermoses (neurocutaneous syndromes) in epileptic patients. Arch Neurol Psychiatry 1931;26:1145-94.
[Google Scholar]
|
Fulltext Views
5,192
PDF downloads
1,887





