Translate this page into:
Non-healing cutaneous ulcer as the initial presentation of disseminated cryptococcosis
Corresponding Author: Dr. Priya Prathap, Department of Dermatology and Venereology, Government Medical College, Thrissur, M.G.Kavu, Thrissur, 680596, Kerala, India. priya.anil.an@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Premjith TJ, Prathap P, Asokan N, Balakrishnan S. Non-healing cutaneous ulcer as the initial presentation of disseminated cryptococcosis. Indian J Dermatol Venereol Leprol 2022;88:873.
Sir,
Cutaneous cryptococcosis exists in two clinical forms.1 The localized type of cutaneous cryptococcosis, namely primary cutaneous cryptococcosis, is more frequent in immunocompetent individuals. Immuno-compromised patients may have disseminated skin lesions, from a systemic focus. We report a case of non-healing cutaneous ulcer as the initial presentation in an immunocompromised patient with disseminated cryptococcosis.
A 40-year-old female, a manual labourer, residing in a rural area, developed an ulcer on her right thumb three months ago. She had a thorn prick at the site, two weeks prior to the onset of the ulcer. There was an inadequate response to treatment with several courses of antibiotics from nearby hospitals. After three months she attended our hospital for continuous fever, headache, vomiting and neck stiffness for the previous two weeks. On examination, the ulcer on the right thumb was of 1.5 × 1 cm size, irregular borders and necrotic floor [Figure 1]. Sensations were preserved on the thumb. The surrounding skin was indurated and tender. Right axillary lymph nodes were enlarged (1.5 × 1 cm), mobile, non-tender and non-matted. Peripheral nerves were normal. Clinical differentials considered for the ulcer on the thumb were deep fungal infections, Hansen’s disease, tuberculous chancre and atypical mycobacterial infection.

- Necrotic ulcer on right thumb
Blood haemoglobin was 7.5 mg/dl, total leucocyte count was 2800 cells/mm3 with differential count of P93L2M5 and ESR was 104 mm/1st hour. Peripheral blood smear showed microcytic anaemia. Ear lobe smear was negative for mycobacterium leprae. She was detected to be positive for human immunodeficiency virus (HIV). Immuno comb, tri dot test and liquid phase enzyme-linked immunosorbent assay (ELISA) were done. CD4 cell count was 25 