Translate this page into:
Non-eczematous lichenoid contact cheilitis: A rare presentation
Corresponding author: Dr. Biswanath Behera, Department of Dermatology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. biswanthbehera61@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Garg S, Behera B, Priyadharsan B, Gowda SK, Sethy M. Non-eczematous lichenoid contact cheilitis: A rare presentation. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1660_2024
Dear Editor,
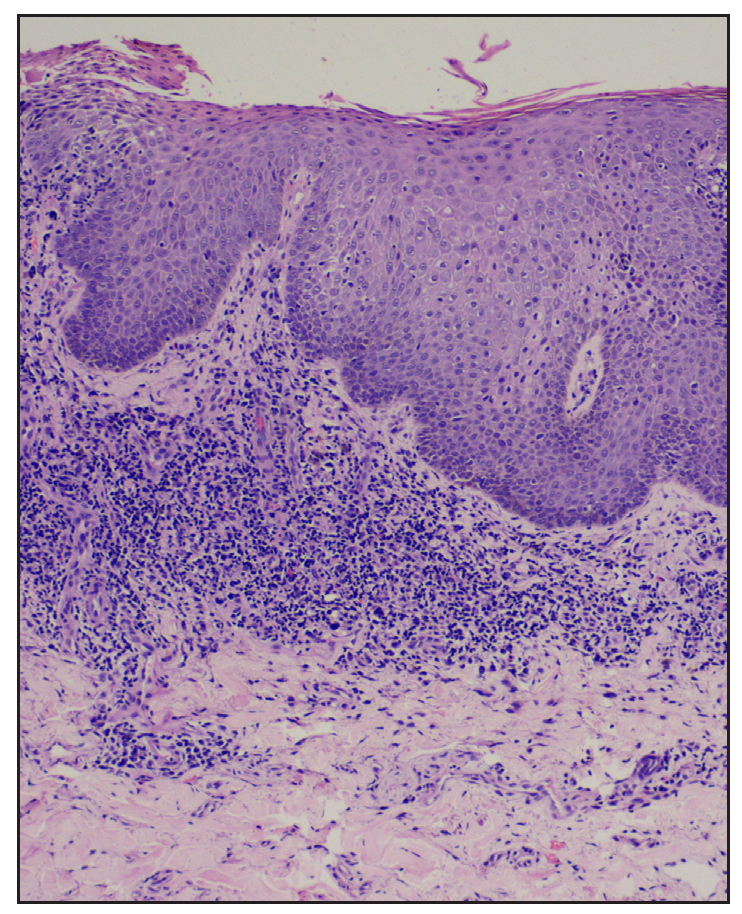
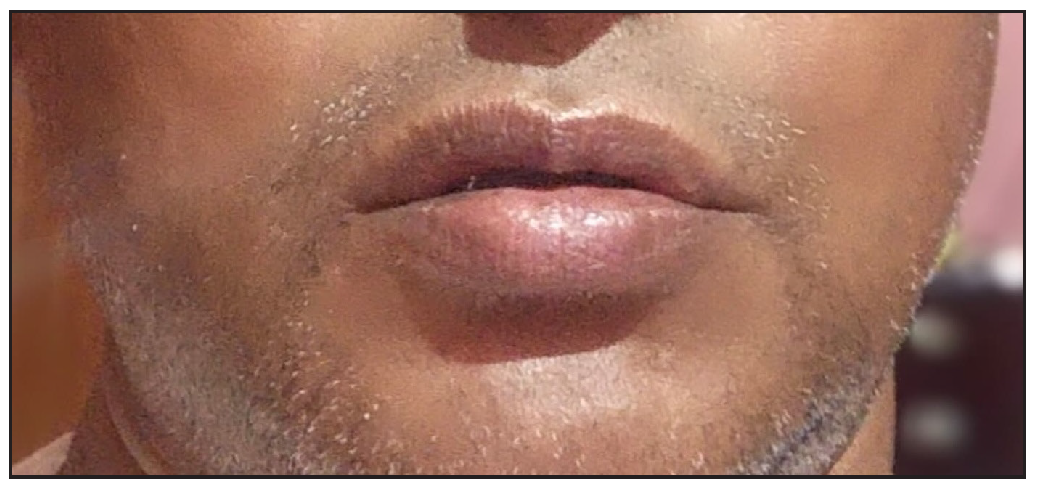
A 50-year-old non-diabetic, non-hypertensive man presented with recurrent elevated lip lesions for two months. It was associated with mild itching without any oozing. He reported using black-coloured dye (containing paraphenylenediamine, PPD) on scalp hair for five years and on the moustache hair for two months. Initially, he used to experience itching, followed by the development of itchy, reddish, and pigmented lesions on the lips. The patient had a history of similar red elevated scaly lesions associated with itching over the scalp after using hair dye. Because of the scalp lesions, the patient stopped using hair dye on that area. It was not associated with any breathing difficulty or eyelid oedema. He denied the use of lip cosmetics, smoking, chewing tobacco, or any oral medications. The lesions used to improve with the use of topical steroids. Examination showed multiple erythematous to reddish-grey flat-topped papules and plaques on the vermilion of both lips, which were associated with erosion and crusting. In addition, a similar lesion was present on the upper lip. The lip angles were spared [Figure 1]. Examination showed that the oral cavity and the rest of the mucocutaneous regions were spared too. The possibility of lichen planus cheilitis and lichenoid contact cheilitis was considered. Dermoscopy revealed scale-crust, erosions, and reddish-grey structureless areas [Figure 2a]. Patch testing with Indian standard and cosmetic series showed positivity for paraphenylenediamine (2+, PPD). Histopathological examination showed an acanthotic epidermis with focal parakeratosis, mild spongiosis, lymphocytic exocytosis, basal cell vacuolisation, and a dense band of lichenoid infiltrate consistent with the lichenoid eruption [Figure 2b]. Based on these findings, a final diagnosis of lichenoid contact cheilitis (LCD) secondary to PPD-containing hair dye was made. The patient was advised to stop using the PPD-containing hair dye. Application of a topical mometasone furoate 0.1% cream twice daily was prescribed for two weeks [Figure 3], leading to complete subsidence of the lesion without any recurrence at the six-month follow-up.

