Translate this page into:
Nicolau syndrome following sclerotherapy for pyogenic granuloma
2 Department of Plastic Surgery, Bangalore Medical College and Research Institute, Bengaluru, Karnataka, India
Correspondence Address:
Sarvajnamurthy A Sacchidanand
Department of Dermatology, Venereology and Leprosy, Bangalore Medical College and Research Institute, Bengaluru, Karnataka
India
| How to cite this article: Nirmal B, Segu SS, Sacchidanand SA, Deshpande P. Nicolau syndrome following sclerotherapy for pyogenic granuloma. Indian J Dermatol Venereol Leprol 2014;80:484 |
Sir,
Pyogenic granuloma is a benign tumor characterized by lobular capillary proliferation. Conventional treatment includes complete surgical excision with primary closure which results in scarring and cannot be performed in the routine outpatient setting. Sclerotherapy is a simple and novel modality which scores over surgical treatment in terms of lower cost and feasiblity. A 25-year-old male patient presented with a red nodule of size 0.5 Χ 0.5 cm, on the thenar eminence of his right palm, of 2 months duration [Figure - 1]. The lesion was occasionally painful and bled on trauma. A clinical diagnosis of pyogenic granuloma was made and he was offered sclerotherapy with sodium tetradecyl sulfate (STS). A volume of 0.1 ml of 1% STS was injected into the lesion until it blanched completely. Immediately after injection, the patient complained of intense pain at the injection site and at the tip of the right thumb. Local therapy including injection of saline under the lesion and application of a nitroglycerine patch did not mitigate the pain at the tip of the thumb. Livedoid changes and bluish discoloration developed over the thumb tip and pyogenic granuloma [Figure - 2]. [1] Gradually, the thumb became pale and cold. He was immediately shifted to the plastic surgery department. A Doppler study confirmed reduced flow in both branches of the princeps pollicis artery, more so in the lateral one. Based on the history and clinical features, a diagnosis of Nicolau′s syndrome was made. Guided by Doppler ultrasound, 0.1 ml of 2% lignocaine was injected around both branches of the princeps pollicis. The hand was warmed and kept elevated. Intravenous dipyridamole 60 mg was administered immediately along with blood pressure monitoring. He also received subcutaneous injections of low molecular weight heparin 40 mg/day for 3 days, followed by low dose aspirin 75 mg once daily and dipyridamole 25 mg twice daily for a month. He was given oral antibiotics for a week to prevent secondary infection. The proximal half of the thumb developed cutaneous necrosis on its lateral aspect; sloughing of skin was followed by complete re-epithelialization in 6 weeks [Figure - 3]. The pyogenic granuloma over the thenar eminence also sloughed off during this period. The entire wound healed completely without sequelae except for slight cutaneous atrophy over the lateral aspect of the thumb. A slight neurological deficit in the form of stereognosis was present over the lateral thumb which improved over 10 weeks.