cells/mm3. Cerebrospinal fluid (CSF) examination following lumbar puncture showed scanty pus cells, no growth of bacteria on culture, negative for tuberculous bacilli on catridge-based nucleic acid amplification test (CBNAAT), but positive for cryptococcal antigen by ELISA. Chest x-ray showed right upper lobe consolidation. Sputum culture grew Klebsiella. USG abdomen detected a small haemangioma in the liver. Computerised tomography (CT) and magnetic resonance imaging (MRI) of the brain were normal.
Histopathology of the ulcer showed capsulated organisms in dermis, [Figures 2a and b] enhanced by mucicarmine, Gomori methenamine silver and periodic acid Schiff stains, suggestive of cryptococcus [Figures 2c to h]. Fine needle aspiration cytology (FNAC) from axillary lymph node showed cryptococci [Figure 3].
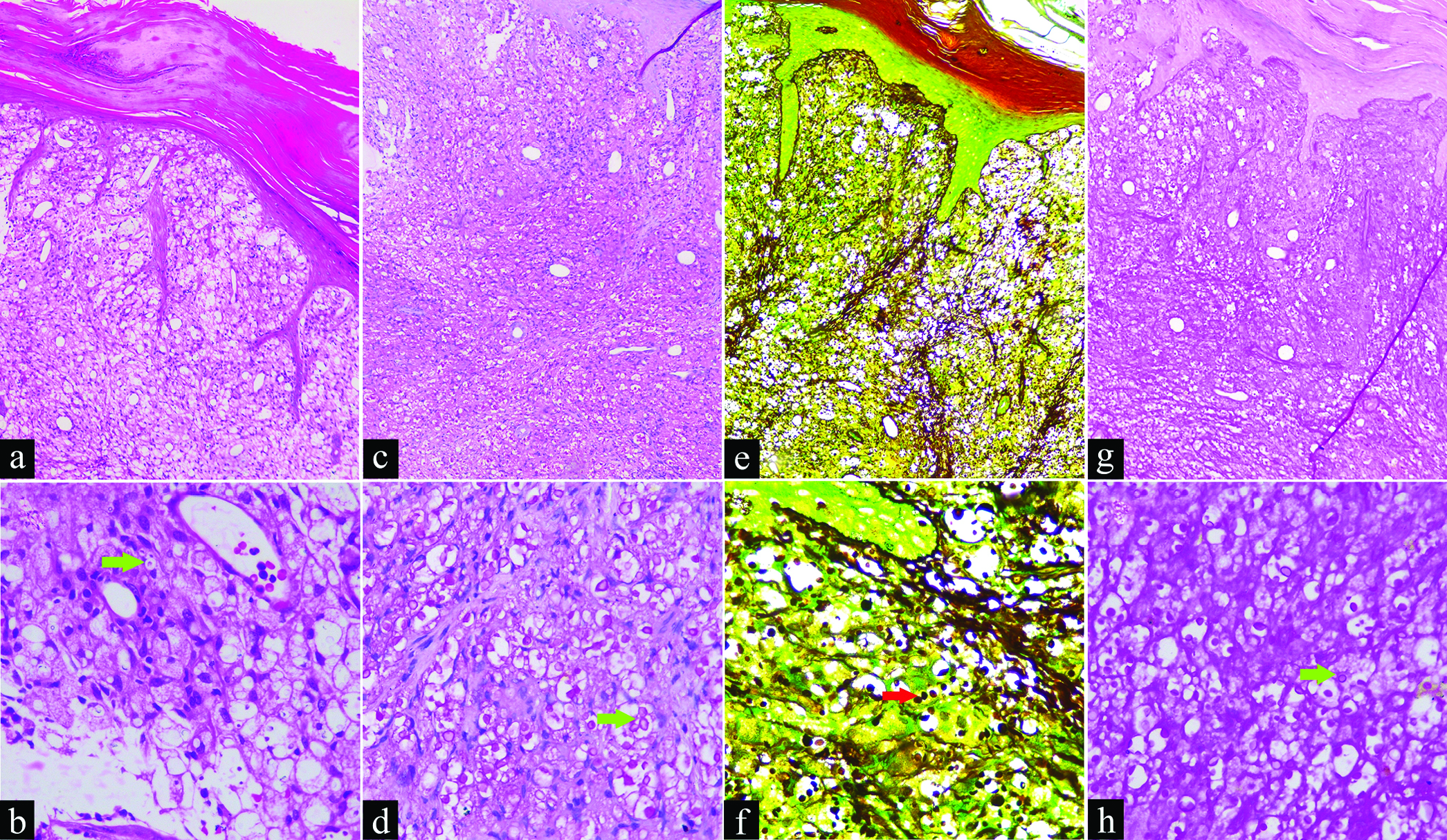
- (a) Edge of ulcer showing hyperkeratosis, parakeratosis, dermal edema with mixed inflammatory infiltrates and many spores within and outside histiocytes (H&E, × 100); (b) High power view (green arrow) showing yeast forms–extracellular and within the histiocytes (H&E, × 400); (c and d) Red spores (Mucicarmine stain, × 100 & × 400); (e and f) (red arrow) Black spores (Gomori methenamine silver stain, × 100 & × 400); (g and h) (green arrow) Purple staining of cryptococcus and unstained capsule (Periodic acid-Schiff stain, × 100 & × 400)
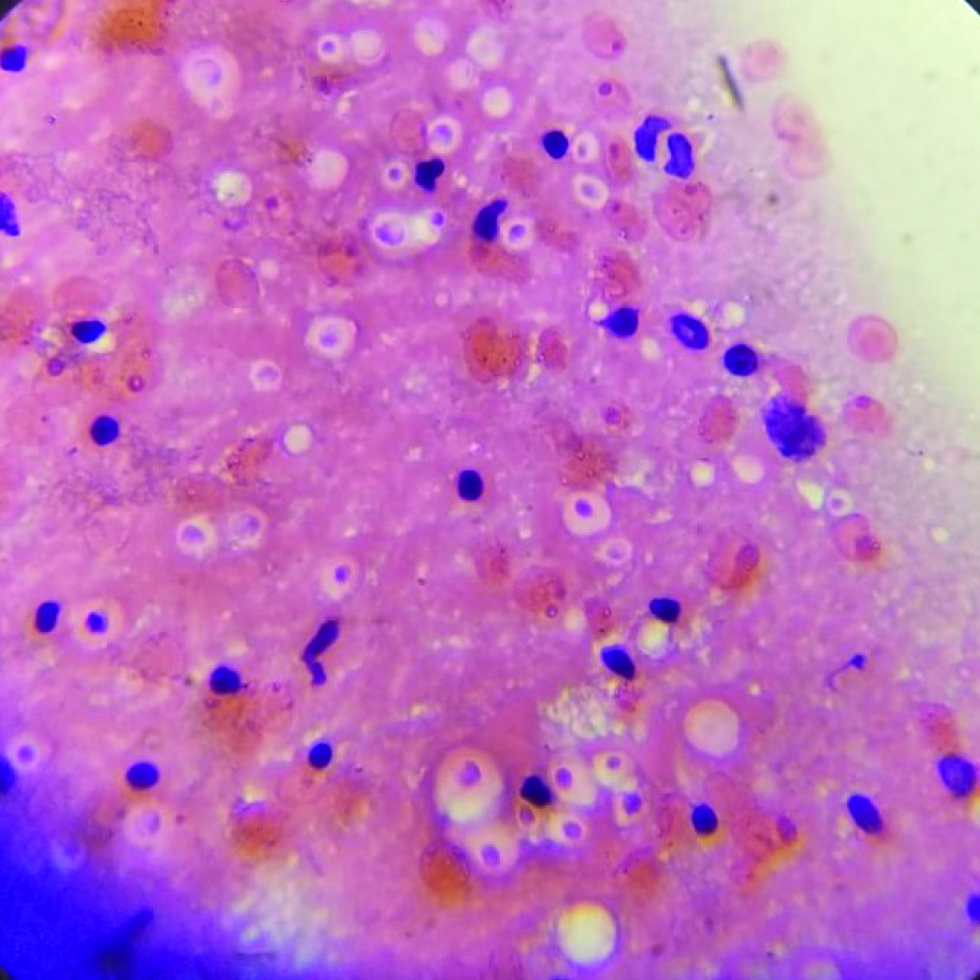
- Fine needle aspiration cytology from cervical lymph showing refractile round structures (H&E, 400×)
The natural course of the disease, clinical features and histopathology suggested a diagnosis of disseminated cryptococcosis. Following current World Health Organization (WHO) guidelines, she was treated with injection amphotericin B 1 mg/kg for two weeks, followed by tab fluconazole 800 mg/day for two months.2 Anti-retroviral therapy with tenofovir, lamivudine and efavirenz and cotrimoxazole prophylaxis for Pneumocystis jiroveci were also started. Within two weeks she recovered from meningitis and within six weeks, the ulcer healed [Figure 4]. Tab fluconazole 200 mg/day was continued for six months.

- Post-treatment picture