- Multiple erythematous to reddish-grey flat-topped small papules with erosions and crusting.

- Dermoscopy shows scale-crust, erosions, and reddish-grey structureless areas (non polarised, 10x).
- Histopathology shows an acanthotic epidermis with focal parakeratosis, mild spongiosis, exocytosis, basal cell vacuolisation, and a dense band of lichenoid infiltrate consistent with the lichenoid eruption (Haematoxylin & eosin, 400x).
- Complete subsidence of lesions post therapy.
Cheilitis, a common entity encountered in day-to-day clinical practice, can be due to a multitude of causes. Many agents can cause contact cheilitis (CC). Clinically, it can be eczematous or non-eczematous. Non-eczematous contact dermatitis is a rare subtype of contact dermatitis with varied clinical morphology. The various non-eczematous contact dermatitis described are erythema multiforme-like, purpuric, pigmented, lichenoid, lymphomatoid, pustular, and dyshidrosiform contact dermatitis.1 PPD-containing hair dyes and PPD-derived colour are well known to cause lichenoid contact cheilitis (LCC). Other reported causative agents are nickel, copper, arsenic, mercury, gold, Primula obconica, epoxy resins, aminoglycoside antibiotics, and methacrylic acid esters.2,3
Lichenoid contact cheilitis can be mistaken for lichen planus, especially in skin of colour, as both present as violaceous or reddish-lilac papules and plaques. Table 1 summarises the differences between lichen planus and LCD.1 A history of contact with a positive patch test for the concerned allergen can help differentiate between the two conditions. Histopathological examination can closely resemble lichen planus. However, lichen planus shows wedge-shaped hypergranulosis, prominent basal vacuolar degeneration, Civatte bodies, and band-like subepidermal lymphocytic infiltration obscuring the dermo-epidermal junction. In addition, spongiosis is not a feature of LP.1
| Criteria | LCD | LP |
|---|---|---|
| Spongiosis | ++ | - |
| Hypergranulosis | -/+ | +++ |
| Basal cell vacuolar degeneration | + | +++ |
| Pigment incontinence | + | +++ |
| Civatte bodies | - | ++ |
| Dermal papillae | Lengthened | Broad, dome shape |
| Inflammatory infiltrate (lymphohistiocytic) | Perivascular and mild | Band-like |
+: present, -: absent
A rare variant of non-eczematous contact cheilitis, called pigmented contact cheilitis, has been described as caused by using lipsticks. The various types of allergens implicated in different kinds of non-eczematous contact dermatitis have been tabulated in Table 2.1-5 Paraphenylenediamine is known to cause lichenoid, pigmented, pustular, purpuric, lymphomatous, and dyshidrosiform types of non-eczematous contact dermatitis.1