 |
| Figure 1: Pyogenic granuloma on right thenar eminence of palm-before treatment |
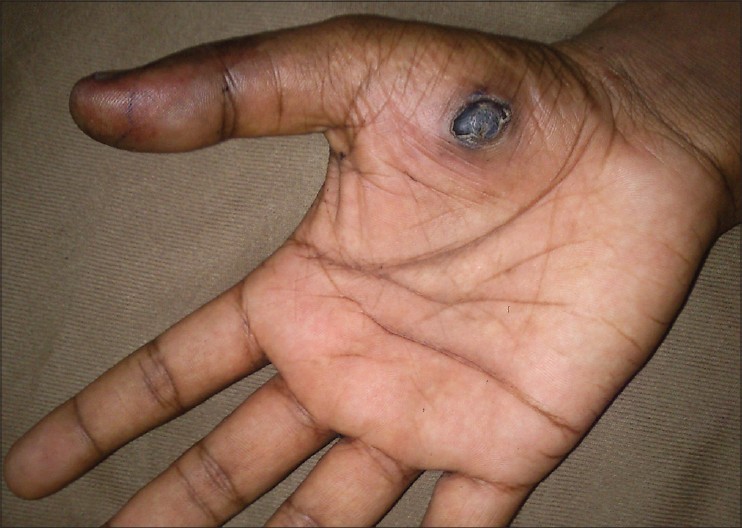 |
| Figure 2: Livedoid changes and bluish discoloration of thumb tip including discoloration of pyogenic granuloma |
 |
| Figure 3: Re-epithelization after sloughing of necrotic areas on right thumb |
Nicolau syndrome, also called embolia cutis medicamentosa, is a rare entity characterized by necrosis of the skin with a livedoid pattern. [1] It has been reported following injections of antibiotics, piroxicam, diclofenac, [2] corticosteroids, local anesthetics and sclerotherapy agents. [3] This syndrome was first described by Nicolau in 1925, when it was seen after the use of bismuth salts for treatment of syphilis. It is attributed to direct arterial embolism of the drug itself or to ischemia resulting from peri-arterial injection. Peri-arterial injection can trigger ischemia either due to compression when large volumes are injected or due to arterial vasospasm. Clinical features include the development of burning and stabbing pain after injection along with pallor, followed by bluish-red reticulate erythema and the formation of a necrotic eschar healing in a few days with an atrophic scar. [4] Diagnosis is mainly clinical; however, Doppler ultrasound studies help in assessing the occlusion of blood vessels and magnetic resonance imaging helps in delineating the extent of damage. Early institution of treatment has been reported to avert permanent ischemia and loss of digits. Conventionally, anticoagulant therapy using drugs like heparin is used to restore arterial blood supply and limit the progression of thrombosis. Additionally, we used doppler-guided peri-arterial injection of a small volume of lignocaine without adrenaline for its vasodilatory effect. Before administering peri-arterial lignocaine, it must be ensured that resuscitative equipment and drugs to treat any toxic reactions are available. Other therapies to improve vascularity in Nicolau syndrome include pentoxyphylline, hyperbaric oxygen and intravenous alprostadil. Corticosteroids have also been used to reduce inflammation. Surgical debridement may be necessary in cases of severe necrosis.
Techniques to prevent the dissipation of sclerosants beyond the desired target of action include compression along the periphery of the vascular lesion using the ring of an artery forceps, the use of a tourniquet, cyanoacrylate embolization prior to sclerotherapy or balloon embolization. [5]
Sclerotherapy is a simple and effective procedure for the treatment of pyogenic granulomas with the advantage of being an outpatient procedure, not requiring much equipment, that can be performed by a dermatologist in an office setting. Though seemingly simple, it needs to be done carefully. Nicolau syndrome is a potentially catastrophic complication. Dermatologists must be aware of this rare complication as prompt recognition prevents serious consequences.
| 1. |
Masthan SD, Salome, Madhav, Reddy KC, Sridevi, Lakshmi, et al. Nicolau syndrome. Indian J Dermatol Venereol Leprol 2002;68:45-6.
[Google Scholar]
|
| 2. |
Sarifakioglu E. Nicolau syndrome after diclofenac injection. J Eur Acad Dermatol Venereol 2007;21:266-7.
[Google Scholar]
|
| 3. |
Ramelet AA, Parmentier L. Delayed Nicolau's livedoid dermatitis after ultrasound-guided sclerotherapy. Dermatol Surg 2010;36:155-8.
[Google Scholar]
|
| 4. |
Nischal K, Basavaraj H, Swaroop M, Agrawal D, Sathyanarayana B, Umashankar N. Nicolau syndrome: An iatrogenic cutaneous necrosis. J Cutan Aesthet Surg 2009;2:92-5.
[Google Scholar]
|
| 5. |
Khandpur S. Sclerotherapy for vascular malformations. In: Venkatram M, editor. ACS(I) Textbook on Cutaneous and Aesthetic Surgery. New Delhi: Jaypee Brothers Medical Publishers; 2012. p. 463-71.
[Google Scholar]
|
Fulltext Views
3,987
PDF downloads
2,405