Cryptococcus neoformans is a capsulated saprophytic basidiomycete, which is abundant in soil having bird droppings. Important sub-species are grubii (A) and neoformans (D) which are seen in soil and gattii (B, C) found in red gum trees. The usual mode of entry into the body is by aerosol inhalation and the primary disease is usually pulmonary.3 Less commonly it can invade the skin through trauma and contact with avian excreta and result in primary cutaneous cryptococcosis.1 Skin lesions in cutaneous cryptococcosis are cysts, acneiform papules, pustules, nodules, molluscum contagiosum like umbilicated lesions and necrotizing fasciitis.4
Systemic dissemination from primary cutaneous cryptococcosis is extremely rare. In a series of 22 cases of primary cutaneous cryptococcosis described by Neuville et al. one patient co-infected with HIV had cryptococcal antigens in CSF.5 But there was no mention of clinically manifested meningitis in that patient.
Our case underlines the need for including cutaneous cryptococcosis in the differential diagnosis of patients, especially from a rural and agricultural background, presenting with non-healing traumatic ulcers. Our case also highlights the need to evaluate such a patient for systemic dissemination, especially if the patient is immune-compromised. Early recognition of this disease can be life-saving.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Primary cutaneous cryptococcosis due to cryptococcus neoformans in an immunocompetent host treated with itraconazole and drainage: Case report and review of the literature. Case Rep Dermatol. 2021;13:89-97.
- [CrossRef] [PubMed] [Google Scholar]
- WHO. Guidelines for the diagnosis, prevention and management of cryptococcal disease in HIV-infected adults, adolescents and children. Supplement to the 2016 consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. [Online]. Available from: https://www.who.int/hiv/pub/guidelines/cryptococcal-disease/en/ [Accessed 10 February 2021].
- [Google Scholar]
- Cutaneous cryptococcosis: An underlying immunosuppression? Clinical manifestations, pathogenesis, diagnostic examinations and treatment. Postepy Dermatol Alergol. 2020;37:154-8.
- [CrossRef] [PubMed] [Google Scholar]
- Primary cutaneous cryptococcosis: An unusual injection site infection. Case Rep Dermatol. 2020;12:138-43.
- [CrossRef] [PubMed] [Google Scholar]
- Primary cutaneous cryptococcosis: A distinct clinical entity. Clinical Infectious Diseases. 2003;36:337-47.
- [CrossRef] [PubMed] [Google Scholar]