| Type of reaction | Substance | Allergens |
|---|---|---|
| Erythema multiforme-like | Plants and woods | Dalbergia nigra (Brazilian rosewood), Pau ferro (Machaerium scleroxylon), Eucalyptus saligna, Artemisia vulgaris, poison ivy |
| Medicaments | Ethylenediamine, pyrrolnitrin, sulfamide, econazole, and balsam of Peru | |
| Others | Brominated compounds, phenyl sulphone derivatives, and epoxy resin | |
| Purpuric contact dermatitis | Rubber compounds | N-isopropyl-N-phenyl-paraphenylenediamine and mercaptobenzothiazole |
| Textile compounds | Optical whiteners (Tinopal CH 3566) and azoic dyes | |
| Plants | Agave americana L, Zea mais, Frullania | |
| Pigmented contact dermatitis | Dyes | Naphthol AS, Sudan I, and paraphenylenediamine |
| Cosmetics | Pigments: Pigment orange 3, pigment red 3 and pigment red 49 | |
| Fragrances | Jasmine and Hydroxycitronellal | |
| Antiseptics | Carbanilide | |
| Others | Formaldehyde, nickel, and rubber | |
| Lymphomatoid | Dyes | Paraphenylenediamine, |
| Metals | Nickel and gold | |
| Others | para-tertiary butyl-phenol resin, and ethylenediamine | |
| Pustular | Trichloroethylene, minoxidil | |
| Metals | Nickel, copper, arsenic, and mercury, and potassium dichromate | |
| Dyshidrosiform | Topical medications | |
| Dyes | Paraphenylenediamine (PPD) | |
| Metals | Nickel, cobalt, mercury | |
| Others | Para tertiary butyl phenol and formaldehyde resin | |
| Lichenoid | Dyes | Para- phenylenediamine, |
| Metals | Nickel, copper, zinc, and mercury | |
| Others | Epoxy resins, antibiotics, methacrylic acid esters, and methylisothiazolinone |
In conclusion, we report a rare lichenoid contact cheilitis secondary to PPD and highlight the importance of recognising the same to avoid misdiagnosis and conduct appropriate management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Noneczematous contact dermatitis. ISRN Allergy. 2013;2013:361746.
- [CrossRef] [PubMed] [Google Scholar]
- Para-phenylenediamine-induced lichenoid eruptions. Contact Dermatitis. 1999;41:40-1.
- [CrossRef] [PubMed] [Google Scholar]
- Lichenoid contact dermatitis secondary to methylisothiazolinone (MI) JAAD Case Rep. 2016;2:380-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lichenoid lesions of the upper lip: A retrospective study of 24 cases. Med. Oral Patol. Oral Cir. Bucal. 2018;23:e302-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A sudden flare-up of a quiescent oral lichen planus: Methylisothiazolinone as the prime suspect? Contact Dermatitis. 2015;72:186-9.
- [CrossRef] [PubMed] [Google Scholar]





